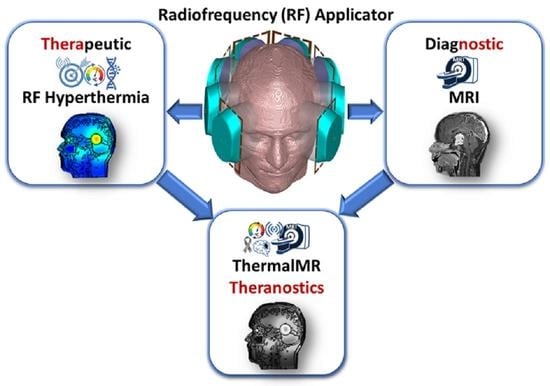
Advanced Radio Frequency Applicators for Thermal Magnetic Resonance Theranostics of Brain Tumors
Abstract
:Simple Summary
Abstract
1. Introduction
2. Materials and Methods
2.1. Electromagnetic Field Simulations and Patient Model
2.2. Integration of Loop and Dipole Antenna in a Hybrid RF Building Block

2.3. ThermalMR RF Applicators
2.4. Transmission Field and RF Power Deposition for MRI
2.5. Targeted RF Heating for Thermal Therapy
2.6. Temperature Simulations
2.7. Thermal Therapy Quality Assessment
2.8. Statistical Analysis
3. Results
3.1. Transmission Field and RF Power Deposition for MRI
3.2. Targeted RF Heating for Thermal Therapy
3.3. Temperature Simulations
3.4. Thermal Therapy Quality Assessment
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Abbreviations
| MR | magnetic resonance |
| MRI | magnetic resonance imaging |
| ThermalMR | thermal magnetic resonance |
| MRTh | MR thermometry |
| RF | radiofrequency |
| UHF | ultrahigh field |
| HT | hyperthermia |
| RT | radiotherapy |
| WHO | World Health Organization |
| GBM | glioblastoma multiforme |
| CNS | central nervous system |
| TMTP | thermalMR treatment planning |
| E-field | electric Field |
| B1+ | RF transmission field used for MRI |
| B₀ | main static magnetic field of MRI scanner |
| SAR | specific absorption rate |
| SAR10g | 10 g averaged SAR distribution |
| EMF | electromagnetic field |
| SGBT | self-grounded bow-tie |
| LD | loop+SGBT dipole building block |
| L | loop building block |
| D | SGBT dipole building block |
| 16LD | hybrid 16-channel loop+SGBT dipole ThermalMR RF applicator |
| 8D | 8-channel SGBT dipole ThermalMR RF applicator |
| 8L | 8-channel loop ThermalMR RF applicator |
| cir | circular array |
| cir_HS | circular horse-shoe array |
| ellip | elliptical array |
| ellip_HS | elliptical horse-shoe array |
| 16LDcir | circular array variant of 16LD |
| 16LDcir_HS | circular horse-shoe array variant of 16LD |
| 16LDellip | elliptical array variant of 16LD |
| 16LDellip_HS | elliptical horse-shoe array variant of 16LD |
| 8Dcir | circular array variant of 8D |
| 8Dcir_HS | circular horse-shoe array variant of 8D |
| 8Dellip | elliptical array variant of 8D |
| 8Dellip_HS | elliptical horse-shoe array variant of 8D |
| 8Lcir | circular array variant of 8L |
| 8Lcir_HS | circular horse-shoe array variant of 8L |
| 8Lellip | elliptical array variant of 8L |
| 8Lellip_HS | elliptical horse-shoe array variant of 8L |
| MVFS | multiplexed vector field shaping |
| M | excitation mode provided by MVFS algorithm |
| PLD | power loss density |
| ROI | region of interest |
| TV | target volume |
| TC | tumor coverage |
| TC25 | fraction of the tumor volume enclosed by 25% peak SARmax isolines |
| TC50 | fraction of the tumor volume enclosed by 50% peak SARmax isolines |
| TC80 | fraction of the tumor volume enclosed by 80% peak SARmax isolines |
| TC100 | fraction of the tumor volume enclosed by 100% peak SARmax isolines |
| HTQ | Hotspot-to-target quotient |
| SAF | SAR amplification factor |
| ESHO | European Society for Hyperthermic Oncology |
| T | temperature |
| Tmean | mean temperature inside TV |
| Tmax | maximum temperature inside TV |
| Tx°C | index temperature coverage inside TV |
| T40°C | fraction of the tumor volume enclosed by 40 °C |
| T41°C | fraction of the tumor volume enclosed by 41 °C |
| T42°C | fraction of the tumor volume enclosed by 42 °C |
| Max | maximum |
| Min | minimum |
| CEM | cumulative equivalent minutes |
| FoV | field-of-view |
References
- Lee Titsworth, W.; Murad, G.J.; Hoh, B.L.; Rahman, M. Fighting fire with fire: The revival of thermotherapy for gliomas. Anticancer Res. 2014, 34, 565–574. [Google Scholar] [PubMed]
- Wust, P.; Hildebrandt, B.; Sreenivasa, G.; Rau, B.; Gellermann, J.; Riess, H.; Felix, R.; Schlag, P.M. Hyperthermia in combined treatment of cancer. Lancet Oncol. 2002, 3, 487–497. [Google Scholar] [CrossRef] [PubMed]
- Kok, H.P.; Crezee, J. Hyperthermia treatment planning: Clinical application and ongoing research. In Proceedings of the 2020 14th European Conference on Antennas and Propagation (EuCAP), Copenhagen, Denmark, 15–20 March 2020; pp. 1–5. [Google Scholar]
- Horsman, M.R.; Overgaard, J. Hyperthermia: A potent enhancer of radiotherapy. Clin. Oncol. 2007, 19, 418–426. [Google Scholar] [CrossRef] [PubMed]
