Biomimetic Remineralization of an Extracellular Matrix Collagen Membrane for Bone Regeneration
Abstract
:1. Introduction
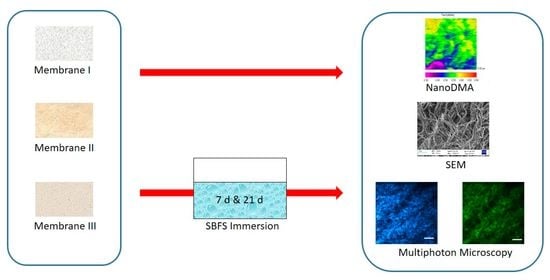
2. Materials and Methods
2.1. Tested GBR Collagen Membranes Description
2.2. Acellular Static In Vitro Bioactivity Test
2.3. Nanomechanical Properties Analysis
2.4. Scanning Electron Microscopy (SEM)
2.5. Multiphoton Microscopy Imaging
2.6. Statistical Analysis
3. Results
3.1. Nanomechanical Properties Analysis
3.2. Scanning Electron Microscopy (SEM)
3.3. Multiphoton Microscopy Imaging
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Sanz, M.; Dahlin, C.; Apatzidou, D.; Artzi, Z.; Bozic, D.; Calciolari, E.; Bruyn, H.D.; Dommisch, H.; Donos, N.; Eickholz, P.; et al. Biomaterials and Regenerative Technologies Used in Bone Regeneration in the Craniomaxillofacial Region: Consensus Report of Group 2 of the 15th European Workshop on Periodontology on Bone Regeneration. J. Clin. Periodontol. 2019, 46, 82–91. [Google Scholar] [CrossRef] [PubMed]
- You, P.; Liu, Y.; Wang, X.; Li, B.; Wu, W.; Tang, L. Acellular Pericardium: A Naturally Hierarchical, Osteoconductive, and Osteoinductive Biomaterial for Guided Bone Regeneration. J. Biomed. Mater. Res. A 2021, 109, 132–145. [Google Scholar] [CrossRef] [PubMed]
- Yu, L.; Wei, M. Biomineralization of Collagen-Based Materials for Hard Tissue Repair. Int. J. Mol. Sci. 2021, 22, 944. [Google Scholar] [CrossRef] [PubMed]
- Parenteau-Bareil, R.; Gauvin, R.; Berthod, F. Collagen-Based Biomaterials for Tissue Engineering Applications. Materials 2010, 3, 1863–1887. [Google Scholar] [CrossRef]
- Caridade, S.G.; Mano, J.F. Engineering Membranes for Bone Regeneration. Tissue Eng. Part A 2017, 23, 1502–1533. [Google Scholar] [CrossRef] [PubMed]
- Rothamel, D.; Benner, M.; Fienitz, T.; Happe, A.; Kreppel, M.; Nickenig, H.-J.; Zöller, J.E. Biodegradation Pattern and Tissue Integration of Native and Cross-Linked Porcine Collagen Soft Tissue Augmentation Matrices—An Experimental Study in the Rat. Head Face Med. 2014, 10, 10. [Google Scholar] [CrossRef] [PubMed]
- Bozkurt, A.; Apel, C.; Sellhaus, B.; van Neerven, S.; Wessing, B.; Hilgers, R.-D.; Pallua, N. Differences in Degradation Behavior of Two Non-Cross-Linked Collagen Barrier Membranes: An in Vitro and in Vivo Study. Clin. Oral Implant. Res. 2014, 25, 1403–1411. [Google Scholar] [CrossRef]
- Li, J.; Yan, J.-F.; Wan, Q.-Q.; Shen, M.-J.; Ma, Y.-X.; Gu, J.-T.; Gao, P.; Tang, X.-Y.; Yu, F.; Chen, J.-H.; et al. Matrix Stiffening by Self-Mineralizable Guided Bone Regeneration. Acta Biomater. 2021, 125, 112–125. [Google Scholar] [CrossRef]
- Song, Q.; Jiao, K.; Tonggu, L.; Wang, L.G.; Zhang, S.L.; Yang, Y.D.; Zhang, L.; Bian, J.H.; Hao, D.X.; Wang, C.Y.; et al. Contribution of Biomimetic Collagen-Ligand Interaction to Intrafibrillar Mineralization. Sci. Adv. 2019, 5, eaav9075. [Google Scholar] [CrossRef]
- ISO 23317:2014. Available online: https://www.iso.org/cms/render/live/en/sites/isoorg/contents/data/standard/06/50/65054.html (accessed on 7 July 2022).
