Effectiveness of Naldemedine Compared with Magnesium Oxide in Preventing Opioid-Induced Constipation: A Randomized Controlled Trial
Abstract
:Simple Summary
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Design
2.2. Randomization and Masking
2.3. Endpoints
2.4. Statistical Analysis
3. Results
3.1. Baseline Characteristics
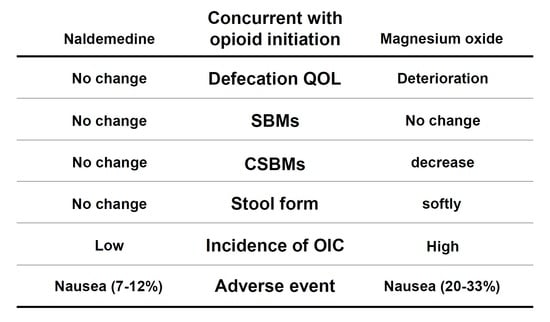
3.2. Primary and Secondary Endpoints
3.3. Safety Outcomes
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Portenoy, R.K.; Ahmed, E. Principles of Opioid Use in Cancer Pain. J. Clin. Oncol. 2014, 32, 1662–1670. [Google Scholar] [CrossRef] [PubMed]
- Caraceni, A.; Hanks, G.; Kaasa, S.; Bennett, M.I.; Brunelli, C.; Cherny, N.; Dale, O.; de Conno, F.; Fallon, M.; Hanna, M.; et al. Use of Opioid Analgesics in the Treatment of Cancer Pain: Evidence-Based Recommendations from the EAPC. Lancet Oncol. 2012, 13, e58–e68. [Google Scholar] [CrossRef]
- Poulsen, J.L.; Brock, C.; Olesen, A.E.; Nilsson, M.; Drewes, A.M. Evolving Paradigms in the Treatment of Opioid-Induced Bowel Dysfunction. Ther. Adv. Gastroenterol. 2015, 8, 360–372. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Morlion, B.; Clemens, K.E.; Dunlop, W. Quality of Life and Healthcare Resource in Patients Receiving Opioids for Chronic Pain: A Review of the Place of Oxycodone/Naloxone. Clin. Drug Investig. 2015, 35, 1–11. [Google Scholar] [CrossRef] [Green Version]
- Lazzari, M.; Greco, M.T.; Marcassa, C.; Finocchi, S.; Caldarulo, C.; Corli, O. Efficacy and Tolerability of Oral Oxycodone and Oxycodone/Naloxone Combination in Opioid-Naive Cancer Patients: A Propensity Analysis. Drug Des. Devel. Ther. 2015, 9, 5863–5872. [Google Scholar] [CrossRef] [Green Version]
- Camilleri, M. Opioid-Induced Constipation: Challenges and Therapeutic Opportunities. Am. J. Gastroenterol. 2011, 106, 835–842; quiz 843. [Google Scholar] [CrossRef]
- Wirz, S.; Wittmann, M.; Schenk, M.; Schroeck, A.; Schaefer, N.; Mueller, M.; Standop, J.; Kloecker, N.; Nadstawek, J. Gastrointestinal Symptoms under Opioid Therapy: A Prospective Comparison of Oral Sustained-Release Hydromorphone, Transdermal Fentanyl, and Transdermal Buprenorphine. Eur. J. Pain 2009, 13, 737–743. [Google Scholar] [CrossRef]
- Cook, S.F.; Lanza, L.; Zhou, X.; Sweeney, C.T.; Goss, D.; Hollis, K.; Mangel, A.W.; Fehnel, S.E. Gastrointestinal Side Effects in Chronic Opioid Users: Results from a Population-Based Survey. Aliment. Pharmacol. Ther. 2008, 27, 1224–1232. [Google Scholar] [CrossRef]
- Bell, T.J.; Panchal, S.J.; Miaskowski, C.; Bolge, S.C.; Milanova, T.; Williamson, R. The Prevalence, Severity, and Impact of Opioid-Induced Bowel Dysfunction: Results of a US and European Patient Survey (PROBE 1). Pain Med. 2009, 10, 35–42. [Google Scholar] [CrossRef]