- Issels, R.D.; Lindner, L.H.; Verweij, J.; Wust, P.; Reichardt, P.; Schem, B.C.; Abdel-Rahman, S.; Daugaard, S.; Salat, C.; Wendtner, C.M.; et al. Neo-adjuvant chemotherapy alone or with regional hyperthermia for localised high-risk soft-tissue sarcoma: A randomised phase 3 multicentre study. Lancet Oncol. 2010, 11, 561–570. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Sminia, P.; van der Zee, J.; Wondergem, J.; Haveman, J. Effect of hyperthermia on the central nervous system: A review. Int. J. Hyperth. 1994, 10, 1–30. [Google Scholar] [CrossRef]
- Sneed, P.K.; Stauffer, P.R.; McDermott, M.W.; Diederich, C.J.; Lamborn, K.R.; Prados, M.D.; Chang, S.; Weaver, K.A.; Spry, L.; Malec, M.K.; et al. Survival benefit of hyperthermia in a prospective randomized trial of brachytherapy boost +/- hyperthermia for glioblastoma multiforme. Int. J. Radiat. Oncol. Biol. Phys. 1998, 40, 287–295. [Google Scholar] [CrossRef]
- Seegenschmiedt, M.H.; Karlsson, U.L.; Black, P.; Brady, L.W. Thermoradiotherapy for brain tumors. Three cases of recurrent malignant astrocytoma and review of clinical experience. Am. J. Clin. Oncol. 1995, 18, 510–518. [Google Scholar] [CrossRef]
- Yang, Z.; Gao, D.; Zhao, J.; Yang, G.; Guo, M.; Wang, Y.; Ren, X.; Kim, J.S.; Jin, L.; Tian, Z.; et al. Thermal immuno-nanomedicine in cancer. Nat. Rev. Clin. Oncol. 2023, 20, 116–134. [Google Scholar] [CrossRef]
- Jordan, A.; Scholz, R.; Maier-Hauff, K.; Johannsen, M.; Wust, P.; Nadobny, J.; Schirra, H.; Schmidt, H.; Deger, S.; Loening, S.; et al. Presentation of a new magnetic field therapy system for the treatment of human solid tumors with magnetic fluid hyperthermia. J. Magn. Magn. Mater. 2001, 225, 118–126. [Google Scholar] [CrossRef] [Green Version]
- Kok, H.P.; Crezee, J. Adapt2Heat: Treatment planning-assisted locoregional hyperthermia by on-line visualization, optimization and re-optimization of SAR and temperature distributions. Int. J. Hyperth. 2022, 39, 265–277. [Google Scholar] [CrossRef]
- Hersh, A.M.; Bhimreddy, M.; Weber-Levine, C.; Jiang, K.; Alomari, S.; Theodore, N.; Manbachi, A.; Tyler, B.M. Applications of Focused Ultrasound for the Treatment of Glioblastoma: A New Frontier. Cancers 2022, 14, 4920. [Google Scholar] [CrossRef] [PubMed]
- Huang, P.C.; Chaney, E.J.; Aksamitiene, E.; Barkalifa, R.; Spillman, D.R., Jr.; Bogan, B.J.; Boppart, S.A. Biomechanical sensing of in vivo magnetic nanoparticle hyperthermia-treated melanoma using magnetomotive optical coherence elastography. Theranostics 2021, 11, 5620–5633. [Google Scholar] [CrossRef] [PubMed]
- Liu, X.; Zhang, Y.; Wang, Y.; Zhu, W.; Li, G.; Ma, X.; Zhang, Y.; Chen, S.; Tiwari, S.; Shi, K.; et al. Comprehensive understanding of magnetic hyperthermia for improving antitumor therapeutic efficacy. Theranostics 2020, 10, 3793–3815. [Google Scholar] [CrossRef]
- Kok, H.P.; Korshuize-van Straten, L.; Bakker, A.; de Kroon-Oldenhof, R.; Westerveld, G.H.; Versteijne, E.; Stalpers, L.J.A.; Crezee, J. Feasibility of on-line temperature-based hyperthermia treatment planning to improve tumour temperatures during locoregional hyperthermia. Int. J. Hyperth. 2018, 34, 1082–1091. [Google Scholar] [CrossRef] [Green Version]
- Sheybani, N.D.; Batts, A.J.; Mathew, A.S.; Thim, E.A.; Price, R.J. Focused Ultrasound Hyperthermia Augments Release of Glioma-derived Extracellular Vesicles with Differential Immunomodulatory Capacity. Theranostics 2020, 10, 7436–7447. [Google Scholar] [CrossRef]
- Kok, H.P.; Cressman, E.N.K.; Ceelen, W.; Brace, C.L.; Ivkov, R.; Grull, H.; Ter Haar, G.; Wust, P.; Crezee, J. Heating technology for malignant tumors: A review. Int. J. Hyperth. 2020, 37, 711–741. [Google Scholar] [CrossRef] [PubMed]
- Canters, R.A.; Paulides, M.M.; Franckena, M.F.; van der Zee, J.; van Rhoon, G.C. Implementation of treatment planning in the routine clinical procedure of regional hyperthermia treatment of cervical cancer: An overview and the Rotterdam experience. Int. J. Hyperth. 2012, 28, 570–581. [Google Scholar] [CrossRef]
- Fang, Y.; He, Y.; Wu, C.; Zhang, M.; Gu, Z.; Zhang, J.; Liu, E.; Xu, Q.; Asrorov, A.M.; Huang, Y. Magnetism-mediated targeting hyperthermia-immunotherapy in "cold" tumor with CSF1R inhibitor. Theranostics 2021, 11, 6860–6872. [Google Scholar] [CrossRef]
- Kato, H.; Ishida, T. Present and future status of noninvasive selective deep heating using RF in hyperthermia. Med. Biol. Eng. Comput. 1993, 31, S2–S11. [Google Scholar] [CrossRef]
- Sullivan, D.M.; Ben-Yosef, R.; Kapp, D.S. Stanford 3D hyperthermia treatment planning system. Technical review and clinical summary. Int. J. Hyperth. 1993, 9, 627–643. [Google Scholar] [CrossRef]
