Glycosaminoglycan Analysis of FFPE Tissues from Prostate Cancer and Benign Prostate Hyperplasia Patients Reveals Altered Regulatory Functions and Independent Markers for Survival
Abstract
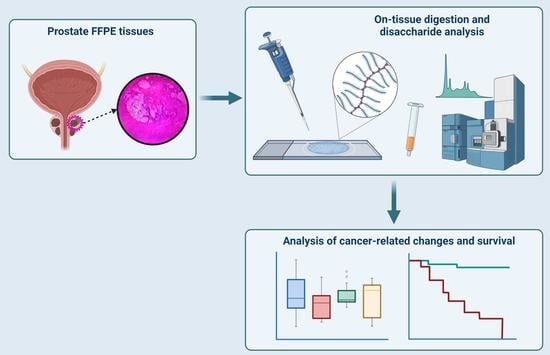
:Simple Summary
Abstract
1. Introduction
2. Materials and Methods
2.1. Chemicals and Reagents
2.2. Patients Selection
2.3. FFPE Tissue Preparation
2.4. High-Performance Liquid Chromatography–Mass Spectrometry
2.5. Statistical Analysis, Data Visualization
3. Results
3.1. Total Abundance of Chondroitin Sulfate and Heparan Sulfate
3.2. Sulfation Motifs of Chondroitin Sulfate
3.3. Sulfation Motifs of Heparan Sulfate
3.4. Survival Analysis
3.5. Independence of GAG Motifs from Currently Used Clinical Parameters
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Appendix A




References
- Sung, H.; Ferlay, J.; Siegel, R.L.; Laversanne, M.; Soerjomataram, I.; Jemal, A.; Bray, F. Global Cancer Statistics 2020: GLOBOCAN Estimates of Incidence and Mortality Worldwide for 36 Cancers in 185 Countries. CA Cancer J. Clin. 2021, 71, 209–249. [Google Scholar] [CrossRef] [PubMed]
- Parker, C.; Castro, E.; Fizazi, K.; Heidenreich, A.; Ost, P.; Procopio, G.; Tombal, B.; Gillessen, S. Prostate cancer: ESMO Clinical Practice Guidelines for diagnosis, treatment and follow-up. Ann. Oncol. 2020, 31, 1119–1134. [Google Scholar] [CrossRef] [PubMed]
- Meghan, A.R.; Tanya, S. Biomarkers for Diagnosis and Prognosis of Prostate Cancer; IntechOpen: London, UK, 2019. [Google Scholar] [CrossRef] [Green Version]
- Rodrigues, G.; Warde, P.; Pickles, T.; Crook, F.J.; Brundage, M.; Souhami, L.; Lukka, H.; Genitourinary Radiation Oncologists of Canada. Pre-treatment risk stratification of prostate cancer patients: A critical review. Can. Urol. Assoc. J. 2012, 6, 121–127. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Lokshin, A.; Mikhaleva, L.M.; Goufman, E.I.; Boltovskaya, M.N.; Tikhonova, N.B.; Stepanova, I.I.; Stepanov, A.A.; Potoldykova, N.V.; Vinarov, A.Z.; Stemmer, P.; et al. Proteolyzed Variant of IgG with Free C-Terminal Lysine as a Biomarker of Prostate Cancer. Biology 2021, 10, 817. [Google Scholar] [CrossRef] [PubMed]
- Lindahl, U.; Couchman, J.; Kimata, K.; Esko, J.D. Proteoglycans and Sulfated Glycosaminoglycans. In Essentials of Glycobiology, 3rd ed.; Varki, A., Cummings, R.D., Esko, J.D., Stanley, P., Hart, G.W., Aebi, M., Darvill, A.G., Kinoshita, T., Packer, N.H., Eds.; Cold Spring Harbor Laboratory Press: Cold Spring Harbor, NY, USA, 2015; pp. 207–221. [Google Scholar] [CrossRef]
- Kreuger, J.; Kjellén, L. Heparan Sulfate Biosynthesis. J. Histochem. Cytochem. 2012, 60, 898–907. [Google Scholar] [CrossRef] [Green Version]
- Gibbs, R.V. Cytokines and Glycosaminoglycans (GAGS). Glycobiol. Medicine 2003, 535, 125–143. [Google Scholar] [CrossRef]
- Kjellén, L.; Lindahl, U. Specificity of glycosaminoglycan–protein interactions. Curr. Opin. Struct. Biol. 2018, 50, 101–108. [Google Scholar] [CrossRef]
- Raman, R.; Sasisekharan, V.; Sasisekharan, R. Structural Insights into Biological Roles of Protein-Glycosaminoglycan Interactions. Chem. Biol. 2005, 12, 267–277. [Google Scholar] [CrossRef]
