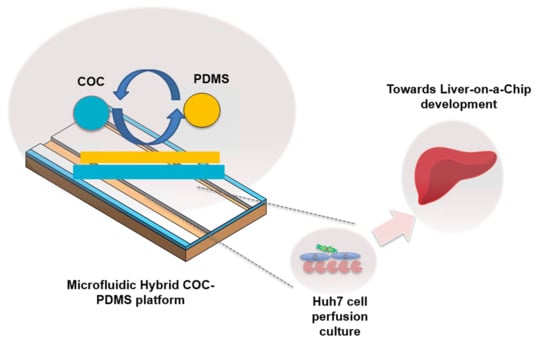
Development of a Hybrid Polymer-Based Microfluidic Platform for Culturing Hepatocytes towards Liver-on-a-Chip Applications
Abstract
:1. Introduction
2. Materials and Methods
2.1. Materials
2.2. Microfluidic Chips Design and Fabrication
2.3. Substrate Biocompatibility Studies
2.4. Microchannel Characterization
2.5. Cell Culture and Material Biocompatibility
2.6. Cell Loading and Flow Experiments
2.7. Cell Functionality Assessment
2.8. Microscopy
3. Results and Discussions
3.1. Evaluation of Microfluidic Device Substrates
3.2. Hybrid COC–PDMS Device Overview
3.3. Computational Fluid Dynamics Simulations
3.3.1. Governing Equations and Physical Models
3.3.2. Computational Domain and Boundary Conditions
3.3.3. Mesh Verification and Boundary Conditions
3.4. Perfusion of Cell Culture in the HCP Platform
4. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Ehrlich, A.; Duche, D.; Ouedraogo, G.; Nahmias, Y. Challenges and opportunities in the design of liver-on-chip microdevices. Annu. Rev. Biomed. Eng. 2019, 21, 219–239. [Google Scholar] [CrossRef]
- Starokozhko, V.; Groothuis, G.M. Judging the value of ‘liver-on-a-chip’devices for prediction of toxicity. Expert Opin. Drug Metab. Toxicol. 2017, 13, 125–128. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ding, C.; Chen, X.; Kang, Q.; Yan, X. Biomedical Application of Functional Materials in Organ-on-a-Chip. Front. Bioeng. Biotechnol. 2020, 8. [Google Scholar] [CrossRef] [PubMed]
- Campbell, S.B.; Wu, Q.; Yazbeck, J.; Liu, C.; Okhovatian, S.; Radisic, M. Beyond polydimethylsiloxane: Alternative materials for fabrication of organ-on-a-chip devices and microphysiological systems. ACS Biomater. Sci. Eng. 2020. [Google Scholar] [CrossRef]
- Low, L.A.; Tagle, D.A. Tissue chips to aid drug development and modeling for rare diseases. Expert Opin. Orphan Drugs 2016, 4, 1113–1121. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Mottet, G.; Perez-Toralla, K.; Tulukcuoglu, E.; Bidard, F.-C.; Pierga, J.-Y.; Draskovic, I.; Londono-Vallejo, A.; Descroix, S.; Malaquin, L.; Louis Viovy, J. A three dimensional thermoplastic microfluidic chip for robust cell capture and high resolution imaging. Biomicrofluidics 2014, 8, 024109. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Van Midwoud, P.M.; Janse, A.; Merema, M.T.; Groothuis, G.M.; Verpoorte, E. Comparison of biocompatibility and adsorption properties of different plastics for advanced microfluidic cell and tissue culture models. Anal. Chem. 2012, 84, 3938–3944. [Google Scholar] [CrossRef] [PubMed]
- Theobald, J.; Ghanem, A.; Wallisch, P.; Banaeiyan, A.A.; Andrade-Navarro, M.A.; Taškova, K.; Haltmeier, M.; Kurtz, A.; Becker, H.; Reuter, S. Liver-kidney-on-chip to study toxicity of drug metabolites. ACS Biomater. Sci. Eng. 2018, 4, 78–89. [Google Scholar] [CrossRef] [PubMed]
- Rennert, K.; Steinborn, S.; Gröger, M.; Ungerböck, B.; Jank, A.-M.; Ehgartner, J.; Nietzsche, S.; Dinger, J.; Kiehntopf, M.; Funke, H. A microfluidically perfused three dimensional human liver model. Biomaterials 2015, 71, 119–131. [Google Scholar] [CrossRef]
- Gröger, M.; Lange, M.; Rennert, K.; Kaschowitz, T.; Plettenberg, H.; Hoffmann, M.; Mosig, A.S. Novel approach for the prediction of cell densities and viability in standardized translucent cell culture biochips with near infrared spectroscopy. Eng. Life Sci. 2017, 17, 585–593. [Google Scholar] [CrossRef]
- Wen, X.; Yamanaka, M.; Terada, S.; Kamei, K.-i. In vitro nonalcoholic fatty liver disease model with cyclo-olefin-polymer-based microphysiological systems. bioRxiv 2020. [Google Scholar] [CrossRef]