- Myotoku, M.; Nakanishi, A.; Kanematsu, M.; Sakaguchi, N.; Hashimoto, N.; Koyama, F.; Yamaguchi, S.; Ikeda, K.; Konishi, H.; Hirotani, Y. Reduction of Opioid Side Effects by Prophylactic Measures of Palliative Care Team May Result in Improved Quality of Life. J. Palliat. Med. 2010, 13, 401–406. [Google Scholar] [CrossRef]
- Rosti, G.; Gatti, A.; Costantini, A.; Sabato, A.F.; Zucco, F. Opioid-Related Bowel Dysfunction: Prevalence and Identification of Predictive Factors in a Large Sample of Italian Patients on Chronic Treatment. Eur. Rev. Med. Pharmacol. Sci. 2010, 14, 1045–1050. [Google Scholar] [PubMed]
- Tokoro, A.; Imai, H.; Fumita, S.; Harada, T.; Noriyuki, T.; Gamoh, M.; Akashi, Y.; Sato, H.; Kizawa, Y. Incidence of Opioid-Induced Constipation in Japanese Patients with Cancer Pain: A Prospective Observational Cohort Study. Cancer Med. 2019, 8, 4883–4891. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Tuteja, A.K.; Biskupiak, J.; Stoddard, G.J.; Lipman, A.G. Opioid-Induced Bowel Disorders and Narcotic Bowel Syndrome in Patients with Chronic Non-Cancer Pain. Neurogastroenterol. Motil. 2010, 22, 424–430.e96. [Google Scholar] [CrossRef] [PubMed]
- Lee, A.A.; Hasler, W.L. Opioids and Gi Motility-Friend or Foe? Curr. Treat. Options Gastroenterol. 2016, 14, 478–494. [Google Scholar] [CrossRef]
- Japanese Society of Palliative Medicine; Committee on Guidelines. Guidelines for the Palliation of Gastrointestinal Symptoms in Cancer Patients 2017 Edition; Published Online; Japanese Society for Palliative Medicine: Osaka, Japan, 2017; p. 32. [Google Scholar]
- Ishihara, M.; Ikesue, H.; Matsunaga, H.; Suemaru, K.; Kitaichi, K.; Suetsugu, K.; Oishi, R.; Sendo, T.; Araki, H.; Itoh, Y.; et al. A Multi-Institutional Study Analyzing Effect of Prophylactic Medication for Prevention of Opioid-Induced Gastrointestinal Dysfunction. Clin. J. Pain 2012, 28, 373–381. [Google Scholar] [CrossRef]
- Camilleri, M.; Drossman, D.A.; Becker, G.; Webster, L.R.; Davies, A.N.; Mawe, G.M. Emerging Treatments in Neurogastroenterology: A Multidisciplinary Working Group Consensus Statement on Opioid-Induced Constipation. Neurogastroenterol. Motil. 2014, 26, 1386–1395. [Google Scholar] [CrossRef] [Green Version]
- Fukumura, K.; Yokota, T.; Baba, Y.; Arjona Ferreira, J.C. Phase 1, Randomized, Double-Blind, Placebo-Controlled Studies on the Safety, Tolerability, and Pharmacokinetics of Naldemedine in Healthy Volunteers. Clin. Pharmacol. Drug Dev. 2018, 7, 474–483. [Google Scholar] [CrossRef] [Green Version]
- Webster, L.R.; Yamada, T.; Arjona Ferreira, J.C. A phase 2b, Randomized, Double-Blind Placebo-Controlled Study to Evaluate the Efficacy and Safety of Naldemedine for the Treatment of Opioid-Induced Constipation in Patients with Chronic Noncancer Pain. Pain Med. 2017, 18, 2350–2360. [Google Scholar] [CrossRef]
- Song, X.; Wang, D.; Qu, X.; Dong, N.; Teng, S. A Meta-Analysis of Naldemedine for the Treatment of Opioid-Induced Constipation. Expert Rev. Clin. Pharmacol. 2019, 12, 121–128. [Google Scholar] [CrossRef]