- Rijnen, Z.; Bakker, J.F.; Canters, R.A.; Togni, P.; Verduijn, G.M.; Levendag, P.C.; Van Rhoon, G.C.; Paulides, M.M. Clinical integration of software tool VEDO for adaptive and quantitative application of phased array hyperthermia in the head and neck. Int. J. Hyperth. 2013, 29, 181–193. [Google Scholar] [CrossRef] [PubMed]
- Kiyatkin, E.A.; Sharma, H.S. Permeability of the blood-brain barrier depends on brain temperature. Neuroscience 2009, 161, 926–939. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Tabatabaei, S.N.; Girouard, H.; Carret, A.S.; Martel, S. Remote control of the permeability of the blood-brain barrier by magnetic heating of nanoparticles: A proof of concept for brain drug delivery. J. Control. Release 2015, 206, 49–57. [Google Scholar] [CrossRef] [PubMed]
- Brito, B.; Price, T.W.; Gallo, J.; Banobre-Lopez, M.; Stasiuk, G.J. Smart magnetic resonance imaging-based theranostics for cancer. Theranostics 2021, 11, 8706–8737. [Google Scholar] [CrossRef]
- Rabha, B.; Bharadwaj, K.K.; Pati, S.; Choudhury, B.K.; Sarkar, T.; Kari, Z.A.; Edinur, H.A.; Baishya, D.; Atanase, L.I. Development of Polymer-Based Nanoformulations for Glioblastoma Brain Cancer Therapy and Diagnosis: An Update. Polymers 2021, 13, 4114. [Google Scholar] [CrossRef]
- Ji, Y.; Winter, L.; Navarro, L.; Ku, M.C.; Periquito, J.S.; Pham, M.; Hoffmann, W.; Theune, L.E.; Calderon, M.; Niendorf, T. Controlled Release of Therapeutics from Thermoresponsive Nanogels: A Thermal Magnetic Resonance Feasibility Study. Cancers 2020, 12, 1380. [Google Scholar] [CrossRef]
- Kneidl, B.; Peller, M.; Winter, G.; Lindner, L.H.; Hossann, M. Thermosensitive liposomal drug delivery systems: State of the art review. Int. J. Nanomed. 2014, 9, 4387–4398. [Google Scholar] [CrossRef] [Green Version]
- Paulides, M.M.; Dobsicek Trefna, H.; Curto, S.; Rodrigues, D.B. Recent technological advancements in radiofrequency- andmicrowave-mediated hyperthermia for enhancing drug delivery. Adv. Drug Deliv. Rev. 2020, 163–164, 3–18. [Google Scholar] [CrossRef]
- Huang, Q.; Hu, J.K.; Lohr, F.; Zhang, L.; Braun, R.; Lanzen, J.; Little, J.B.; Dewhirst, M.W.; Li, C.Y. Heat-induced gene expression as a novel targeted cancer gene therapy strategy. Cancer Res. 2000, 60, 3435–3439. [Google Scholar]
- Bernstein, J.G.; Garrity, P.A.; Boyden, E.S. Optogenetics and thermogenetics: Technologies for controlling the activity of targeted cells within intact neural circuits. Curr. Opin. Neurobiol. 2012, 22, 61–71. [Google Scholar] [CrossRef] [Green Version]
- Alexandrescu, S.; Korshunov, A.; Lai, S.H.; Dabiri, S.; Patil, S.; Li, R.; Shih, C.S.; Bonnin, J.M.; Baker, J.A.; Du, E.; et al. Epithelioid Glioblastomas and Anaplastic Epithelioid Pleomorphic Xanthoastrocytomas--Same Entity or First Cousins? Brain Pathol. 2016, 26, 215–223. [Google Scholar] [CrossRef] [PubMed]
- Louis, D.N.; Perry, A.; Reifenberger, G.; von Deimling, A.; Figarella-Branger, D.; Cavenee, W.K.; Ohgaki, H.; Wiestler, O.D.; Kleihues, P.; Ellison, D.W. The 2016 World Health Organization Classification of Tumors of the Central Nervous System: A summary. Acta Neuropathol. 2016, 131, 803–820. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Roussakow, S.V. Clinical and economic evaluation of modulated electrohyperthermia concurrent to dose-dense temozolomide 21/28 days regimen in the treatment of recurrent glioblastoma: A retrospective analysis of a two-centre German cohort trial with systematic comparison and effect-to-treatment analysis. BMJ Open 2017, 7, e017387. [Google Scholar] [CrossRef] [Green Version]
- Grech, N.; Dalli, T.; Mizzi, S.; Meilak, L.; Calleja, N.; Zrinzo, A. Rising Incidence of Glioblastoma Multiforme in a Well-Defined Population. Cureus 2020, 12, e8195. [Google Scholar] [CrossRef]
- Tan, A.C.; Ashley, D.M.; Lopez, G.Y.; Malinzak, M.; Friedman, H.S.; Khasraw, M. Management of glioblastoma: State of the art and future directions. CA Cancer J. Clin. 2020, 70, 299–312. [Google Scholar] [CrossRef]
- Oberacker, E.; Kuehne, A.; Oezerdem, C.; Nadobny, J.; Weihrauch, M.; Beck, M.; Zschaeck, S.; Diesch, C.; Eigentler, T.W.; Waiczies, H.; et al. Radiofrequency applicator concepts for thermal magnetic resonance of brain tumors at 297 MHz (7.0 Tesla). Int. J. Hyperth. 2020, 37, 549–563. [Google Scholar] [CrossRef]
- Seebass, M.; Beck, R.; Gellermann, J.; Nadobny, J.; Wust, P. Electromagnetic phased arrays for regional hyperthermia: Optimal frequency and antenna arrangement. Int. J. Hyperth. 2001, 17, 321–336. [Google Scholar] [CrossRef]