- Jellali, R.; Paullier, P.; Fleury, M.-J.; Leclerc, E. Liver and kidney cells cultures in a new perfluoropolyether biochip. Sens. Actuators B Chem. 2016, 229, 396–407. [Google Scholar] [CrossRef]
- Bale, S.S.; Manoppo, A.; Thompson, R.; Markoski, A.; Coppeta, J.; Cain, B.; Haroutunian, N.; Newlin, V.; Spencer, A.; Azizgolshani, H. A thermoplastic microfluidic microphysiological system to recapitulate hepatic function and multicellular interactions. Biotechnol. Bioeng. 2019, 116, 3409–3420. [Google Scholar] [CrossRef] [PubMed]
- Ochs, C.J.; Kasuya, J.; Pavesi, A.; Kamm, R.D. Oxygen levels in thermoplastic microfluidic devices during cell culture. Lab Chip 2014, 14, 459–462. [Google Scholar] [CrossRef] [Green Version]
- Zhou, W.; Dou, M.; Sanjay, S.T.; Xu, F.; Li, X.J. Recent Innovations in Cost-Effective Polymer and Paper Hybrid Microfluidic Devices. Lab Chip 2021. [Google Scholar] [CrossRef] [PubMed]
- Khvostichenko, D.S.; Kondrashkina, E.; Perry, S.L.; Pawate, A.S.; Brister, K.; Kenis, P.J. An X-ray transparent microfluidic platform for screening of the phase behavior of lipidic mesophases. Analyst 2013, 138, 5384–5395. [Google Scholar] [CrossRef] [Green Version]
- Zhang, B.; Xu, H.; Huang, Y.; Shu, W.; Feng, H.; Cai, J.; Zhong, J.F.; Chen, Y. Improving single-cell transcriptome sequencing efficiency with a microfluidic phase-switch device. Analyst 2019, 144, 7185–7191. [Google Scholar] [CrossRef]
- Malic, L.; Zhang, X.; Brassard, D.; Clime, L.; Daoud, J.; Luebbert, C.; Barrere, V.; Boutin, A.; Bidawid, S.; Farber, J. Polymer-based microfluidic chip for rapid and efficient immunomagnetic capture and release of Listeria monocytogenes. Lab Chip 2015, 15, 3994–4007. [Google Scholar] [CrossRef] [PubMed]
- Jang, H.; Pawate, A.S.; Bhargava, R.; Kenis, P.J. Polymeric microfluidic continuous flow mixer combined with hyperspectral FT-IR imaging for studying rapid biomolecular events. Lab Chip 2019, 19, 2598–2609. [Google Scholar] [CrossRef]
- Schieferstein, J.M.; Pawate, A.S.; Varel, M.J.; Guha, S.; Astrauskaite, I.; Gennis, R.B.; Kenis, P.J. X-ray transparent microfluidic platforms for membrane protein crystallization with microseeds. Lab Chip 2018, 18, 944–954. [Google Scholar] [CrossRef] [PubMed]
- Svensson, K. Fabrication and Characterisation of a 3-Layer Aorta-on-a-Chip. Master’s Thesis, Uppsala University, Uppsala, Sweden, 2017. [Google Scholar]
- Tan, K.; Keegan, P.; Rogers, M.; Lu, M.; Gosset, J.R.; Charest, J.; Bale, S.S. A high-throughput microfluidic microphysiological system (PREDICT-96) to recapitulate hepatocyte function in dynamic, re-circulating flow conditions. Lab Chip 2019, 19, 1556–1566. [Google Scholar] [CrossRef] [PubMed]
- Greer, A.I.; Vasiev, I.; Della-Rosa, B.; Gadegaard, N. Fluorinated ethylene–propylene: A complementary alternative to PDMS for nanoimprint stamps. Nanotechnology 2016, 27, 155301. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kulsharova, G.; Kurmangaliyeva, A. Liver microphysiological platforms for drug metabolism applications. Cell Prolif. 2021, e13099. [Google Scholar]
- Sunkara, V.; Park, D.-K.; Hwang, H.; Chantiwas, R.; Soper, S.A.; Cho, Y.-K. Simple room temperature bonding of thermoplastics and poly (dimethylsiloxane). Lab Chip 2011, 11, 962–965. [Google Scholar] [CrossRef] [Green Version]
- Naomi, R.; Ridzuan, P.M.; Bahari, H. Current Insights into Collagen Type I. Polymers 2021, 13, 2642. [Google Scholar] [CrossRef]