- Ryou, H.; Romberg, E.; Pashley, D.H.; Tay, F.R.; Arola, D. Nanoscopic Dynamic Mechanical Properties of Intertubular and Peritubular Dentin. J. Mech. Behav. Biomed. Mater. 2012, 7, 3–16. [Google Scholar] [CrossRef]
- Pashley, D.H.; Tay, F.R.; Carvalho, R.M.; Rueggeberg, F.A.; Agee, K.A.; Carrilho, M.; Donnelly, A.; García-Godoy, F. From Dry Bonding to Water-Wet Bonding to Ethanol-Wet Bonding. A Review of the Interactions between Dentin Matrix and Solvated Resins Using a Macromodel of the Hybrid Layer. Am. J. Dent. 2007, 20, 7–20. [Google Scholar] [PubMed]
- Han, L.; Grodzinsky, A.J.; Ortiz, C. Nanomechanics of the Cartilage Extracellular Matrix. Annu. Rev. Mater. Res. 2011, 41, 133–168. [Google Scholar] [CrossRef] [PubMed]
- Bueno, J.M.; Gualda, E.J.; Artal, P. Adaptive Optics Multiphoton Microscopy to Study Ex Vivo Ocular Tissues. J. Biomed. Opt. 2010, 15, 066004. [Google Scholar] [CrossRef] [PubMed]
- Skorsetz, M.; Artal, P.; Bueno, J.M. Performance Evaluation of a Sensorless Adaptive Optics Multiphoton Microscope. J. Microsc. 2016, 261, 249–258. [Google Scholar] [CrossRef] [PubMed]
- Lin, S.-J.; Wu, R.-J.; Tan, H.-Y.; Lo, W.; Lin, W.-C.; Young, T.-H.; Hsu, C.-J.; Chen, J.-S.; Jee, S.-H.; Dong, C.-Y. Evaluating Cutaneous Photoaging by Use of Multiphoton Fluorescence and Second-Harmonic Generation Microscopy. Opt. Lett. 2005, 30, 2275–2277. [Google Scholar] [CrossRef] [PubMed]
- Ebisawa, Y.; Kokubo, T.; Ohura, K.; Yamamuro, T. Bioactivity of CaO·SiO2-Based Glasses:In Vitro Evaluation. J. Mater. Sci. Mater. Med. 1990, 1, 239–244. [Google Scholar] [CrossRef]
- Kim, D.; Lee, B.; Thomopoulos, S.; Jun, Y.-S. The Role of Confined Collagen Geometry in Decreasing Nucleation Energy Barriers to Intrafibrillar Mineralization. Nat. Commun. 2018, 9, 962. [Google Scholar] [CrossRef] [PubMed]
- Li, N.; Li, Y.; Gong, D.; Xia, C.; Liu, X.; Xu, Z. Efficient Decellularization for Bovine Pericardium with Extracellular Matrix Preservation and Good Biocompatibility. Interact. Cardiovasc. Thorac. Surg. 2018, 26, 768–776. [Google Scholar] [CrossRef]
- Zouhair, S.; Sasso, E.D.; Tuladhar, S.R.; Fidalgo, C.; Vedovelli, L.; Filippi, A.; Borile, G.; Bagno, A.; Marchesan, M.; Giorgio, D.R.; et al. A Comprehensive Comparison of Bovine and Porcine Decellularized Pericardia: New Insights for Surgical Applications. Biomolecules 2020, 10, 371. [Google Scholar] [CrossRef]
- Ueda, M.; Saito, S.; Murata, T.; Hirano, T.; Bise, R.; Kabashima, K.; Suzuki, S. Combined Multiphoton Imaging and Biaxial Tissue Extension for Quantitative Analysis of Geometric Fiber Organization in Human Reticular Dermis. Sci. Rep. 2019, 9, 10644. [Google Scholar] [CrossRef] [PubMed]
- Toledano, M.; Asady, S.; Toledano-Osorio, M.; García-Godoy, F.; Serrera-Figallo, M.-A.; Benítez-García, J.A.; Osorio, R. Differential Biodegradation Kinetics of Collagen Membranes for Bone Regeneration. Polymers 2020, 12, 1290. [Google Scholar] [CrossRef] [PubMed]