- Ozaki, A.; Kessoku, T.; Iwaki, M.; Kobayashi, T.; Yoshihara, T.; Kato, T.; Honda, Y.; Ogawa, Y.; Imajo, K.; Higurashi, T.; et al. Comparing the Effectiveness of Magnesium Oxide and Naldemedine in Preventing Opioid-Induced Constipation: A Proof of Concept, Single Institutional, Two Arm, Open-Label, Phase II, Randomized Controlled Trial: The MAGNET Study. Trials 2020, 21, 453. [Google Scholar] [CrossRef]
- Schulz, K.F.; Altman, D.G.; Moher, D.; Consolidated Standards of Reporting Trials Group. CONSORT 2010 Statement: Updated Guidelines for Reporting Parallel Group Randomised Trials. BMJ 2010, 340, c332. [Google Scholar] [CrossRef] [PubMed]
- Nomura, H.; Agatsuma, T.; Mimura, T. Validity and Reliability of the Japanese Version of the Patient Assessment of Constipation Quality of Life Questionnaire. J. Gastroenterol. 2014, 49, 667–673. [Google Scholar] [CrossRef] [PubMed]
- Katakami, N.; Harada, T.; Murata, T.; Shinozaki, K.; Tsutsumi, M.; Yokota, T.; Arai, M.; Tada, Y.; Narabayashi, M.; Boku, N. Randomized phase III and Extension Studies: Efficacy and Impacts on Quality of Life of Naldemedine in Subjects with Opioid-Induced Constipation and Cancer. Ann. Oncol. 2018, 29, 1461–1467. [Google Scholar] [CrossRef] [PubMed]
- Nakajima, A.; Seki, M.; Taniguchi, S.; Ohta, A.; Gillberg, P.G.; Mattsson, J.P.; Camilleri, M. Safety and Efficacy of Elobixibat for Chronic Constipation: Results from a Randomised, Double-Blind, Placebo-Controlled, phase 3 Trial and an Open-Label, Single-Arm, phase 3 Trial. Lancet Gastroenterol. Hepatol. 2018, 3, 537–547. [Google Scholar] [CrossRef]
- Marquis, P.; de la Loge, C.; Dubois, D.; McDermott, A.; Chassany, O. Development and Validation of the Patient Assessment of Constipation Quality of Life Questionnaire. Scand. J. Gastroenterol. 2005, 40, 540–551. [Google Scholar] [CrossRef]
- Frank, L.; Kleinman, L.; Farup, C.; Taylor, L.; Miner, P. Psychometric Validation of a Constipation Symptom Assessment Questionnaire. Scand. J. Gastroenterol. 1999, 34, 870–877. [Google Scholar]
- Longstreth, G.F.; Thompson, W.G.; Chey, W.D.; Houghton, L.A.; Mearin, F.; Spiller, R.C. Functional Bowel Disorders. Gastroenterology 2006, 130, 1480–1491. [Google Scholar] [CrossRef]
- Agachan, F.; Chen, T.; Pfeifer, J.; Reissman, P.; Wexner, S.D. A Constipation Scoring System to Simplify Evaluation and Management of Constipated Patients. Dis. Colon Rectum 1996, 39, 681–685. [Google Scholar] [CrossRef]
- Mearin, F.; Lacy, B.E.; Chang, L.; Chey, W.D.; Lembo, A.J.; Simren, M.; Spiller, R. Bowel Disorders. Gastroenterology 2016, 150, 1393–1407.e5. [Google Scholar] [CrossRef] [Green Version]
- Fukuhara, S.; Bito, S.; Green, J.; Hsiao, A.; Kurokawa, K. Translation, Adaptation, and Validation of the SF-36 Health Survey for Use in Japan. J. Clin. Epidemiol. 1998, 51, 1037–1044. [Google Scholar] [CrossRef]