- Gerolami, R.; Uch, R.; Jordier, F.; Chapel, S.; Bagnis, C.; Bréchot, C.; Mannoni, P. Gene transfer to hepatocellular carcinoma: Transduction efficacy and transgene expression kinetics by using retroviral and lentiviral vectors. Cancer Gene Ther. 2000, 7, 1286–1292. [Google Scholar] [CrossRef] [Green Version]
- Probst, C.; Schneider, S.; Loskill, P. High-throughput organ-on-a-chip systems: Current status and remaining challenges. Curr. Opin. Biomed. Eng. 2018, 6, 33–41. [Google Scholar] [CrossRef]
- Hassan, S.; Sebastian, S.; Maharjan, S.; Lesha, A.; Carpenter, A.M.; Liu, X.; Xie, X.; Livermore, C.; Zhang, Y.S.; Zarrinpar, A. Liver-on-a-Chip Models of Fatty Liver Disease. Hepatology 2020, 71, 733–740. [Google Scholar] [CrossRef] [PubMed]
- Gehlen, D.B.; De Lencastre Novaes, L.C.; Long, W.; Ruff, A.J.; Jakob, F.; Haraszti, T.; Chandorkar, Y.; Yang, L.; van Rijn, P.; Schwaneberg, U. Rapid and Robust Coating Method to Render Polydimethylsiloxane Surfaces Cell-Adhesive. ACS Appl. Mater. Interfaces 2019, 11, 41091–41099. [Google Scholar] [CrossRef] [PubMed]
- Jeon, J.S.; Chung, S.; Kamm, R.D.; Charest, J.L. Hot embossing for fabrication of a microfluidic 3D cell culture platform. Biomed. Microdevices 2011, 13, 325–333. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Cooper, M.; Charest, J.L.; Coppeta, J. Design principles for dynamic microphysiological systems. In Microfluidic Cell Culture Systems; Elsevier: Amsterdam, The Netherlands, 2019; pp. 1–29. [Google Scholar]
- Bhatia, S.N.; Ingber, D.E. Microfluidic organs-on-chips. Nat. Biotechnol. 2014, 32, 760–772. [Google Scholar] [CrossRef] [PubMed]
- Rojas-Soloŕzano, L.R.; Anna, S.L.; Bradeddine, B.; Amon, C.H. Modeling and simulation of a rollerball microfluidic device. In Proceedings of the International Conference on Nanochannels, Microchannels, and Minichannels, Pohang, Korea, 22–24 June 2009; pp. 705–716. [Google Scholar]
- Islamov, M.; Sypabekova, M.; Kanayeva, D.; Rojas-Solórzano, L. CFD modeling of chamber filling in a micro-biosensor for protein detection. Biosensors 2017, 7, 45. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kang, J.H.; Kim, Y.C.; Park, J.-K. Analysis of pressure-driven air bubble elimination in a microfluidic device. Lab Chip 2008, 8, 176–178. [Google Scholar] [CrossRef] [PubMed]
- Obach, R.S. Predicting drug-drug interactions from in vitro drug metabolism data: Challenges and recent advances. Curr. Opin. Drug Discov. Dev. 2009, 12, 81–89. [Google Scholar]
- Deng, J.; Zhang, X.; Chen, Z.; Luo, Y.; Lu, Y.; Liu, T.; Wu, Z.; Jin, Y.; Zhao, W.; Lin, B. A cell lines derived microfluidic liver model for investigation of hepatotoxicity induced by drug-drug interaction. Biomicrofluidics 2019, 13, 024101. [Google Scholar] [CrossRef]
- Bhise, N.S.; Manoharan, V.; Massa, S.; Tamayol, A.; Ghaderi, M.; Miscuglio, M.; Lang, Q.; Zhang, Y.S.; Shin, S.R.; Calzone, G. A liver-on-a-chip platform with bioprinted hepatic spheroids. Biofabrication 2016, 8, 014101. [Google Scholar] [CrossRef]
- Banaeiyan, A.A.; Theobald, J.; Paukštyte, J.; Wölfl, S.; Adiels, C.B.; Goksör, M. Design and fabrication of a scalable liver-lobule-on-a-chip microphysiological platform. Biofabrication 2017, 9, 015014. [Google Scholar] [CrossRef] [PubMed]
- Fröhlich, E. Comparison of conventional and advanced in vitro models in the toxicity testing of nanoparticles. Artif. Cells Nanomed. Biotechnol. 2018, 46, 1091–1107. [Google Scholar] [CrossRef] [Green Version]
- Moradi, E.; Jalili-Firoozinezhad, S.; Solati-Hashjin, M. Microfluidic organ-on-a-chip models of human liver tissue. Acta Biomater. 2020. [Google Scholar] [CrossRef]