- Maurer, T.; Stoffel, M.H.; Belyaev, Y.; Stiefel, N.G.; Vidondo, B.; Küker, S.; Mogel, H.; Schäfer, B.; Balmer, J. Structural Characterization of Four Different Naturally Occurring Porcine Collagen Membranes Suitable for Medical Applications. PLoS ONE 2018, 13, e0205027. [Google Scholar] [CrossRef] [PubMed]
- An, Y.-Z.; Kim, Y.-K.; Lim, S.-M.; Heo, Y.-K.; Kwon, M.-K.; Cha, J.-K.; Lee, J.-S.; Jung, U.-W.; Choi, S.-H. Physiochemical Properties and Resorption Progress of Porcine Skin-Derived Collagen Membranes: In Vitro and In Vivo Analysis. Dent. Mater. J. 2018, 37, 332–340. [Google Scholar] [CrossRef] [PubMed]
- Hoornaert, A.; d’Arros, C.; Heymann, M.-F.; Layrolle, P. Biocompatibility, Resorption and Biofunctionality of a New Synthetic Biodegradable Membrane for Guided Bone Regeneration. Biomed. Mater. 2016, 11, 045012. [Google Scholar] [CrossRef] [PubMed]
- Vallecillo-Rivas, M.; Toledano-Osorio, M.; Vallecillo, C.; Toledano, M.; Osorio, R. The Collagen Origin Influences the Degradation Kinetics of Guided Bone Regeneration Membranes. Polymers 2021, 13, 3007. [Google Scholar] [CrossRef] [PubMed]
- Vallecillo, C.; Toledano-Osorio, M.; Vallecillo-Rivas, M.; Toledano, M.; Osorio, R. In Vitro Biodegradation Pattern of Collagen Matrices for Soft Tissue Augmentation. Polymers 2021, 13, 2633. [Google Scholar] [CrossRef] [PubMed]
- Trowbridge, E.A.; Roberts, K.M.; Crofts, C.E.; Lawford, P.V. Pericardial Heterografts. Toward Quality Control of the Mechanical Properties of Glutaraldehyde-Fixed Leaflets. J. Thorac. Cardiovasc. Surg. 1986, 92, 21–28. [Google Scholar] [CrossRef]
- Jin, C.; Zhao, L.; Wu, Z.; Li, B.; Liu, R.; He, H.; Wang, L.; Wang, W. Comparison on the Properties of Bovine Pericardium and Porcine Pericardium Used as Leaflet Materials of Transcatheter Heart Valve. Artif. Organs 2022, 46, 427–438. [Google Scholar] [CrossRef] [PubMed]
- Wang, Y.; Hahn, J.; Zhang, Y. Mechanical Properties of Arterial Elastin With Water Loss. J. Biomech. Eng. 2018, 140, 0410121–0410128. [Google Scholar] [CrossRef]
- Doussot, A.; Abo-Alhassan, F.; Derbal, S.; Fournel, I.; Kasereka-Kisenge, F.; Codjia, T.; Khalil, H.; Dubuisson, V.; Najah, H.; Laurent, A.; et al. Indications and Outcomes of a Cross-Linked Porcine Dermal Collagen Mesh (Permacol) for Complex Abdominal Wall Reconstruction: A Multicenter Audit. World J. Surg. 2019, 43, 791–797. [Google Scholar] [CrossRef] [PubMed]
- Tarakanova, A.; Chang, S.-W.; Buehler, M.J. Computational Materials Science of Bionanomaterials: Structure, Mechanical Properties and Applications of Elastin and Collagen Proteins. In Handbook of Nanomaterials Properties; Bhushan, B., Luo, D., Schricker, S.R., Sigmund, W., Zauscher, S., Eds.; Springer: Berlin/Heidelberg, Germany, 2014; pp. 941–962. ISBN 978-3-642-31106-2. [Google Scholar]
- Li, Y.; Rodriguez-Cabello, J.C.; Aparicio, C. Intrafibrillar Mineralization of Self-Assembled Elastin-Like Recombinamer Fibrils. ACS Appl. Mater. Interfaces 2017, 9, 5838–5846. [Google Scholar] [CrossRef] [PubMed]
