1. Introduction
Engineered skeletal muscle substitutes are needed to treat the consequences of muscular trauma or disorders that result in loss of muscle parenchyma. Large defects cannot be compensated by the innate regenerative capacity of the muscle [
1]. Muscle architecture is unique: it comprises of parallel-aligned myofibers held together by the structure and composition of the surrounding extracellular matrix (ECM).
The extracellular matrix of muscle consists of two layers, the basal lamina, which is in close contact to the cells by binding to the integrin receptors protruding from the cellular plasma membrane, and the fibrillar reticular lamina, which surrounds the cells. The basal lamina consists of the non-fibrillar collagen type IV, laminin, and proteoglycans. Below this dense basal lamina, the fibrillar reticular lamina resides, which corresponds to the interstitial connective tissue comprising mainly of (fibrillar) collagens, e.g., collagen I and proteoglycans [
2,
3,
4]. Laminin and collagen IV are the most abundant in the basal lamina [
2] while fibronectin is present in and between basal lamina. During muscle regeneration, basal lamina-based Laminin enhances proliferation and differentiation of myoblasts [
2,
5]. The strict physical separation of the spatially randomly organized basal membrane and the interstitial ECM in which the molecules are organized in the (linear) direction of the muscle’s contraction, warrants to investigate topographic designs for skeletal muscle tissue engineering. This is irrespective of the scaffold material whether this is synthetic polymer or natural ECM-based.
A dense network of capillaries that contact myofibers, only separated by the basal membrane, perfuses muscle. In vitro, topography guides cellular behavior such as the proliferation and differentiation of myoblasts [
6,
7,
8,
9,
10,
11]. We showed, by using innovative PDMS-based topography gradient substrates, that, in vitro, in micrometer-sized linear substrate topographies, parallel aligned myotubes are induced during differentiation of muscle stem cells (satellite cells) [
12]. Human myoblasts can align to a variety of features but the one that most closely resembles the native myotubes diameter of 100 µm [
13] is a sinusoidal directional pattern of 10-µm wavelength with an average myotube diameters of 66 ± 59 µm [
12]. The interaction between human myoblasts and endothelial cells in an aligned topography is pertinent for more sophisticated and functional skeletal muscle engineering but has not yet been adequately studied [
14,
15,
16]. We recently published that also vascular endothelial cells prefer linear topographies for proliferation over flat surfaces while network formation did not follow linear topography [
17]. This was expected, because networks are interconnected endothelial with a honeycomb appearance in vitro as well as in vivo.
Besides topographical cues, cellular plasticity is influenced by biochemical cues such as provided by the extracellular matrix, e.g., integrin motifs in the basal lamina, as discussed above. By virtue of their pericytic nature, mesenchymal stem cells (MSC) such as adipose tissue-derived stromal cells (ASCs) stimulate formation of vascular networks from seeded endothelial cells [
18]. This process depends on cell-to-cell contacts between ASC and endothelial cells in Notch-mediated fashion [
19]. We previously showed that ASCs deposit two pivotal ECM components, the basal membrane constituent’s collagen IV and also fibronectin that are essential to initiate vasculogenesis [
20]. Satellite cells, i.e., the muscle’s endogenous MSCs that are also muscle stem cells, are activated after damage to facilitate regeneration. During muscle regeneration, angiogenesis and myogenesis coincide [
21]. The local ischemia that occurs after damage causes myotubes to secrete pro-angiogenic factors such as vascular endothelial growth factor (VEGF) and hepatocyte growth factor (HGF) [
21,
22,
23]. Before and after myoblast differentiation, extracellular matrix components are deposited. In fact, this is highest during differentiation, which indicates that ECM is being remodeled while myofibers are formed [
23].