- Tóth, G.; Pál, D.; Sugár, S.; Kovalszky, I.; Dezső, K.; Schlosser, G.; Drahos, L.; Turiák, L. Expression of glycosaminoglycans in cirrhotic liver and hepatocellular carcinoma—a pilot study including etiology. Anal. Bioanal. Chem. 2022, 1–10. [Google Scholar] [CrossRef]
- Turiák, L.; Shao, C.; Meng, L.; Khatri, K.; Leymarie, N.; Wang, Q.; Pantazopoulos, H.; Leon, D.R.; Zaia, J. Workflow for Combined Proteomics and Glycomics Profiling from Histological Tissues. Anal. Chem. 2014, 86, 9670–9678. [Google Scholar] [CrossRef] [Green Version]
- Turiák, L.; Tóth, G.; Ozohanics, O.; Révész, Á.; Ács, A.; Vékey, K.; Zaia, J.; Drahos, L. Sensitive method for glycosaminoglycan analysis of tissue sections. J. Chromatogr. A 2018, 1544, 41–48. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Sanderson, R.D.; Yang, Y.; Purushothaman, A.; Khotskaya, Y.B.; Ritchie, J.P.; Ramani, V.C. Proteoglycans and Cancer. In Cell-Extracellular Matrix Interactions in Cancer; Zent, R., Pozzi, A., Eds.; Springer: New York, NY, USA, 2010; pp. 191–215. [Google Scholar] [CrossRef]
- Edwards, I.J. Proteoglycans in prostate cancer. Nat. Rev. Urol. 2012, 9, 196–206. [Google Scholar] [CrossRef] [PubMed]
- Turiák, L.; Ozohanics, O.; Tóth, G.; Ács, A.; Révész, Á.; Vékey, K.; Telekes, A.; Drahos, L. High sensitivity proteomics of prostate cancer tissue microarrays to discriminate between healthy and cancerous tissue. J. Proteom. 2018, 197, 82–91. [Google Scholar] [CrossRef] [PubMed]
- Tóth, G.; Vékey, K.; Drahos, L.; Horváth, V.; Turiák, L. Salt and solvent effects in the microscale chromatographic separation of heparan sulfate disaccharides. J. Chromatogr. A 2019, 1610, 460548. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Tóth, G.; Vékey, K.; Sugár, S.; Kovalszky, I.; Drahos, L.; Turiák, L. Salt gradient chromatographic separation of chondroitin sulfate disaccharides. J. Chromatogr. A 2020, 1619, 460979. [Google Scholar] [CrossRef] [PubMed]
- Ihaka, R.; Gentleman, R. R: A Language for Data Analysis and Graphics. J. Comput. Graph. Stat. 1996, 5, 299–314. [Google Scholar] [CrossRef]
- Wickham, H. Data Analysis. In ggplot2: Elegant Graphics for Data Analysis; Wickham, H., Ed.; Springer International Publishing: New York, NY, USA, 2016; pp. 189–201. [Google Scholar] [CrossRef]
- Lánczky, A.; Győrffy, B. Web-Based Survival Analysis Tool Tailored for Medical Research (KMplot): Development and Implementation. J. Med. Internet Res. 2021, 23, e27633. [Google Scholar] [CrossRef]
- Goulas, A.; Hatzichristou, D.G.; Karakiulakis, G.; Mirtsou-Fidani, V.; Kalinderis, A.; Papakonstantinou, E. Benign hyperplasia of the human prostate is associated with tissue enrichment in chondroitin sulphate of wide size distribution. Prostate 2000, 44, 104–110. [Google Scholar] [CrossRef]
- Liu, C.-H.; Lan, C.-T.; Chou, J.-F.; Tseng, T.-J.; Liao, W.-C. CHSY1 promotes aggressive phenotypes of hepatocellular carcinoma cells via activation of the hedgehog signaling pathway. Cancer Lett. 2017, 403, 280–288. [Google Scholar] [CrossRef]