- Boraldi, F.; Moscarelli, P.; Lofaro, F.D.; Sabia, C.; Quaglino, D. The Mineralization Process of Insoluble Elastin Fibrillar Structures: Ionic Environment vs Degradation. Int. J. Biol. Macromol. 2020, 149, 693–706. [Google Scholar] [CrossRef] [PubMed]
- Fickl, S.; Nannmark, U.; Schlagenhauf, U.; Hürzeler, M.B.; Kebschull, M. Porcine Dermal Matrix in the Treatment of Dehiscence-Type Defects--an Experimental Split-Mouth Animal Trial. Clin. Oral Implant. Res. 2015, 26, 799–805. [Google Scholar] [CrossRef] [PubMed]
- Engler, A.J.; Sen, S.; Sweeney, H.L.; Discher, D.E. Matrix Elasticity Directs Stem Cell Lineage Specification. Cell 2006, 126, 677–689. [Google Scholar] [CrossRef] [PubMed]
- Baker, B.M.; Trappmann, B.; Wang, W.Y.; Sakar, M.S.; Kim, I.L.; Shenoy, V.B.; Burdick, J.A.; Chen, C.S. Cell-Mediated Fibre Recruitment Drives Extracellular Matrix Mechanosensing in Engineered Fibrillar Microenvironments. Nat. Mater. 2015, 14, 1262–1268. [Google Scholar] [CrossRef] [PubMed]
- Osorio, R.; Carrasco-Carmona, Á.; Toledano, M.; Osorio, E.; Medina-Castillo, A.L.; Iskandar, L.; Marques, A.; Deb, S.; Toledano-Osorio, M. Ex Vivo Investigations on Bioinspired Electrospun Membranes as Potential Biomaterials for Bone Regeneration. J. Dent. 2020, 98, 103359. [Google Scholar] [CrossRef] [PubMed]
- Winter, H.H. Can the Gel Point of a Cross-Linking Polymer Be Detected by the G′-G″ Crossover? Polym. Eng. Sci. 1987, 27, 1698–1702. [Google Scholar] [CrossRef]
- Ávila, F.J.; Gambín, A.; Artal, P.; Bueno, J.M. In Vivo Two-Photon Microscopy of the Human Eye. Sci. Rep. 2019, 9, 10121. [Google Scholar] [CrossRef]
- Haluszka, D.; Aminmansour, S.; Tóth, P.; Aminmansour, S.; Kellermayer, M. Nanomechanical and Nonlinear Optical Properties of Glycated Dental Collagen. J. Dent. Res. 2022, 220345221100404. [Google Scholar] [CrossRef]
- Haluszka, D.; Lőrincz, K.; Molnár, G.; Tamás, G.; Kolonics, A.; Szipőcs, R.; Kárpáti, S.; Wikonkál, N.M. In Vivo Second-Harmonic Generation and Ex Vivo Coherent Anti-Stokes Raman Scattering Microscopy to Study the Effect of Obesity to Fibroblast Cell Function Using an Yb-Fiber Laser-Based CARS Extension Unit. Microsc. Res. Tech. 2015, 78, 823–830. [Google Scholar] [CrossRef]
- Jaiswal, A.K.; Kadam, S.S.; Soni, V.P.; Bellare, J.R. Improved Functionalization of Electrospun PLLA/Gelatin Scaffold by Alternate Soaking Method for Bone Tissue Engineering. Appl. Surf. Sci. 2013, 268, 477–488. [Google Scholar] [CrossRef]
- Manakhov, A.; Permyakova, E.S.; Ershov, S.; Sheveyko, A.; Kovalskii, A.; Polčák, J.; Zhitnyak, I.Y.; Gloushankova, N.A.; Zajíčková, L.; Shtansky, D.V. Bioactive TiCaPCON-Coated PCL Nanofibers as a Promising Material for Bone Tissue Engineering. Appl. Surf. Sci. 2019, 479, 796–802. [Google Scholar] [CrossRef]
- Fujihara, K.; Kotaki, M.; Ramakrishna, S. Guided Bone Regeneration Membrane Made of Polycaprolactone/Calcium Carbonate Composite Nano-Fibers. Biomaterials 2005, 26, 4139–4147. [Google Scholar] [CrossRef] [PubMed]