- Paulides, M.M.; Curto, S.; Wu, M.; Winter, L.; Rhoon, G.C.v.; Yeo, D.T.B. Advances in magnetic resonance guided radiofrequency hyperthermia. In Proceedings of the 2017 11th European Conference on Antennas and Propagation (EUCAP), Paris, France, 19–24 March 2017; pp. 3692–3696. [Google Scholar]
- Prinz, C.; Starke, L.; Millward, J.M.; Fillmer, A.; Delgado, P.R.; Waiczies, H.; Pohlmann, A.; Rothe, M.; Nazaré, M.; Paul, F.; et al. In vivo detection of teriflunomide-derived fluorine signal during neuroinflammation using fluorine MR spectroscopy. Theranostics 2021, 11, 2490–2504. [Google Scholar] [CrossRef] [PubMed]
- Starke, L.; Millward, J.M.; Prinz, C.; Sherazi, F.; Waiczies, H.; Lippert, C.; Nazaré, M.; Paul, F.; Niendorf, T.; Waiczies, S. First in vivo fluorine-19 magnetic resonance imaging of the multiple sclerosis drug siponimod. Theranostics 2023, 13, 1217–1234. [Google Scholar] [CrossRef]
- Paulides, M.M.; Bakker, J.F.; Neufeld, E.; van der Zee, J.; Jansen, P.P.; Levendag, P.C.; van Rhoon, G.C. Winner of the “New Investigator Award” at the European Society of Hyperthermia Oncology Meeting 2007. The HYPERcollar: A novel applicator for hyperthermia in the head and neck. Int. J. Hyperth. 2007, 23, 567–576. [Google Scholar] [CrossRef]
- Togni, P.; Rijnen, Z.; Numan, W.C.; Verhaart, R.F.; Bakker, J.F.; van Rhoon, G.C.; Paulides, M.M. Electromagnetic redesign of the HYPERcollar applicator: Toward improved deep local head-and-neck hyperthermia. Phys. Med. Biol. 2013, 58, 5997–6009. [Google Scholar] [CrossRef] [PubMed]
- Oberacker, E.; Diesch, C.; Nadobny, J.; Kuehne, A.; Wust, P.; Ghadjar, P.; Niendorf, T. Patient-Specific Planning for Thermal Magnetic Resonance of Glioblastoma Multiforme. Cancers 2021, 13, 1867. [Google Scholar] [CrossRef] [PubMed]
- Winter, L.; Niendorf, T. Electrodynamics and radiofrequency antenna concepts for human magnetic resonance at 23.5 T (1 GHz) and beyond. MAGMA 2016, 29, 641–656. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Winter, L.; Ozerdem, C.; Hoffmann, W.; Santoro, D.; Muller, A.; Waiczies, H.; Seemann, R.; Graessl, A.; Wust, P.; Niendorf, T. Design and evaluation of a hybrid radiofrequency applicator for magnetic resonance imaging and RF induced hyperthermia: Electromagnetic field simulations up to 14.0 Tesla and proof-of-concept at 7.0 Tesla. PLoS ONE 2013, 8, e61661. [Google Scholar] [CrossRef]
- Niendorf, T.; Oezerdem, C.; Ji, Y.; Oberacker, E.; Kuehne, A.; Waiczies, H.; Winter, L. Radiative RF antenna arrays for cardiac, brain and thermal magnetic resonance at ultrahigh and extreme magnetic field strengths: Concepts, electromagnetic field simulations and applications. In Proceedings of the 2017 International Conference on Electromagnetics in Advanced Applications (ICEAA), Verona, Italy, 11–15 September 2017; pp. 1567–1570. [Google Scholar]
- Han, H.; Eigentler, T.W.; Wang, S.; Kretov, E.; Winter, L.; Hoffmann, W.; Grass, E.; Niendorf, T. Design, Implementation, Evaluation and Application of a 32-Channel Radio Frequency Signal Generator for Thermal Magnetic Resonance Based Anti-Cancer Treatment. Cancers 2020, 12, 1720. [Google Scholar] [CrossRef]
- Han, H.; Oberacker, E.; Kuehne, A.; Wang, S.; Eigentler, T.W.; Grass, E.; Niendorf, T. Multi-Channel RF Supervision Module for Thermal Magnetic Resonance Based Cancer Therapy. Cancers 2021, 13, 1001. [Google Scholar] [CrossRef]
- Winter, L.; Oberacker, E.; Paul, K.; Ji, Y.; Oezerdem, C.; Ghadjar, P.; Thieme, A.; Budach, V.; Wust, P.; Niendorf, T. Magnetic resonance thermometry: Methodology, pitfalls and practical solutions. Int. J. Hyperth. 2016, 32, 63–75. [Google Scholar] [CrossRef] [Green Version]
- Davis, R.M.; Viglianti, B.L.; Yarmolenko, P.; Park, J.Y.; Stauffer, P.; Needham, D.; Dewhirst, M.W. A method to convert MRI images of temperature change into images of absolute temperature in solid tumours. Int. J. Hyperth. 2013, 29, 569–581. [Google Scholar] [CrossRef] [Green Version]
- Rieke, V.; Butts Pauly, K. MR thermometry. J. Magn. Reson. Imaging 2008, 27, 376–390. [Google Scholar] [CrossRef]
- Odeen, H.; Parker, D.L. Magnetic resonance thermometry and its biological applications-Physical principles and practical considerations. Prog. Nucl. Magn. Reson. Spectrosc. 2019, 110, 34–61. [Google Scholar] [CrossRef]