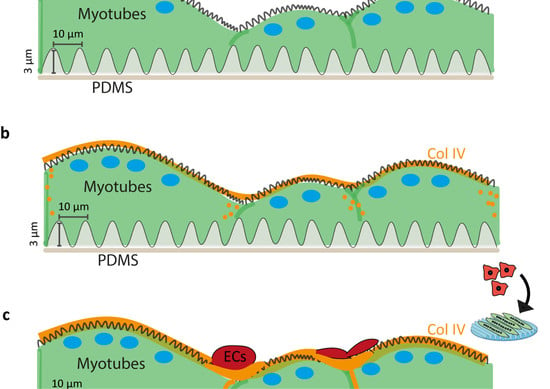
In tissue, a basal membrane surrounds the capillaries. Thus, we hypothesized that muscle stem cells and their derived myotubes support adhesion and network formation of endothelial cells. Topography-mediated aligned myotubes would facilitate formation of co-aligned capillary networks from endothelial cells. Understanding an in vitro system including the influence of the topography, composition, and biochemical cues interacting in the system is useful to guide tissue development and create a substitute suitable for patients.
3. Results
The directional topography made by plasma surface oxidation of PDMS showed sinusoidal features of 10.3 ± 0.2-µm wavelength and 3.4 ± 0.1-µm amplitude (
Figure 2a). This feature was previously identified by us to support alignment and differentiation of myoblasts to myotubes most optimal and was therefore used as the foundation in this study [
12]. Topography of aligned myotubes was measured by AFM to uncover the topography influence of the substrate on the structure of the myotube surface. AFM analyses of differentiated myoblasts showed that these covered both the TCP and the PDMS topography (
Figure 2b–d). Myotube alignment can be observed once compared with the flat TCP surface (
Figure 2b). Myotube topography resulted in nanotopography at the cell surface with aligned protruding dents of approximately 300–900 nm in width and 10–100 nm in height parallel to the length of the myotubes (
Figure 2c,d). In addition, microtopography was observed corresponding to the myotube diameters, 1–2 µm in amplitude and 20–60 µm in diameter, at the intersection with neighboring myotubes (
Figure 2c).
Myotubes and ECs attached to the directional topography (
Figure 3) while adhering poorly to flat PDMS and readily detached within five days, which was only marginally improved by prior coating with gelatin [
12]. On gelatin-coated flat PDMS, myotubes continued to form, yet seemed to aggregate, for eight days (
Figure 3a,b). ECs attached and proliferated on both flat and structured PDMS after two days. Directional topography caused cells to align (
Figure 3c). After five days on flat PDMS, ECs had detached and formed aggregates, whereas the ECs on the directional topography remain aligned (
Figure 3d), which corroborates our earlier findings on mixed topographies that ECs tend to detach and aggregate [
17].
After two days of co-culture, endothelial cells readily attached and followed the myotubes directionality irrespective of the underlying substrate (
Figure 4a). Although ECs adhered and proliferated (
Figure 4b) on top of the myotubes on all surfaces, no visible network formation was observed during the follow up time. Flat PDMS showed myotube differentiation and subsequent detachment, as we previously observed [
12].
Besides adhering to the myotubes, ECs had an elongated tube-shape morphology following the myotubes’ directionality as shown by confocal laser scanning microscopy (
Figure S1a,b). In addition, fibronectin, an instructive protein required for vessel formation and stabilization, was expressed in co-cultured myotubes with ECs surrounding these cells. Interestingly, fibronectin was most strongly expressed at the contact points between myotubes and ECs (
Figure S1b).
We assessed gene expression (see the
Supplementary Materials) of myotubes, ECs, and their co-cultures, to explore the influence of the topography and culture conditions (mono- vs. co-culture) over time to identify whether they would have a stimulating or inhibiting effect on the possible functions needed to create a stabilizing environment for vascular network formation. Irrespective of topography, both monocultures of ECs and myotubes as well as their co-cultures had readily detectable expression of all genes assessed except for
VEGFA. Unexpectedly,
VEFGA was not expressed by monocultured myotubes. In addition,
VEGFA in ECs decreased in a substrate-dependent fashion. After five days of culture, ECs on TCP showed higher gene expression than those on the directional topography (one-way ANOVA
p = 0.0404, Tukey’s multiple comparison test). Vessel formation relies on the stimulation of ECs by the product of
ANGPT2 (encoding angiopoietin 2) expression (besides
VEGFA expression). Indeed,
ANGPT2 expression was detectable and decreased during co-culture (paired t test
p = 0.00663). Upon their formation, endothelial capillary tubes rely on stabilization by pericytic action. Indicative would be expression of
ANGPT1, which was confirmed in co-cultures and myotubes, yet also lower at five days compared to two days (
p = 0.0007). In vascularization processes, ECs express
PDGFB and secrete PDGF-BB to attract pericytes for their stabilization. Indeed, ECs monocultures showed (increased) expression of
PDGFB (
p = 0.0334) as did co-cultures over time (
p = 0.0154). Secreted paracrine factors tend to change more than cell-bound markers. This was corroborated by absence of change in expression of the (pericytic) receptor for PDGF-BB (i.e.,
PDGFRB) or pericyte marker, the HSPG NG2 encoded by
CSGP4. Expression of established endothelial-specific genes such as
CDH5 and
PECAM1 either did not change (
CDH5) or decreased such as for
PECAM1 on flat substrate co-cultures (one-way ANOVA
p = 0.0432, Tukey’s multiple comparison test).