- Ware, B.R.; Khetani, S.R. Engineered liver platforms for different phases of drug development. Trends Biotechnol. 2017, 35, 172–183. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Gough, A.; Soto-Gutierrez, A.; Vernetti, L.; Ebrahimkhani, M.R.; Stern, A.M.; Taylor, D.L. Human biomimetic liver microphysiology systems in drug development and precision medicine. Nat. Rev. Gastroenterol. Hepatol. 2020, 18, 252–268. [Google Scholar]
- Wagner, I.; Materne, E.-M.; Brincker, S.; Süßbier, U.; Frädrich, C.; Busek, M.; Sonntag, F.; Sakharov, D.A.; Trushkin, E.V.; Tonevitsky, A.G. A dynamic multi-organ-chip for long-term cultivation and substance testing proven by 3D human liver and skin tissue co-culture. Lab Chip 2013, 13, 3538–3547. [Google Scholar] [CrossRef] [Green Version]
- Khedr, M.M.; Messaoudi, W.; Jonnalagadda, U.S.; Abdelmotelb, A.M.; Glynne-Jones, P.; Hill, M.; Khakoo, S.I.; Hilal, M.A. Generation of functional hepatocyte 3D discoids in an acoustofluidic bioreactor. Biomicrofluidics 2019, 13, 014112. [Google Scholar] [CrossRef]
- Kim, M.S.; Yeon, J.H.; Park, J.-K. A microfluidic platform for 3-dimensional cell culture and cell-based assays. Biomed. Microdevices 2007, 9, 25–34. [Google Scholar] [CrossRef]
- Torisawa, Y.-s.; Takagi, A.; Nashimoto, Y.; Yasukawa, T.; Shiku, H.; Matsue, T. A multicellular spheroid array to realize spheroid formation, culture, and viability assay on a chip. Biomaterials 2007, 28, 559–566. [Google Scholar] [CrossRef] [PubMed]
- Zawada, R.J.X.; Kwan, P.; Olszewski, K.L.O.L.; Llinas, M.; Huang, S.-G.G. Quantitative determination of urea concentrations in cell culture medium. Biochem. Cell Biol. 2009, 87, 541–544. [Google Scholar] [CrossRef] [PubMed]
- Peters, S.J.; Haagsman, H.P.; van Norren, K. Arginase release by primary hepatocytes and liver slices results in rapid conversion of arginine to urea in cell culture media. Toxicol. Vitr. 2008, 22, 1094–1098. [Google Scholar] [CrossRef] [PubMed]
- Darakhshan, S.; Pour, A.B.; Kowsari-Esfahan, R.; Vosough, M.; Montazeri, L.; Ghanian, M.H.; Baharvand, H.; Piryaei, A. Generation of scalable hepatic micro-tissues as a platform for toxicological studies. Tissue Eng. Regen. Med. 2020, 17, 459–475. [Google Scholar] [CrossRef] [PubMed]





| Mesh-Elements (Feature) | Air Fraction | Deviation, % |
|---|---|---|
| 41,000 (XX-Coarse) | 0.156 | |
| 83,000 (Coarse) | 0.187 | 16.6 |
| 166,367 (Medium) | 0.188 | 0.55 |
| 332,734 (Fine) | 0.188 | 0.16 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kulsharova, G.; Kurmangaliyeva, A.; Darbayeva, E.; Rojas-Solórzano, L.; Toxeitova, G. Development of a Hybrid Polymer-Based Microfluidic Platform for Culturing Hepatocytes towards Liver-on-a-Chip Applications. Polymers 2021, 13, 3215. https://doi.org/10.3390/polym13193215
Kulsharova G, Kurmangaliyeva A, Darbayeva E, Rojas-Solórzano L, Toxeitova G. Development of a Hybrid Polymer-Based Microfluidic Platform for Culturing Hepatocytes towards Liver-on-a-Chip Applications. Polymers. 2021; 13(19):3215. https://doi.org/10.3390/polym13193215
Chicago/Turabian StyleKulsharova, Gulsim, Akbota Kurmangaliyeva, Elvira Darbayeva, Luis Rojas-Solórzano, and Galiya Toxeitova. 2021. "Development of a Hybrid Polymer-Based Microfluidic Platform for Culturing Hepatocytes towards Liver-on-a-Chip Applications" Polymers 13, no. 19: 3215. https://doi.org/10.3390/polym13193215
APA StyleKulsharova, G., Kurmangaliyeva, A., Darbayeva, E., Rojas-Solórzano, L., & Toxeitova, G. (2021). Development of a Hybrid Polymer-Based Microfluidic Platform for Culturing Hepatocytes towards Liver-on-a-Chip Applications. Polymers, 13(19), 3215. https://doi.org/10.3390/polym13193215