- Mueller-Lissner, S.; Kamm, M.A.; Wald, A.; Hinkel, U.; Koehler, U.; Richter, E.; Bubeck, J. Multicenter, 4-Week, Double-Blind, Randomized, Placebo-Controlled Trial of Sodium Picosulfate in Patients with Chronic Constipation. Am. J. Gastroenterol. 2010, 105, 897–903. [Google Scholar] [CrossRef] [PubMed]
- European Medicines Agency. Guideline on the Evaluation of Medicinal Products for the Treatment of Chronic Constipation (Including Opioid Induced Constipation) and for Bowel Cleansing; European Medicines Agency and Committee for Medicinal Products for Human Use (CHMP): Amsterdam, The Netherlands, 2015. [Google Scholar]
- Murakami, K.; Sasakii, S.; Okubo, H.; Takahashi, Y.; Hoso, Y.; Itabashi, M.; Freshmen in Dietetic Courses Study II Group. Food Intake and Functional Constipation: A Cross-Sectional Study of 3,835 Japanese Women Aged 18–20 Years. J. Nutr. Sci. Vitaminol. 2007, 53, 30–36. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Asaoka, D.; Takeda, T.; Inami, Y.; Abe, D.; Shimada, Y.; Matsumoto, K.; Ueyama, H.; Matsumoto, K.; Komori, H.; Akazawa, Y.; et al. The Association Between Frailty and Abdominal Symptoms: A Hospital-Based Cross-Sectional Study. Intern. Med. 2020, 59, 1677–1685. [Google Scholar] [CrossRef] [PubMed]
- Smith, K.; Hopp, M.; Mundin, G.; Bond, S.; Bailey, P.; Woodward, J.; Palaniappan, K.; Church, A.; Limb, M.; Connor, A. Naloxone as Part of a Prolonged Release Oxycodone/Naloxone Combination Reduces Oxycodone-Induced Slowing of Gastrointestinal Transit in Healthy Volunteers. Expert Opin. Investig. Drugs 2011, 20, 427–439. [Google Scholar] [CrossRef]
- Smith, P.; Lavery, A.; Turkington, R.C. An Overview of Acute Gastrointestinal Side Effects of Systemic Anti-Cancer Therapy and Their Management. Best Pract. Res. Clin. Gastroenterol. 2020, 48–49, 101691. [Google Scholar] [CrossRef]
- Knowles, C.H.; Lindberg, G.; Panza, E.; De Giorgio, R. New Perspectives in the Diagnosis and Management of Enteric Neuropathies. Nat. Rev. Gastroenterol. Hepatol. 2013, 10, 206–218. [Google Scholar] [CrossRef]
- Stojanovska, V.; Sakkal, S.; Nurgali, K. Platinum-Based Chemotherapy: Gastrointestinal Immunomodulation and Enteric Nervous System Toxicity. Am. J. Physiol. Gastrointest. Liver Physiol. 2015, 308, G223–G232. [Google Scholar] [CrossRef] [Green Version]
- Narayan, P.; Wahby, S.; Gao, J.J.; Amiri-Kordestani, L.; Ibrahim, A.; Bloomquist, E.; Tang, S.; Xu, Y.; Liu, J.; Fu, W.; et al. FDA Approval Summary: Atezolizumab plus Paclitaxel Protein-Bound for the Treatment of Patients with Advanced or Metastatic TNBC Whose Tumors Express PD-L1. Clin. Cancer Res. 2020, 26, 2284–2289. [Google Scholar] [CrossRef] [Green Version]
- Hanai, A.; Ishiguro, H.; Sozu, T.; Tsuda, M.; Arai, H.; Mitani, A.; Tsuboyama, T. Effects of a Self-Management Program on Antiemetic-Induced Constipation During Chemotherapy Among Breast Cancer Patients: A Randomized Controlled Clinical Trial. Breast Cancer Res. Treat. 2016, 155, 99–107. [Google Scholar] [CrossRef] [Green Version]