- Momose, T.; Yoshimura, Y.; Harumiya, S.; Isobe, K.; Kito, M.; Fukushima, M.; Kato, H.; Nakayama, J. Chondroitin sulfate synthase 1 expression is associated with malignant potential of soft tissue sarcomas with myxoid substance. Hum. Pathol. 2016, 50, 15–23. [Google Scholar] [CrossRef] [Green Version]
- Ricciardelli, C.; Mayne, K.; Sykes, P.; Raymond, W.; McCaul, K.; Marshall, V.R.; Tilley, W.; Skinner, J.M.; Horsfall, D.J. Elevated stromal chondroitin sulfate glycosaminoglycan predicts progression in early-stage prostate cancer. Clin. Cancer Res. 1997, 3, 983–992. [Google Scholar]
- Ricciardelli, C.; Quinn, D.; Raymond, W.; McCaul, K.; Sutherland, P.D.; Stricker, P.D.; Grygiel, J.J.; Sutherland, R.L.; Marshall, V.R.; Tilley, W.; et al. Elevated levels of peritumoral chondroitin sulfate are predictive of poor prognosis in patients treated by radical prostatectomy for early-stage prostate cancer. Cancer Res. 1999, 59, 2324–2328. [Google Scholar]
- Ricciardelli, C.; Mayne, K.; Sykes, P.; Raymond, W.; McCaul, K.; Marshall, V.R.; Horsfall, D.J. Elevated levels of versican but not decorin predict disease progression in early-stage prostate cancer. Clin. Cancer Res. 1998, 4, 963–971. [Google Scholar]
- Iida, S.; Suzuki, K.; Matsuoka, K.; Takazono, I.; Shimada, A.; Inoue, M.; Yahara, J.; Noda, S. Analysis of glycosaminoglycans in human prostate by high-performance liquid chromatography. Br. J. Urol. 1997, 79, 763–769. [Google Scholar] [CrossRef]
- Pudełko, A.; Wisowski, G.; Olczyk, K.; Koźma, E.M. The dual role of the glycosaminoglycan chondroitin-6-sulfate in the development, progression and metastasis of cancer. FEBS J. 2019, 286, 1815–1837. [Google Scholar] [CrossRef] [Green Version]
- Mikami, T.; Kitagawa, H. Biosynthesis and function of chondroitin sulfate. Biochim. Et Biophys. Acta (BBA) Gen. Subj. 2013, 1830, 4719–4733. [Google Scholar] [CrossRef]
- Benito-Arenas, R.; Doncel-Pérez, E.; Fernández-Gutiérrez, M.; Garrido, L.; García-Junceda, E.; Revuelta, J.; Bastida, A.; Fernández-Mayoralas, A. A holistic approach to unravelling chondroitin sulfation: Correlations between surface charge, structure and binding to growth factors. Carbohydr. Polym. 2018, 202, 211–218. [Google Scholar] [CrossRef]
- da Cunha, A.L.; Aguiar, J.A.; da Silva, F.S.C.; Michelacci, Y.M. Do chondroitin sulfates with different structures have different activities on chondrocytes and macrophages? Int. J. Biol. Macromol. 2017, 103, 1019–1031. [Google Scholar] [CrossRef]
- Tan, G.-K.; Tabata, Y. Chondroitin-6-sulfate attenuates inflammatory responses in murine macrophages via suppression of NF-κB nuclear translocation. Acta Biomater. 2014, 10, 2684–2692. [Google Scholar] [CrossRef]
- Hagerling, C.; Casbon, A.-J.; Werb, Z. Balancing the innate immune system in tumor development. Trends Cell Biol. 2014, 25, 214–220. [Google Scholar] [CrossRef] [Green Version]
- Theocharis, A.D.; Skandalis, S.S.; Tzanakakis, G.N.; Karamanos, N.K. Proteoglycans in health and disease: Novel roles for proteoglycans in malignancy and their pharmacological targeting. FEBS J. 2010, 277, 3904–3923. [Google Scholar] [CrossRef] [PubMed]
- Ricciardelli, C.; Sakko, A.J.; Ween, M.P.; Russell, D.L.; Horsfall, D.J. The biological role and regulation of versican levels in cancer. Cancer Metastasis Rev. 2009, 28, 233–245. [Google Scholar] [CrossRef] [PubMed]