- Denis de Senneville, B.; Quesson, B.; Moonen, C.T. Magnetic resonance temperature imaging. Int. J. Hyperth. 2005, 21, 515–531. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Pegah Takook, H.D.T.; Zeng, X.; Fhager, A.; Persson, M. A Computational Study Using Time Reversal Focusing for Hyperthermia Treatment Planning. Prog. Electromagn. Res. B 2017, 73, 117–130. [Google Scholar] [CrossRef] [Green Version]
- Takook, P.; Persson, M.; Gellermann, J.; Trefna, H.D. Compact self-grounded Bow-Tie antenna design for an UWB phased-array hyperthermia applicator. Int. J. Hyperth. 2017, 33, 387–400. [Google Scholar] [CrossRef]
- Takook, P.; Persson, M.; Trefná, H.D. Performance Evaluation of Hyperthermia Applicators to Heat Deep-Seated Brain Tumors. IEEE J. Electromagn. RF Microw. Med. Biol. 2018, 2, 18–24. [Google Scholar] [CrossRef]
- Takook, P.; Shafiemehr, M.; Persson, M.; Trefná, H.D. Experimental evaluation of UWB applicator prototype for head and neck hyperthermia. In Proceedings of the 2017 11th European Conference on Antennas and Propagation (EUCAP), Paris, France, 19–24 March 2017; pp. 3619–3620. [Google Scholar]
- Takook, P.; Trefná, H.D.; Persson, M. Performance evaluation of 2 hyperthermia applicators for deep-seated brain tumors. In Proceedings of the 2017 First IEEE MTT-S International Microwave Bio Conference (IMBIOC), Gothenburg, Sweden, 15–17 May 2017; pp. 1–3. [Google Scholar]
- Trefná, H.D.; Imtiaz, A.; Lui, H.S.; Rubæk, T.; Persson, M. Evolution of an UWB antenna for hyperthermia array applicator. In Proceedings of the 2012 6th European Conference on Antennas and Propagation (EUCAP), Prague, Czech Republic, 26–30 March 2012; pp. 1046–1048. [Google Scholar]
- Zanoli, M.; Ek, E.; Dobšíček Trefná, H. Antenna Arrangement in UWB Helmet Brain Applicators for Deep Microwave Hyperthermia. Cancers 2023, 15, 1447. [Google Scholar] [CrossRef] [PubMed]
- Erturk, M.A.; Raaijmakers, A.J.; Adriany, G.; Ugurbil, K.; Metzger, G.J. A 16-channel combined loop-dipole transceiver array for 7 Tesla body MRI. Magn. Reson. Med. 2017, 77, 884–894. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Woo, M.K.; Delabarre, L.; Lee, B.Y.; Waks, M.; Lagore, R.L.; Radder, J.W.; Eryaman, Y.; Ugurbil, K.; Adriany, G. Evaluation of a 16-Channel Transceiver Loop + Dipole Antenna Array for Human Head Imaging at 10.5 Tesla. IEEE Access 2020, 8, 203555–203563. [Google Scholar] [CrossRef]
- Raaijmakers, A.J.; Luijten, P.R.; van den Berg, C.A. Dipole antennas for ultrahigh-field body imaging: A comparison with loop coils. NMR Biomed. 2016, 29, 1122–1130. [Google Scholar] [CrossRef]
- Lattanzi, R.; Wiggins, G.C.; Zhang, B.; Duan, Q.; Brown, R.; Sodickson, D.K. Approaching ultimate intrinsic signal-to-noise ratio with loop and dipole antennas. Magn. Reson. Med. 2018, 79, 1789–1803. [Google Scholar] [CrossRef]
- Pfrommer, A.; Henning, A. The ultimate intrinsic signal-to-noise ratio of loop- and dipole-like current patterns in a realistic human head model. Magn. Reson. Med. 2018, 80, 2122–2138. [Google Scholar] [CrossRef]
- Hurshkainen, A.; Steensma, B.R.; Glybovski, S.B.; Voogt, I.J.; Melchakova, I.V.; Belov, P.A.; Berg, C.A.T.v.d.; Raaijmakers, A.J.E. On Optimization of Radiative Dipole Body Array Coils for 7 Tesla MRI. arXiv 2017, arXiv:1710.02399. [Google Scholar]
- Erturk, M.A.; Wu, X.; Eryaman, Y.; Van de Moortele, P.F.; Auerbach, E.J.; Lagore, R.L.; DelaBarre, L.; Vaughan, J.T.; Ugurbil, K.; Adriany, G.; et al. Toward imaging the body at 10.5 tesla. Magn. Reson. Med. 2017, 77, 434–443. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Eryaman, Y.; Guerin, B.; Keil, B.; Mareyam, A.; Herraiz, J.L.; Kosior, R.K.; Martin, A.; Torrado-Carvajal, A.; Malpica, N.; Hernandez-Tamames, J.A.; et al. SAR reduction in 7T C-spine imaging using a ”dark modes“ transmit array strategy. Magn. Reson. Med. 2015, 73, 1533–1539. [Google Scholar] [CrossRef] [Green Version]
- Lagore, R.L.; Moeller, S.; Zimmermann, J.; DelaBarre, L.; Radder, J.; Grant, A.; Ugurbil, K.; Yacoub, E.; Harel, N.; Adriany, G. An 8-dipole transceive and 24-loop receive array for non-human primate head imaging at 10.5 T. NMR Biomed. 2021, 34, e4472. [Google Scholar] [CrossRef]
- Prasad, B.; Kim, J.K.; Kim, S. Role of Simulations in the Treatment Planning of Radiofrequency Hyperthermia Therapy in Clinics. J. Oncol. 2019, 2019, 9685476. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Foundation, I.I. Virtual Population (ViP) Models:DUKE. Available online: https://itis.swiss/virtual-population/virtual-population/overview/ (accessed on 1 January 2022).