- Stein, A.; Voigt, W.; Jordan, K. Chemotherapy-Induced Diarrhea: Pathophysiology, Frequency and Guideline-Based Management. Ther. Adv. Med. Oncol. 2010, 2, 51–63. [Google Scholar] [CrossRef] [Green Version]
- Eisenberg, P.; Figueroa-Vadillo, J.; Zamora, R.; Charu, V.; Hajdenberg, J.; Cartmell, A.; Macciocchi, A.; Grunberg, S.; 99-04 Palonosetron Study Group. Improved Prevention of Moderately Emetogenic Chemotherapy-Induced Nausea and Vomiting with Palonosetron, a Pharmacologically novel 5-HT3 Receptor Antagonist: Results of a phase III, Single-Dose Trial Versus Dolasetron. Cancer 2003, 98, 2473–2482. [Google Scholar] [CrossRef] [PubMed]
- Rojas, C.; Raje, M.; Tsukamoto, T.; Slusher, B.S. Molecular Mechanisms of 5-HT(3) and NK(1) Receptor Antagonists in Prevention of Emesis. Eur. J. Pharmacol. 2014, 722, 26–37. [Google Scholar] [CrossRef] [PubMed]
- Minami, M.; Endo, T.; Yokota, H.; Ogawa, T.; Nemoto, M.; Hamaue, N.; Hirafuji, M.; Yoshioka, M.; Nagahisa, A.; Andrews, P.L. Effects of CP-99, 994, a Tachykinin NK(1) Receptor Antagonist, on Abdominal Afferent Vagal Activity in Ferrets: Evidence for Involvement of NK(1) and 5-HT(3) Receptors. Eur. J. Pharmacol. 2001, 428, 215–220. [Google Scholar] [CrossRef]
- Crockett, S.D.; Greer, K.B.; Heidelbaugh, J.J.; Falck-Ytter, Y.; Hanson, B.J.; Sultan, S.; American Gastroenterological Association Institute Clinical Guidelines Committee. American Gastroenterological Association Institute Guideline on the Medical Management of Opioid-Induced Constipation. Gastroenterology 2019, 156, 218–226. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kanemasa, T.; Matsuzaki, T.; Koike, K.; Hasegawa, M.; Suzuki, T. Preventive Effects of Naldemedine, Peripherally Acting Mu-Opioid Receptor Antagonist, on Morphine-Induced Nausea and Vomiting in Ferrets. Life Sci. 2020, 257, 118048. [Google Scholar] [CrossRef] [PubMed]
- Sato, J.; Tanaka, R.; Ishikawa, H.; Suzuki, T.; Shino, M. A Preliminary Study of the Effect of Naldemedine Tosylate on Opioid-Induced Nausea and Vomiting. Support. Care Cancer 2020, 28, 1083–1088. [Google Scholar] [CrossRef]
- Gisondi, P.; Conti, A.; Galdo, G.; Piaserico, S.; de Simone, C.; Girolomoni, G. Ustekinumab does not increase body mass index in patients with chronic plaque psoriasis: A prospective cohort study. Br. J. Dermatol. 2013, 168, 1124–1127. [Google Scholar] [CrossRef]
- Clinical Guidelines for Cancer Pain Management, 2nd ed.; WHO: Geneva, Switzerland, 2014.




| Characteristic | 1500 mg MgO | 0.2 mg NAL |
|---|---|---|
| (n = 60) | (n = 60) | |
| Age (years) | 51 (9) | 52 (9) |
| Sex | ||
| Female | 37 (62) | 36 (60) |
| Male | 23 (38) | 24 (40) |
| Body mass index (kg/m2) | 22 (4) | 22 (10) |
| History of abdominal operation | 33 (55) | 33 (55) |
| ECOG PS 0–2 | 54 (90) | 52 (87) |
| Palliative prognosis index ≤ 3.5 | 56 (93) | 53 (88) |
| Primary tumor site | ||