- Wu, Y.J.; La Pierre, D.P.; Wu, J.; Yee, A.J.; Yang, B.B. The interaction of versican with its binding partners. Cell Res. 2005, 15, 483–494. [Google Scholar] [CrossRef] [PubMed]
- Hirose, J.; Kawashima, H.; Yoshie, O.; Tashiro, K.; Miyasaka, M. Versican Interacts with Chemokines and Modulates Cellular Responses. J. Biol. Chem. 2001, 276, 5228–5234. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ricciardelli, C.; Russell, D.L.; Ween, M.; Mayne, K.; Suwiwat, S.; Byers, S.; Marshall, V.R.; Tilley, W.; Horsfall, D.J. Formation of Hyaluronan- and Versican-rich Pericellular Matrix by Prostate Cancer Cells Promotes Cell Motility. J. Biol. Chem. 2007, 282, 10814–10825. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Hu, Y.; Sun, H.; Owens, R.T.; Wu, J.; Chen, Y.Q.; Berquin, I.M.; Perry, D.; O’Flaherty, J.T.; Edwards, I.J. Decorin Suppresses Prostate Tumor Growth through Inhibition of Epidermal Growth Factor and Androgen Receptor Pathways. Neoplasia 2009, 11, 1042–1053. [Google Scholar] [CrossRef] [Green Version]
- Schaefer, L.; Schaefer, R.M. Proteoglycans: From structural compounds to signaling molecules. Cell Tissue Res. 2009, 339, 237–246. [Google Scholar] [CrossRef]
- Nakamura, N.; Kojima, J. Changes in charge density of heparan sulfate isolated from cancerous human liver tissue. Cancer Res. 1981, 41, 278–283. [Google Scholar]
- Tátrai, P.; Egedi, K.; Somorácz, Á.; van Kuppevelt, T.H.; Dam, G.T.; Lyon, M.; Deakin, J.A.; Kiss, A.; Schaff, Z.; Kovalszky, I. Quantitative and Qualitative Alterations of Heparan Sulfate in Fibrogenic Liver Diseases and Hepatocellular Cancer. J. Histochem. Cytochem. 2010, 58, 429–441. [Google Scholar] [CrossRef] [Green Version]
- Carlsson, P.; Presto, J.; Spillmann, D.; Lindahl, U.; Kjellén, L. Heparin/Heparan Sulfate Biosynthesis. J. Biol. Chem. 2008, 283, 20008–20014. [Google Scholar] [CrossRef]
- Sheng, J.; Liu, R.; Xu, Y.; Liu, J. The Dominating Role of N-Deacetylase/N-Sulfotransferase 1 in Forming Domain Structures in Heparan Sulfate. J. Biol. Chem. 2011, 286, 19768–19776. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Presto, J.; Thuveson, M.; Carlsson, P.; Busse, M.; Wilén, M.; Eriksson, I.; Kusche-Gullberg, M.; Kjellén, L. Heparan sulfate biosynthesis enzymes EXT1 and EXT2 affect NDST1 expression and heparan sulfate sulfation. Proc. Natl. Acad. Sci. USA 2008, 105, 4751–4756. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Santos, N.J.; Barquilha, C.N.; Barbosa, I.C.; Macedo, R.T.; Lima, F.O.; Justulin, L.A.; Barbosa, G.O.; Carvalho, H.F.; Felisbino, S.L. Syndecan Family Gene and Protein Expression and Their Prognostic Values for Prostate Cancer. Int. J. Mol. Sci. 2021, 22, 8669. [Google Scholar] [CrossRef] [PubMed]
- Szatmári, T.; Ötvös, R.; Hjerpe, A.; Dobra, K. Syndecan-1 in Cancer: Implications for Cell Signaling, Differentiation, and Prognostication. Dis. Markers 2015, 2015, 1–13. [Google Scholar] [CrossRef] [Green Version]
- Szarvas, T.; Reis, H.; Dorp, F.V.; Tschirdewahn, S.; Niedworok, C.; Nyirady, P.; Schmid, K.W.; Rübben, H.; Kovalszky, I. Soluble syndecan-1 (SDC1) serum level as an independent pre-operative predictor of cancer-specific survival in prostate cancer. Prostate 2016, 76, 977–985. [Google Scholar] [CrossRef]