Additionally, protein production and organization of the myoblasts and myotubes was assessed on TCP to identify the ECM proteins that promote attachment of endothelial cells and support formation of tube-like structures. Myoblasts and myotubes had a similar behavior in protein deposition on TCP (
Figure S3). Fibronectin was poorly expressed by myoblasts and myotubes. Basal lamina proteins collagen type IV and laminin were deposited by myoblasts and myotubes. Constructive, interstitial matrix, fibrous protein collagen type I was lowly expressed by myoblasts and myotubes while it was deposited in a patchy pattern. This was expected, because collagen I is usually deposited by professional connective tissue cells, i.e., fibroblasts. In contrast, collagen III was highly expressed in both cases (myoblast and myotubes). Similarly, collagen IV and laminin were present in the cytoplasm of myoblasts and deposited around myotubes. Thus, in vitro, muscle stem cells (myoblasts) appear to accumulate these ECM proteins in an intracytoplasmic manner while these are deposited upon their differentiation to myotubes.
The ECM was deposited following the directionality of the myotubes irrespective of the substrate. Thus, in the case of myotube alignment due to topography, the deposition of the extracellular components also followed the aligned directionality. The myotube deposited laminin, fibronectin and collagens mainly parallel to the myotubes with occasional perpendicular fibers creating a mesh-like structure (
Figure 5a,b and
Figure S4a). The co-culture with ECs did not influence this pattern of ECM deposition irrespective of substrate (
Figure 5). However, the areas where ECs and myotubes were in contact had a higher deposition of ECM proteins. Fibronectin and collagen I were lowly expressed but their deposition patterns followed the cells’ directionality. Collagens III and IV showed deposition patterns similar to fibronectin and collagen I. Laminin deposition was similar too, yet more abundant than the other ECM components while it covered the entire surface of all the substrates.
Expression analyses of genes for ECM components corroborated the protein expression data for
LAMA1 (
Figure 5c). Myotube monocultures and co-cultures with ECs showed
LAMA1 expression increased by two-fold change (paired t-test
p = 0.0307 and
p = 0.0410) between the two-day co-culture (five-day-old myotubes) and five-day co-culture (seven-day-old myotubes). Myotubes’ monoculture showed low gene expression of
FN1 after five days of differentiation (two days of co-culture). Expression of
FN1 and
COL4A1 was below detection level in myotubes (
Figure 5d,e).
FN1 expression was only detected on seven-day-old myotubes on flat PDMS and TCP. This low gene expression was also reflected in the co-cultures.
COL4A1 expression was undetectable in the myotube monocultures (
Figure 5d) while this protein had been deposited as shown by immunofluorescence (
Figure 5a and
Figure S4a). ECs and their co-culture with myotubes showed a decreased
COL4A1 expression from two to five days of co-culture (paired t-test
p = 0.0052 and
p = 0.0159 respectively). Maturation of myotubes was not affected by the co-cultures (
Figure S4b) as shown by expression of
MYH1 and
MYH2. However, in myotube monocultures
MYH2 expression decreased from five-day-old myotubes to seven-day myotubes (paired t-test
p = 0.0260).
Monocultures of ECs and ASCs (positive control for deposition of ECM proteins [
20]) on the flat control (PDMS), TCP, and the directional topography (
Figure 6) showed that topography also influenced their alignment. ASCs and ECs deposited proteins in an aligned manner following the cells’ directionality on the topography similar to the myotubes (
Figure 6).