| Hepatobiliary and pancreas | 18 (30) | 21 (35) |
| Gastrointestinal tract | 13 (22) | 16 (27) |
| Lung | 5 (8) | 3 (5) |
| Others | 24 (40) | 20 (33) |
| Concurrent cancer treatment | ||
| Chemotherapy (0–14 days) | 0 | 0 |
| Chemotherapy (15–84 days) | 27 (45) | 27 (45) |
| Chemotherapy type | ||
| Platinum agents | 10 (37) | 10 (37) |
| Taxane agents | 6 (22) | 4 (15) |
| Anti-metabolite agents | 10 (37) | 13 (48) |
| Irinotecan | 0 | 0 |
| Antiemetics during chemotherapy # | 3 (11) | 2 (7) |
| Perioperative | 12 (20) | 12 (20) |
| Best supportive care | 9 (15) | 14 (23) |
| Others | 12 (20) | 7 (12) |
| Concomitant medications | ||
| Laxative use | ||
| Naïve | 38 (63) | 42 (70) |
| Regular use (irritant laxative) | 5 (8) | 5 (8) |
| Rescue use (irritant laxative) | 17 (28) | 13 (22) |
| Opioid use at baseline | ||
| Strong opioid | 27 (45) | 30 (50) |
| Weak opioid | 33 (55) | 30 (50) |
| Mean total daily dose of opioid * | ||
| At baseline (mg) | 13 (4) | 13 (4) |
| At 2 weeks (mg) | 14 (4) | 13 (5) |
| At 12 weeks (mg) | 22 (19) | 23 (23) |
| Baseline defecation status | ||
| Mean JPAC-QOL | 0.9 (0.6) | 0.9 (0.4) |
| SBMs per week | 4.3 (1.7) | 4.5 (2.8) |
| CSBMs per week | 3.8 (1.5) | 3.7 (2.1) |
| Stool consistency score | 3.8 (0.7) | 3.6 (1.9) |
| Endpoints | 2 Weeks | 12 Weeks | ||||
|---|---|---|---|---|---|---|
| 1500 mg MgO | 0.2 mg NAL | p Value | 1500 mg MgO | 0.2 mg NAL | p-Value | |
| (n = 60) | (n = 60) | (n = 60) | (n = 60) | |||
| Primary endpoint | ||||||
| JPAC-QOL Overall | 0.5 (0.4) | −0.01 (0.3) | <0.001 | 0.4 (0.4) | 0.03 (0.3) | <0.001 |
| Secondary endpoints | ||||||
| SBM (times/week) | 0.3 (1.7) | −0.1 (2.4) | 0.3 | 0.4 (1.8) | 0.03 (2.3) | 0.4 |
| Stool consistency score | 0.6 (1.1) | −0.3 (1.1) | <0.001 | 0.6 (1.1) | −0.4 (0.9) | <0.001 |
| PAC-SYM Overall | 0.6 (0.5) | 0.02 (0.3) | <0.001 | 0.5 (0.5) | 0.01 (0.4) | <0.001 |
| ROME IV, n (%) | 33 (55) | 20 (33) | 0.02 | 41 (68) | 24 (40) | 0.002 |
| CSS | 0.3 (0.3) | 0.0 (0.3) | <0.001 | 0.5 (0.4) | −0.02 (0.2) | <0.001 |
| SF-36 | ||||||
| Physical component summary | 0 (0) | 0.04 (6.6) | 1.0 | −1.5 (5) | −2.6 (7.2) | 0.3 |
| Mental component summary | 0 (0) | 1.9 (6.1) | 0.02 | 0.2 (5.1) | 0.6 (6.2) | 0.7 |
| Role component summary | 0 (0) | −1.9 (9.7) | 0.1 | 0.9 (7.7) | −1.2 (9.5) | 0.2 |
| Post hoc analyses | ||||||
| CSBM (times/week) | −0.9 (1.5) | 0 (2.0) | 0.01 | −0.7 (1.2) | 0.2 (2.0) | 0.003 |
| JPAC-QOL subscale | ||||||
| Physical discomfort | 0.6 (0.9) | −0.01 (0.6) | <0.001 | 0.6 (0.8) | 0.2 (0.7) | 0.01 |
| Psychosocial discomfort | 0.6 (0.8) | −0.01 (0.4) | <0.001 | 0.5 (0.8) | 0.1 (0.5) | <0.001 |
| Worries/concerns | 0.06 (0.2) | −0.05 (0.4) | 0.1 | 0 (0.5) | −0.1 (0.5) | 0.5 |
| Satisfaction | 1.0 (0.7) | 0.07 (0.5) | <0.001 | 0.9 (0.8) | 0 (0.6) | <0.001 |
| PAC-SYM subscale | ||||||
| Stool symptoms | 0.3 (0.7) | −0.1 (0.6) | <0.001 | 0.2 (0.7) | −0.1 (0.8) | 0.02 |