- Zanoli, M.; Trefna, H.D. Iterative time-reversal for multi-frequency hyperthermia. Phys. Med. Biol. 2021, 66, 045027. [Google Scholar] [CrossRef]
- Lu, Y.; Li, B.; Xu, J.; Yu, J. Dielectric properties of human glioma and surrounding tissue. Int. J. Hyperth. 1992, 8, 755–760. [Google Scholar] [CrossRef]
- Hasgall, P.A.; Di Gennaro, F.; Baumgartner, C.; Neufeld, E.; Lloyd, B.; Gosselin, M.C.; Payne, D.; Klingenböck, A.; Kuster, N. IT’IS Database for Thermal and Electromagnetic Parameters of Biological Tissues; IT’IS Foundation: Zurich, Switzerland, 2022. [Google Scholar] [CrossRef]
- Eigentler, T.W.; Winter, L.; Han, H.; Oberacker, E.; Kuehne, A.; Waiczies, H.; Schmitter, S.; Boehmert, L.; Prinz, C.; Trefna, H.D.; et al. Wideband Self-Grounded Bow-Tie Antenna for Thermal MR. NMR Biomed. 2020, 33, e4274. [Google Scholar] [CrossRef] [Green Version]
- Rijnen, Z.; Togni, P.; Roskam, R.; van de Geer, S.G.; Goossens, R.H.; Paulides, M.M. Quality and comfort in head and neck hyperthermia: A redesign according to clinical experience and simulation studies. Int. J. Hyperth. 2015, 31, 823–830. [Google Scholar] [CrossRef] [Green Version]
- Van der Gaag, M.L.; De Bruijne, M.; Samaras, T.; Van der Zee, J.; Van Rhoon, G.C. Development of a guideline for the water bolus temperature in superficial hyperthermia. Int. J. Hyperth. 2006, 22, 637–656. [Google Scholar] [CrossRef]
- Jin-Yuan, C.; Gandhi, O.P. Numerical simulation of annular-phased arrays of dipoles for hyperthermia of deep-seated tumors. IEEE Trans. Biomed. Eng. 1992, 39, 209–216. [Google Scholar] [CrossRef] [PubMed]
- Roemer, P.B.; Edelstein, W.A.; Hayes, C.E.; Souza, S.P.; Mueller, O.M. The NMR phased array. Magn. Reson. Med. 1990, 16, 192–225. [Google Scholar] [CrossRef]
- Kuehne, A.; Goluch, S.; Waxmann, P.; Seifert, F.; Ittermann, B.; Moser, E.; Laistler, E. Power balance and loss mechanism analysis in RF transmit coil arrays. Magn. Reson. Med. 2015, 74, 1165–1176. [Google Scholar] [CrossRef]
- Graessl, A.; Renz, W.; Hezel, F.; Dieringer, M.A.; Winter, L.; Oezerdem, C.; Rieger, J.; Kellman, P.; Santoro, D.; Lindel, T.D.; et al. Modular 32-channel transceiver coil array for cardiac MRI at 7.0T. Magn. Reson. Med. 2014, 72, 276–290. [Google Scholar] [CrossRef] [PubMed]
- 60601-2-33:2010; Medical Electrical Equipment-Part 2-33: Particular Requirements for the Basic Safety and Essential Performance of Magnetic Resonance Equipment for Medical Diagnosis. IEC: Genève, Switzerland, 2015. Available online: https://mriquestions.com/uploads/3/4/5/7/34572113/safety_iec_60601-2-33previews_1897819_pre.pdf (accessed on 30 November 2022).
- Kuehne, A.; Oberacker, E.; Waiczies, H.; Niendorf, T. Solving the Time- and Frequency-Multiplexed Problem of Constrained Radiofrequency Induced Hyperthermia. Cancers 2020, 12, 1072. [Google Scholar] [CrossRef] [PubMed]
- Kok, H.P.; Kotte, A.; Crezee, J. Planning, optimisation and evaluation of hyperthermia treatments. Int. J. Hyperth. 2017, 33, 593–607. [Google Scholar] [CrossRef] [Green Version]
- Jha, S.; Sharma, P.K.; Malviya, R. Hyperthermia: Role and Risk Factor for Cancer Treatment. Achiev. Life Sci. 2016, 10, 161–167. [Google Scholar] [CrossRef] [Green Version]
- Tilly, W.; Wust, P.; Rau, B.; Harder, C.; Gellermann, J.; Schlag, P.; Budach, V.; Felix, R. Temperature data and specific absorption rates in pelvic tumours: Predictive factors and correlations. Int. J. Hyperth. 2001, 17, 172–188. [Google Scholar] [CrossRef]
- Oh, S.; Ryu, Y.C.; Carluccio, G.; Sica, C.T.; Collins, C.M. Measurement of SAR-induced temperature increase in a phantom and in vivo with comparison to numerical simulation. Magn. Reson. Med. 2014, 71, 1923–1931. [Google Scholar] [CrossRef] [Green Version]
- Li, Z.; Vogel, M.; Maccarini, P.F.; Stakhursky, V.; Soher, B.J.; Craciunescu, O.I.; Das, S.; Arabe, O.A.; Joines, W.T.; Stauffer, P.R. Improved hyperthermia treatment control using SAR/temperature simulation and PRFS magnetic resonance thermal imaging. Int. J. Hyperth. 2011, 27, 86–99. [Google Scholar] [CrossRef] [Green Version]