The ECM expression of the different ECM components was compared to the myotubes (
Figure 6b) to identify cell type-specific deposition patterns. The deposition of ECM by ECs or ASCs on a flat and stiff substrate (TCP) was reduced compared to myotubes in most cases. Except for ASCs, which had a deposition of collagen type I with a near 50% increase and fibronectin with a 30% increase. On the other hand, collagen type I deposition by ECs on TCP was almost 50% reduced compared to myotubes. On the directional topographies, ECs and ASCs deposited less of all ECM proteins compared to myotubes except for fibronectin by ASCs. Fibronectin is relevant in early angiogenesis and was 20% less deposited by ECs than by myotubes, while ASCs deposited almost 15% more than myotubes under similar substrate conditions. For the deposition of the basal lamina component, laminin deposition was around 30% lower for ECs and ASCs compared to myotubes.
On the flat PDMS control, the different monocultures of myotubes, ASCs, ECs, and the co-culture (myotubes plus ECs) attached poorly to the surface (
Figure S5a). The cells detached within two days and formed aggregates. However, these aggregates also produced ECM proteins that negatively affected our fluorescence densitometric readings. Thus, ECM deposition on flat PDMS was unreliable and unusable as control for comparisons. These results show once more the positive influence of the directional topography on cell attachment.
Myotube monocultures had a different fibronectin deposition pattern than the co-cultures in which fibronectin was mostly deposited on top of the myotube surface and in the surroundings of the ECs (
Figure 7a,b). Laminin surrounded the myotubes and its deposition was similar for both, the myotubes monoculture and the co-culture (
Figure 7c,d). Monocultured myotubes showed a distinct punctuated peripheral deposition of collagen IV (
Figure 7e). In addition, collagen IV was deposited basally and apically by myotubes. The co-culture of ECs and myotubes showed a more homogeneous collagen IV deposition with higher punctuated deposits at contacts between ECs and myotubes (
Figure 7f). Myotube monocultures had deposited collagen III surrounding them, but, apically, the deposition was higher (
Figure 7g). The co-culture of ECs and myotubes showed comparable deposition patterns of collagen III as myotube mono-cultures (
Figure 7h). Finally, collagen I deposition was similar in both monoculture of myotubes and co-culture of ECs and myotubes, but in co-cultures collagen I deposits were more intense at contact points of ECs on the myotube surface (
Figure 7i,j).
After characterizing the deposition of the different ECM components by the myotubes and the co-culture with ECs on our directional topography substrate, we compared them with adult human (ocular) muscle tissue and assessed the histology of the vasculature and the ECM organization.
In ocular muscle, capillary vessels were surrounding or traversing the human myotubes, as shown by CD31, endocan, and MHC1 staining (
Figure S6). Most of the vasculature was found in the interstitial tissue (
Figure S6b,c). MHC1 showed moderate expression and varied across individual fibers as depicted by the difference of the intensity in green (immunofluorescence staining) or brown (DAB staining). This relates to the twitching type of fibers in these muscles (fast versus slow).
Fibronectin and collagen I were located in the interstitial tissue of the myotubes (
Figure 8). Small capillaries connected the myotubes, as shown by the arrow on the fibronectin panel (
Figure 8), but larger vessels were in the interstitial connective tissue rich in fibronectin and collagen I. The basal lamina constituent collagen IV covered the periphery of the myotubes and was abundantly present around vessel walls (
Figures S7 and S8). Perilipin and PicroSirus Red staining confirmed that the interstitial tissue was not adipose tissue surrounding the muscle fibers but collagen fibers and fibronectin (
Figures S8–S10). Although we used anti-perilipin antibodies to visualize adipocytes, the striated muscle itself was also stained [
28]. This is due to the antibody recognizing multiple forms of perilipin and because, in recent years, presence of perilipins in muscle is described too. Collagen III was also present in the interstitial tissue (
Figure S7).