| Commercial Name | Collagen Type | Origin | Cross-Link | Others |
|---|---|---|---|---|
| Derma | Type I and III | Heterologous porcine dermis | No | Elastin fibers |
| Evolution Standard | Collagen fibers | Heterologous porcine pericardium | No | |
| Duo-Teck | Liophilized felt | Equine | No | Bone particles |
| 0 d | 7 d | 21 d | ||||||
|---|---|---|---|---|---|---|---|---|
| Mean | SD | Mean | SD | Mean | SD | Statistics | ||
| Complex modulus | Derma | 14.02 A1 | 3.51 | 40.03 A2 | 18.78 | 71.60 A3 | 37.00 | F = 43.15; p < 0.0001 |
| Evolution | 4.47 B1 | 0.68 | 9.97 B1 | 13.10 | 8.34 B1 | 1.07 | F = 133.73; p < 0.0001 | |
| Duo-Teck | 13.56 A | 3.68 | - | - | - | - | ||
| Statistics | F = 98.99; p < 0.0001 | t = 1.45; p = 0.15 | t = 9.36; p < 0.0001 | |||||
| Loss modulus | Derma | 1.31 A1 | 0.49 | 0.97 A1 | 2.84 | −0.77 A1 | 11.81 | F = 0.75; p = 0.47 |
| Evolution | 2.60 B1 | 0.43 | 0.51 A2 | 1.79 | 2.61 B1 | 0.36 | F = 37.40; p < 0.0001 | |
| Duo-Teck | 1.43 A | 0.58 | - | - | - | - | ||
| Statistics | F = 60.78; p < 0.0001 | t = 0.75; p = 0.46 | t = 1.57; p = 0.12 | |||||
| Storage modulus | Derma | 13.19 A1 | 3.49 | 39.56 A2 | 17.72 | 73.92 A3 | 36.84 | F = 49.58; p < 0.0001 |
| Evolution | 2.82 B1 | 0.92 | 6.77 B1 | 12.88 | 7.02 B1 | 1.06 | F = 171.32; p < 0.0001 | |
| Duo-Teck | 13.43 A | 3.42 | - | - | - | - | ||
| Statistics | F = 134.05; p < 0.0001 | t = 0.97; p = 0.33 | t = 9.94; p < 0.0001 | |||||
| Tan delta | Derma | 0.19 A1 | 0.05 | 0.09 A1 | 0.55 | 0.09 A1 | 0.21 | F= 0.79; p = 0.45 |
| Evolution | 1.02 B1 | 0.35 | 0.13 A2 | 0.40 | 0.52 B3 | 0.10 | F= 60.68; p < 0.0001 | |
| Duo-Teck | 0.24 A | 0.19 | - | - | - | - | ||
| Statistics | F = 120.22; p < 0.0001 | t = 0.35; p = 0.72 | t = 10.04; p < 0.0001 | |||||
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Osorio, R.; Asady, S.; Toledano-Osorio, M.; Toledano, M.; Bueno, J.M.; Martínez-Ojeda, R.M.; Osorio, E. Biomimetic Remineralization of an Extracellular Matrix Collagen Membrane for Bone Regeneration. Polymers 2022, 14, 3274. https://doi.org/10.3390/polym14163274
Osorio R, Asady S, Toledano-Osorio M, Toledano M, Bueno JM, Martínez-Ojeda RM, Osorio E. Biomimetic Remineralization of an Extracellular Matrix Collagen Membrane for Bone Regeneration. Polymers. 2022; 14(16):3274. https://doi.org/10.3390/polym14163274
Chicago/Turabian StyleOsorio, Raquel, Samara Asady, Manuel Toledano-Osorio, Manuel Toledano, Juan M. Bueno, Rosa M. Martínez-Ojeda, and Estrella Osorio. 2022. "Biomimetic Remineralization of an Extracellular Matrix Collagen Membrane for Bone Regeneration" Polymers 14, no. 16: 3274. https://doi.org/10.3390/polym14163274
APA StyleOsorio, R., Asady, S., Toledano-Osorio, M., Toledano, M., Bueno, J. M., Martínez-Ojeda, R. M., & Osorio, E. (2022). Biomimetic Remineralization of an Extracellular Matrix Collagen Membrane for Bone Regeneration. Polymers, 14(16), 3274. https://doi.org/10.3390/polym14163274