- Kok, H.P.; Schooneveldt, G.; Bakker, A.; de Kroon-Oldenhof, R.; Korshuize-van Straten, L.; de Jong, C.E.; Steggerda-Carvalho, E.; Geijsen, E.D.; Stalpers, L.J.A.; Crezee, J. Predictive value of simulated SAR and temperature for changes in measured temperature after phase-amplitude steering during locoregional hyperthermia treatments. Int. J. Hyperth. 2018, 35, 330–339. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Paulides, M.M.; Rodrigues, D.B.; Bellizzi, G.G.; Sumser, K.; Curto, S.; Neufeld, E.; Montanaro, H.; Kok, H.P.; Dobsicek Trefna, H. ESHO benchmarks for computational modeling and optimization in hyperthermia therapy. Int. J. Hyperth. 2021, 38, 1425–1442. [Google Scholar] [CrossRef] [PubMed]
- Bellizzi, G.G.; Drizdal, T.; van Rhoon, G.C.; Crocco, L.; Isernia, T.; Paulides, M.M. Predictive value of SAR based quality indicators for head and neck hyperthermia treatment quality. Int. J. Hyperth. 2019, 36, 456–465. [Google Scholar] [CrossRef] [Green Version]
- Canters, R.A.; Wust, P.; Bakker, J.F.; Van Rhoon, G.C. A literature survey on indicators for characterisation and optimisation of SAR distributions in deep hyperthermia, a plea for standardisation. Int. J. Hyperth. 2009, 25, 593–608. [Google Scholar] [CrossRef] [PubMed]
- Kok, H.P.; van der Zee, J.; Guirado, F.N.; Bakker, A.; Datta, N.R.; Abdel-Rahman, S.; Schmidt, M.; Wust, P.; Crezee, J. Treatment planning facilitates clinical decision making for hyperthermia treatments. Int. J. Hyperth. 2021, 38, 532–551. [Google Scholar] [CrossRef]
- Zanoli, M.; Trefna, H.D. Suitability of eigenvalue beam-forming for discrete multi-frequency hyperthermia treatment planning. Med. Phys. 2021, 48, 7410–7426. [Google Scholar] [CrossRef] [PubMed]
- Bruggmoser, G. Some aspects of quality management in deep regional hyperthermia. Int. J. Hyperth. 2012, 28, 562–569. [Google Scholar] [CrossRef]
- Jaffar, N.A.; Lias, K.B.; Madzhi, N.K.; Buniyamin, N. An overview of metamaterials used in applicators in hyperthermia cancer treatment procedure. In Proceedings of the 2017 International Conference on Electrical, Electronics and System Engineering (ICEESE), Kanazawa, Japan, 9–10 November 2017; pp. 32–36. [Google Scholar]
- Wang, G.; Gong, Y. Metamaterial lens applicator for microwave hyperthermia of breast cancer. Int. J. Hyperth. 2009, 25, 434–445. [Google Scholar] [CrossRef]
- Velazquez-Ahumada, M.C.; Freire, M.J.; Marques, R. Metamaterial applicator for microwave hyperthermia. In Proceedings of the 2011 XXXth URSI General Assembly and Scientific Symposium, Istanbul, Turkey, 13–20 August 2011; pp. 1–4. [Google Scholar]
- Schmidt, R.; Webb, A. Metamaterial Combining Electric- and Magnetic-Dipole-Based Configurations for Unique Dual-Band Signal Enhancement in Ultrahigh-Field Magnetic Resonance Imaging. ACS Appl. Mater. Interfaces 2017, 9, 34618–34624. [Google Scholar] [CrossRef]
- Webb, A.; Shchelokova, A.; Slobozhanyuk, A.; Zivkovic, I.; Schmidt, R. Novel materials in magnetic resonance imaging: High permittivity ceramics, metamaterials, metasurfaces and artificial dielectrics. MAGMA 2022, 35, 875–894. [Google Scholar] [CrossRef]
- Chen, H.; Guo, L.; Li, M.; Destruel, A.; Liu, C.; Weber, E.; Liu, F.; Crozier, S. Metamaterial-Inspired Radiofrequency (RF) Shield With Reduced Specific Absorption Rate (SAR) and Improved Transmit Efficiency for UHF MRI. IEEE Trans. Biomed. Eng. 2021, 68, 1178–1189. [Google Scholar] [CrossRef] [PubMed]
- Paulides, M.M.; Stauffer, P.R.; Neufeld, E.; Maccarini, P.F.; Kyriakou, A.; Canters, R.A.; Diederich, C.J.; Bakker, J.F.; Van Rhoon, G.C. Simulation techniques in hyperthermia treatment planning. Int. J. Hyperth. 2013, 29, 346–357. [Google Scholar] [CrossRef] [PubMed]
- Drizdal, T.; van Rhoon, G.C.; Verhaart, R.F.; Fiser, O.; Paulides, M.M. A Guide for Water Bolus Temperature Selection for Semi-Deep Head and Neck Hyperthermia Treatments Using the HYPERcollar3D Applicator. Cancers 2021, 13, 6126. [Google Scholar] [CrossRef] [PubMed]