4. Discussion
In this study, we showed that a topographical system with aligned myotubes facilitates and sustains adhesion and proliferation of endothelial cells through deposition of organized basal membrane proteins, such as collagen IV and laminin, and constructive ECM proteins, such as collagens I and III. A second result is that topography-guided myotubes did not promote maturation of adhered ECs and primitive tubes to a well-stabilized vascular-like network. The vessel-instructive protein, fibronectin, was deposited by myotubes to a lesser extend compared to a professional mesenchymal tissue-remodeling control (ASCs), yet showed to be aligned following the directionality of the topography. Fibronectin alignment by topography has been reported for C2C12 murine myoblasts in a nanotopography system [
29]. In addition, topographical systems have been created by ECM proteins guiding the cell alignment of skeletal muscle cells [
8,
9,
16]. Other substrates have been used for the co-culture and alignment of myoblasts and ECs [
15,
16]. However, to our knowledge, an investigation of the ECM proteins secreted by aligned myotubes, and in co-culture with ECs in a topographical system, has not been described yet.
We observed an effect over time for some genes indifferently of the material and topography. Genes related with vascularization,
ANG2 and
PECAM1, were downregulated over time in the co-cultures.
PDGFB was downregulated by the ECs, and in co-culture it was upregulated. Increase of expression of
PDGFB in the co-culture means that the cell–cell interactions are leading to a pre-vascularization process where remaining satellite cells are being activated mimicking an injury process and endothelial cells express this marker to recruit pericytes [
30]. We only detected that the gene expression was affected by the topography at Day 5 of culture of ECs, where the
VEGFA expression was downregulated in the directional topography compared to TCP. ECs on the topography had different cell spreading and morphology. In the PDMS directional topography, ECs aligned and proliferated, whereas, in the flat PDMS, ECs firstly formed honeycomb-like structure, which later formed aggregates.
Our system produces lower amounts of fibronectin as a monoculture as compared to the co-cultures, i.e., influenced by cell–cell interactions. Virtually no published data exist on the deposition and function of fibronectin by human myoblasts or myotubes. This is relevant because, in clinical perspective, studies with, e.g., murine C2C12 myoblasts, rat L6E9 myoblasts, or otherwise, mammalian or avian myoblasts showed to differ from their human counterparts in many aspects. Almost four decades ago, others showed that in vitro the rate of fibronectin biosynthesis was about five-fold lower in primary chicken muscle cells than chicken fibroblasts [
31]. More recently, fibronectin was shown to be deposited locally by primary murine myotubes to facilitate peripheral arrangement of nuclei in the myotubes’ syncytium. Besides, in vitro muscle cells require a supportive system to develop the necessary ECM for the muscular function and maintenance [
32]. Skeletal muscle myotubes need the cells residing in the surroundings. These cells are satellite cells, fibroblasts, myofibroblasts, adipose cells, and fibro/adipogenic progenitor cells (FAP) [
33]. Therefore, myotubes need cell–cell contact to remodel the matrix [
34] and perhaps fibroblasts are needed in our system because they are the skeletal muscle assemblers of collagens [
32]. In addition, constant matrix remodeling was depicted by our gene expression results where fibronectin was not expressed in some experiments.
Previous studies have shown that C2C12 murine myoblasts deposit various ECM constituents such as collagens I and IV and fibronectin on etched glass [
35]. This fibronectin deposition occurred already after 3.5 h of culture and the distribution of the proteins followed the directionality of the cells. In our system, we also observed that fibronectin was deposited following cells’ directionality and that more fibronectin was deposited at the interface of myotubes and ECs. Fibronectin is found on the interstitial ECM [
36,
37], which was confirmed with the evaluation of the human muscle sample where we observed that most of the endothelial cell population was in the interstitial tissue embedded in collagen I and fibronectin. Additionally, in human muscle, collagen IV was surrounding vessels and myotubes’ sarcomeres. In our system, the lack of deposition of adequate amounts of fibronectin may have hampered the development of adhered ECs to mature networks. Of note, this is not a limitation of the use of HPMECs, because the topographical substrates by themselves warranted spontaneous network formation [
17]. Our data appear to conflict with those of Nagamori et al. who reported that embryonic endothelial cells (HUVEC) readily formed networks on myoblast sheets produced by detachment from thermoresponsive flat substrates [
38]. However, in their system, the use of gelatin to transfer sheets may have facilitated adherence and network formation of the ECs, while in our system the ECs had to rely solely on myotube-deposited ECM. Future studies, besides proving a platform for myotube alignment, also need to provide a matrix to sustain endothelization surrounding the myotubes mimicking the natural muscle.