| Rectal symptoms | 0.7 (0.8) | 0.1 (0.4) | <0.001 | 0.6 (0.8) | 0.2 (0.6) | <0.001 |
| Abdominal symptoms | 0.8 (1.0) | 0.1 (0.4) | <0.001 | 0.7 (0.9) | 0.03 (0.6) | <0.001 |
| Mean time to first SBM (h) | 4.9 (0.8) | 4.9 (1.0) | 0.7 | 4.9 (0.1) | 4.9 (0.1) | 1.0 |
| Mean time to first CSBM (h) | 10.4 (6.4) | 6.4 (3.0) | <0.001 | 10.1 (6.0) | 6.4 (3.9) | <0.001 |
| Numerical rating score for pain | −1.4 (1.8) | −1.2 (2.8) | 0.7 | −1.4 (1.8) | −1.2 (2.8) | 0.6 |
| Adverse Events | 2 Weeks | 12 Weeks | ||||
|---|---|---|---|---|---|---|
| 1500 mg MgO | 0.2 mg NAL | p-Value | 1500 mg MgO | 0.2 mg NAL | p-Value | |
| (n = 60) | (n = 60) | (n = 60) | (n = 60) | |||
| Total adverse event | 32 (53) | 30 (50) | 39 (65) | 32 (53) | ||
| TRAEs | 21 (35) | 11 (18) | 0.02 | 31 (52) | 16 (27) | 0.01 |
| TRAE leading to discontinuation | 0 | 0 | 0 | 0 | ||
| Serious AEs | 0 | 0 | 0 | 0 | ||
| Serious TRAEs | 0 | 0 | 0 | 0 | ||
| Serious TRAE leading to discontinuation | 0 | 0 | 0 | 0 | ||
| Deaths | 0 | 0 | 0 | 0 | ||
| TRAEs | ||||||
| Gastrointestinal disorders SOC | ||||||
| Abdominal pain | 4 (7) | 3 (5) | 9 (15) | 5 (8) | 0.3 | |
| Diarrhea | 4 (7) | 5 (8) | 4 (7) | 6 (10) | ||
| Abdominal distension | 1 (0) | 0 | 5 (8) | 1 (2) | 0.06 | |
| Nausea | 12 (20) | 4 (7) | 0.03 | 20 (33) | 7 (12) | 0.005 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Ozaki, A.; Kessoku, T.; Tanaka, K.; Yamamoto, A.; Takahashi, K.; Takeda, Y.; Kasai, Y.; Iwaki, M.; Kobayashi, T.; Yoshihara, T.; et al. Effectiveness of Naldemedine Compared with Magnesium Oxide in Preventing Opioid-Induced Constipation: A Randomized Controlled Trial. Cancers 2022, 14, 2112. https://doi.org/10.3390/cancers14092112
Ozaki A, Kessoku T, Tanaka K, Yamamoto A, Takahashi K, Takeda Y, Kasai Y, Iwaki M, Kobayashi T, Yoshihara T, et al. Effectiveness of Naldemedine Compared with Magnesium Oxide in Preventing Opioid-Induced Constipation: A Randomized Controlled Trial. Cancers. 2022; 14(9):2112. https://doi.org/10.3390/cancers14092112
Chicago/Turabian StyleOzaki, Anna, Takaomi Kessoku, Kosuke Tanaka, Atsushi Yamamoto, Kota Takahashi, Yuma Takeda, Yuki Kasai, Michihiro Iwaki, Takashi Kobayashi, Tsutomu Yoshihara, and et al. 2022. "Effectiveness of Naldemedine Compared with Magnesium Oxide in Preventing Opioid-Induced Constipation: A Randomized Controlled Trial" Cancers 14, no. 9: 2112. https://doi.org/10.3390/cancers14092112
APA StyleOzaki, A., Kessoku, T., Tanaka, K., Yamamoto, A., Takahashi, K., Takeda, Y., Kasai, Y., Iwaki, M., Kobayashi, T., Yoshihara, T., Kato, T., Suzuki, A., Honda, Y., Ogawa, Y., Fuyuki, A., Imajo, K., Higurashi, T., Yoneda, M., Taguri, M., ... Nakajima, A. (2022). Effectiveness of Naldemedine Compared with Magnesium Oxide in Preventing Opioid-Induced Constipation: A Randomized Controlled Trial. Cancers, 14(9), 2112. https://doi.org/10.3390/cancers14092112