- Katscher, U.; van den Berg, C.A.T. Electric properties tomography: Biochemical, physical and technical background, evaluation and clinical applications. NMR Biomed. 2017, 30, e3729. [Google Scholar] [CrossRef] [PubMed]












| ThermalMR RF Applicator | Individual Excitation Mode (M) Power | ||||
|---|---|---|---|---|---|
| 16LDcir | 300 MHz | 350 MHz | 450 MHz | 450 MHz | Total |
| 0.65 W | 31.48 W | 24.01 W | 15.12 W | 71.26 W | |
| 16LDcir_HS | 350 MHz | 450 MHz | 450 MHz | Total | |
| 21.33 W | 34.21 W | 15.23 W | 70.77 W | ||
| 16LDellip | 300 MHz | 350 MHz | 450 MHz | 450 MHz | Total |
| 14.55 W | 15.84 W | 22.72 W | 18.21 W | 71.32 W | |
| 16LDellip_HS | 350 MHz | 450 MHz | 450 MHz | Total | |
| 18.89 W | 32.66 W | 18.75 W | 70.3 W | ||
| ThermalMR RF Applicator | Mean 7 T | Max 7 T | Min 7 T | * p-Value (vs. 16LD) 7 T | Mean 9.4 T | Max 9.4 T | Min 9.4 T | * p-Value (vs. 16LD) 9.4 T | Mean 10.5 T | Max 10.5 T | Min 10.5 T | * p-Value (vs. 16LD) 10.5 T | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| cir | 16LD | 19.42 | 21.39 | 16.14 | 20.87 | 24.74 | 15.26 | 21.25 | 26.18 | 13.90 | |||
| 8D | 12.89 | 14.63 | 10.27 | 1.05 × 10−83 | 16.18 | 19.07 | 10.83 | 8.42 × 10−70 | 17.26 | 21.30 | 10.23 | 1.56 × 10−43 | |
| 8L | 14.63 | 16.26 | 12.28 | 1.09 × 10−83 | 13.4 | 16.10 | 9.72 | 3.33 × 10−83 | 12.69 | 15.86 | 8.79 | 5.70 × 10−82 | |
| cir_HS | 16LD | 18.33 | 20.22 | 14.69 | 20.01 | 24.06 | 14.02 | 20.33 | 24.70 | 12.94 | |||
| 8D | 14.36 | 16.03 | 10.80 | 3.23 × 10−80 | 16.82 | 20.14 | 11.08 | 3.61 × 10−46 | 16.84 | 20.96 | 10.16 | 9.48 × 10−34 | |
| 8L | 11.57 | 12.69 | 9.90 | 1.03 × 10−83 | 11.86 | 14.06 | 8.63 | 1.07 × 10−83 | 11.51 | 14.11 | 7.78 | 3.80 × 10−83 | |
| ellip | 16LD | 19.77 | 21.95 | 16.66 | 20.03 | 23.82 | 14.80 | 20.40 | 25.20 | 13.53 | |||
| 8D | 12.95 | 14.54 | 10.71 | 1.05 × 10−83 | 15.99 | 18.52 | 11.30 | 9.25 × 10−65 | 17.04 | 20.64 | 10.66 | 1.71 × 10−36 | |
| 8L | 15.07 | 16.78 | 12.17 | 1.31 × 10−83 | 12.41 | 15.22 | 8.34 | 2.04 × 10−83 | 11.70 | 15.03 | 7.16 | 2.34 × 10−82 | |
| ellip_HS | 16LD | 18.37 | 20.47 | 14.48 | 19.74 | 23.44 | 13.85 | 20.66 | 25.54 | 13.47 | |||
| 8D | 14.11 | 15.52 | 10.93 | 8.13 × 10−82 | 16.43 | 19.18 | 10.99 | 1.31 × 10−49 | 17.29 | 21.20 | 10.61 | 3.08 × 10−34 | |
| 8L | 11.89 | 13.83 | 8.72 | 1.05 × 10−83 | 11.51 | 13.99 | 7.44 | 1.11 × 10−83 | 11.77 | 14.92 | 7.21 | 4.94 × 10−82 | |
| ThermalMR RF Applicator | Mean | Max | Min | * p-Value (vs. 16LD) | |
|---|---|---|---|---|---|
| cir | 16LD | 34.1 | 40.4 | 22.9 | |
| 8D | 27.1 | 38.8 | 12.4 | 5.32 × 10−5 | |
| 8L | 10.8 | 24.2 | 1.33 | 3.96 × 10−8 | |
| cir_HS | 16LD | 34.7 | 40.4 | 20.3 | |
| 8D | 30.9 | 40.3 | 17.3 | 6.64 × 10−5 | |
| 8L | 5.57 | 12.9 | 0.712 | 1.18 × 10−7 | |
| ellip | 16LD | 33.6 | 40.6 | 20.5 | |
| 8D | 25.0 | 35.4 | 10.5 | 5.85 × 10−5 | |
| 8L | 9.14 | 19.3 | 1.47 | 3.52 × 10−7 | |
| ellip_HS | 16LD | 34.4 | 40.9 | 20.3 | |
| 8D | 30.1 | 40.6 | 17.2 | 1.9 × 10−3 | |
| 8L | 7.69 | 18.1 | 1.15 | 1.56 × 10−7 | |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Saha, N.; Kuehne, A.; Millward, J.M.; Eigentler, T.W.; Starke, L.; Waiczies, S.; Niendorf, T. Advanced Radio Frequency Applicators for Thermal Magnetic Resonance Theranostics of Brain Tumors. Cancers 2023, 15, 2303. https://doi.org/10.3390/cancers15082303
Saha N, Kuehne A, Millward JM, Eigentler TW, Starke L, Waiczies S, Niendorf T. Advanced Radio Frequency Applicators for Thermal Magnetic Resonance Theranostics of Brain Tumors. Cancers. 2023; 15(8):2303. https://doi.org/10.3390/cancers15082303
Chicago/Turabian StyleSaha, Nandita, Andre Kuehne, Jason M. Millward, Thomas Wilhelm Eigentler, Ludger Starke, Sonia Waiczies, and Thoralf Niendorf. 2023. "Advanced Radio Frequency Applicators for Thermal Magnetic Resonance Theranostics of Brain Tumors" Cancers 15, no. 8: 2303. https://doi.org/10.3390/cancers15082303
APA StyleSaha, N., Kuehne, A., Millward, J. M., Eigentler, T. W., Starke, L., Waiczies, S., & Niendorf, T. (2023). Advanced Radio Frequency Applicators for Thermal Magnetic Resonance Theranostics of Brain Tumors. Cancers, 15(8), 2303. https://doi.org/10.3390/cancers15082303