Our results show that both protein constituents of the basal membrane, i.e., collagen IV and laminin, were deposited by myoblasts more than ECs or even professional connective tissue cell types, i.e., ASCs. This likely explains the efficient adhesion of ECs to pre-differentiated myotubes. Fibronectin, which is a guiding and instructive ECM component for vascularization, was more deposited in myotubes than ECs. However, ASCs deposited even more fibronectin than myotubes, which might show that in our system additional facilitating cells such as stromal or pericytic cells are in demand. We showed before that fibronectin deposited by ASCs augments cell function such as survival and maturation of another myoblast type i.e., cardiomyocytes [
20]. Moreover, we showed that ASCs support formation of vascular endothelial networks in a NOTCH2-dependent fashion [
19]. Both ASCs and myoblasts are mesenchymal stem cells, yet myoblasts and myotubes did not harbor pericytic capacity. We surmise that the low deposition of fibronectin is an underlying cause. In addition, the
VEGFA expression in co-cultures likely is entirely EC-derived while myoblast monocultures did not express
VEGFA. The VEGFA production by ECs might be insufficient to maintain adequate vascularization.
Our findings indicate that there is more cell attachment in the directional topography. Cells detached from the flat PDMS, and, in the directional topography, there was an increase in the deposition of laminin. High expression of laminin is enhancing the proliferation and differentiation properties of the cells [
2]. Laminin gene expression increased in myotubes and co-culture overtime whereas collagen IV gene expression decreased in ECs and the co-culture. Laminin was expressed by myotubes in vitro on the cellular sarcomere. Native muscle remodeling maintains the basal membrane components laminin and collagen IV until the new muscle cells are formed [
39], showing that for regeneration of human skeletal muscle ECM architecture is needed.
Although 3D systems are being investigated as the best option for tissue engineering of skeletal muscle and vascularization, neither the role of the cells’ natural ECM has been addressed in vitro nor the influence of cell alignment on the cell-deposited matrix. Usually, these 3D systems are composed of one main component, e.g., fibrin, but the cellular matrix deposition has been poorly investigated. Most recently, it was found that autologous collagen I deposition in the co-culture of bioartificial muscle could be tuned by decreasing the concentration of fibrin [
40]. However, the network formation behavior decreased once increasing the amount of collagen I in the system. In natural muscle, we found that a large majority of vessels are in the interstitial tissue, which is full of collagen I and fibronectin. Interstitial connective tissue needs to provide a space for regeneration and tissue growth. For that reason, the 3D systems with fibrin/collagen I plus Matrigel have been more successful in maintaining cells in culture than systems with only collagen I [
41,
42,
43], but our system could provide a platform to study the influence of directional topography on the role of the cells’ natural ECM.
Further studies elucidating the ECM properties of different human muscles, aging, and development need to be considered to engineer more personalized skeletal muscle tissue. Additionally, contractile forces are very important for the skeletal muscle functioning and matrix formation. A dynamic in vitro system needs to be implemented to evaluate the ECM architecture and deposition by myotubes to create an interstitial like structure that allows vasculature formation.
Thus far, many studies involved murine-based myoblasts and to a much lesser extent human myoblasts. Although clinical relevance is expected to be higher using human derived cells, it remains difficult to translate findings, as in vivo experiments will be far more difficult to perform. Using murine myoblasts both in vitro and in vivo for extrapolating in vitro data of human myoblasts to in vivo situations are not likely to provide insights due to the intrinsic difference between murine and human myoblasts [
44]. It has been shown that after differentiation of human myoblasts less contractile properties are observed than murine myoblasts and that various surface markers and certain proteins (such as Myostatin) are differently expressed upon differentiation and formation of myofibers [
44,
45,
46]. Even though we see the use of human myoblasts as a strong point for investigating tissue engineering approaches with new biofabrication techniques such as the use of specialized topography substrates, clinical translation with high validity remains a point of concern.