- Szarvas, T.; Sevcenco, S.; Módos, O.; Keresztes, D.; Nyirády, P.; Kubik, A.; Romics, M.; Kovalszky, I.; Reis, H.; Hadaschik, B.; et al. Circulating syndecan-1 is associated with chemotherapy-resistance in castration-resistant prostate cancer. Urol. Oncol. Semin. Orig. Investig. 2018, 36, 312.e9–312.e15. [Google Scholar] [CrossRef]
- Brimo, F.; Vollmer, R.T.; Friszt, M.; Corcos, J.; Bismar, T.A. Syndecan-1 expression in prostate cancer and its value as biomarker for disease progression. Br. J. Urol. 2009, 106, 418–423. [Google Scholar] [CrossRef]
- Watanabe, Y.; Aoki-Kinoshita, K.F.; Ishihama, Y.; Okuda, S. GlycoPOST realizes FAIR principles for glycomics mass spectrometry data. Nucleic Acids Res. 2020, 49, D1523–D1528. [Google Scholar] [CrossRef]






| Total HS | D2S0/D0S6 | D2S6 | D0a10 | 6S-CS/4S-CS Ratio | ||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Clinical Parameter | p-Value | HR | p-Value | HR | p-Value | HR | p-Value | HR | p-Value | HR |
| T-stage | 0.0573 | 0.36 (0.13–1.00) | 0.0252 | 3.97 (1.32–11.92) | 0.0152 | 4.63 (1.59–13.54) | 0.0525 | 3.30 (1.23–8.85) | 0.1807 | 0.40 (0.13–1.27) |
| PSA level | 0.1595 | 0.45 (0.15–1.37) | 0.032 | 3.43 (1.20–9.82) | 0.0252 | 3.90 (1.34–11.29) | 0.1807 | 2.31 (0.84–6.37) | 0.2294 | 0.50 (0.16–1.56) |
| ISUP grade | 0.0456 | 0.33 (0.12–0.93) | 0.0151 | 5.17 (1.73–15.51) | 0.0026 | 8.72 (2.70–28.16) | 0.0525 | 3.45 (1.31–9.04) | 0.2063 | 0.45 (0.15–1.41) |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Tóth, G.; Sugár, S.; Pál, D.; Fügedi, K.D.; Drahos, L.; Schlosser, G.; Oláh, C.; Reis, H.; Kovalszky, I.; Szarvas, T.; et al. Glycosaminoglycan Analysis of FFPE Tissues from Prostate Cancer and Benign Prostate Hyperplasia Patients Reveals Altered Regulatory Functions and Independent Markers for Survival. Cancers 2022, 14, 4867. https://doi.org/10.3390/cancers14194867
Tóth G, Sugár S, Pál D, Fügedi KD, Drahos L, Schlosser G, Oláh C, Reis H, Kovalszky I, Szarvas T, et al. Glycosaminoglycan Analysis of FFPE Tissues from Prostate Cancer and Benign Prostate Hyperplasia Patients Reveals Altered Regulatory Functions and Independent Markers for Survival. Cancers. 2022; 14(19):4867. https://doi.org/10.3390/cancers14194867
Chicago/Turabian StyleTóth, Gábor, Simon Sugár, Domonkos Pál, Kata Dorina Fügedi, László Drahos, Gitta Schlosser, Csilla Oláh, Henning Reis, Ilona Kovalszky, Tibor Szarvas, and et al. 2022. "Glycosaminoglycan Analysis of FFPE Tissues from Prostate Cancer and Benign Prostate Hyperplasia Patients Reveals Altered Regulatory Functions and Independent Markers for Survival" Cancers 14, no. 19: 4867. https://doi.org/10.3390/cancers14194867
APA StyleTóth, G., Sugár, S., Pál, D., Fügedi, K. D., Drahos, L., Schlosser, G., Oláh, C., Reis, H., Kovalszky, I., Szarvas, T., & Turiák, L. (2022). Glycosaminoglycan Analysis of FFPE Tissues from Prostate Cancer and Benign Prostate Hyperplasia Patients Reveals Altered Regulatory Functions and Independent Markers for Survival. Cancers, 14(19), 4867. https://doi.org/10.3390/cancers14194867