Gellan Gum in Wound Dressing Scaffolds
Abstract
:1. Introduction
| Polymers | Advantages | Disadvantages | References |
|---|---|---|---|
| Natural (Alginates, starch, cellulose, pectin, gums, chitin, etc.) | Nontoxic, biodegradable, biocompatible, economical, abundant in nature, and easily metabolized from the body. | Poor mechanical properties, adhesive strength, and extraction process expensive. | [19,20,21,22,23,24] |
| Synthetic (Polyethylene glycol, polyesters, poly lactic acid, polyurethanes, polystyrene, etc.) | Chemical, structural, flexibility mechanical properties are easily improved/controllable, excellent hydrophilic, and | Possibility of toxicity, slow degradation, and poor biocompatibility. | [25,26,27,28,29] |
2. Classification of Wound Dressings
| Classification of Wound Dressings | Commercial Examples: | Advantages | Disadvantages | References |
|---|---|---|---|---|
| Traditional | Bandages, cotton wool, plaster, and gauze | Prevent bacteria contamination and absorb a lot of exudates. | Causes dehydration of the wound and tends to adhere to the wound surface resulting in pains upon removal. | [39,40,41] |
| Biological | Epidermal and dermal skin replacements, skin substitutes, and grafts | Regenerate the lost tissue. | Prone to infection transmission, the possibility of host rejection, and the formation of hypertrophic scars. | [42,43,44] |
| Interactive | None | Provide a moist environment for the wound. | They are semi-occlusive and have poor mechanical stability. | [45,46,47] |
| Bioactive or artificial dressings | Foams, wafers, hydrogels, and transdermal patches | Loaded with antimicrobial agents, biocompatible and biodegradable; They exhibit superior features when compared to other classes of wound dressings. | - | [48,49,50,51] |
3. Properties of Gellan Gum
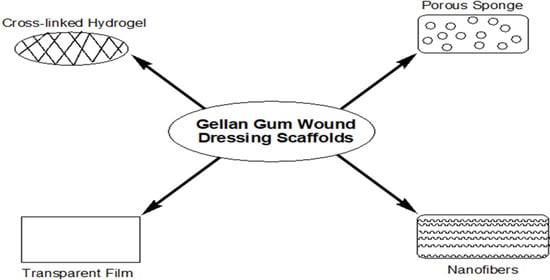
4. Gellan Gum-Based Wound Dressings
4.1. Hydrogels
4.2. Nanofibers
4.3. Films and Membranes
4.4. Other Gellan Wound Dressing Scaffolds
5. Conclusions and Future Perspectives
Author Contributions
Funding
Conflicts of Interest
References
- Mohd, S.S.; Abdullah, M.A.; Mat Amin, K.A. Gellan gum/clay hydrogels for tissue engineering application: Mechanical, thermal behavior, cell viability, and antibacterial properties. J. Bioact. Compact. Polym. 2016, 31, 648–666. [Google Scholar] [CrossRef]
- Mutlu, G.; Calamak, S.; Ulubayram, K.; Guven, E. Curcumin-loaded electrospun PHBV nanofibers as potential wound-dressing material. J. Drug Deliv. Sci. Technol. 2018, 43, 185–193. [Google Scholar] [CrossRef]
- Alven, S.; Nqoro, X.; Aderibigbe, B.A. Polymer-Based Materials Loaded with Curcumin for Wound Healing Application. Polymers 2020, 12, 2286. [Google Scholar] [CrossRef] [PubMed]
- Ndlovu, S.P.; Ngece, K.; Alven, S.; Aderibigbe, B.A. Gelatin-based hybrid scaffolds: Promising wound dressings. Polymers 2021, 13, 2959. [Google Scholar] [CrossRef]
- Rivera, A.E.; Spencer, J.M. Clinical aspects of full-thickness wound healing. Clin. Dermatol. 2007, 25, 39–48. [Google Scholar] [CrossRef] [PubMed]
- Zahedi, P.; Rezaeian, I.; Ranaei-Siadat, S.O.; Jafari, S.H.; Supaphol, P. A review on wound dressings with an emphasis on electrospun nanofibrous polymeric bandages. Polym. Adv. Technol. 2010, 21, 77–95. [Google Scholar] [CrossRef]
- Nosrati, H.; Khodaei, M.; Alizadeh, Z.; Banitalebi-dehkordi, M. Cationic, anionic and neutral polysaccharides for skin tissue engineering and wound healing applications. Int. J. Biol. Macromol. 2021, 192, 298–322. [Google Scholar] [CrossRef]
- Kus, K.J.B.; Ruiz, E.S. Wound Dressings-A Practical Review. Curr. Dermatol. Rep. 2020, 9, 298–308. [Google Scholar] [CrossRef]
- Ahmad, N.; Tayyeb, D.; Ali, I.K.; Alruwaili, N.; Ahmad, W.; ur Rehman, A.; Khan, A.H.; Iqbal, M.S. Development and characterization of hemicellulose-based films for antibacterial wound-dressing application. Polymers 2020, 12, 548. [Google Scholar] [CrossRef]
- Guo, L.A.; DiPietro, S.A. Factors affecting wound healing. J. Dent. Res. 2010, 89, 219–229. [Google Scholar] [CrossRef]
- Alven, S.; Aderibigbe, B.A. Chitosan and Cellulose-Based Hydrogels for Wound Management. Int. J. Mol. Sci. 2020, 21, 9656. [Google Scholar] [CrossRef] [PubMed]
- Dhivya, S.; Padma, V.V.; Santhini, E. Wound dressings-a review. BioMedicine 2015, 5, 24–28. [Google Scholar] [CrossRef] [PubMed]
- Yaşayan, G.; Alarçin, E.; Bal-Öztürk, A.; Avci-Adali, M. Natural polymers for wound dressing applications. In Studies in Natural Products Chemistry; Atta-ur-Rahman, Ed.; Elsevier: Amsterdam, The Netherlands, 2022; Volume 74, pp. 367–441. [Google Scholar]
- Hussain, Z.; Thu, H.E.; Shuid, A.N.; Katas, H.; Hussain, F. Recent Advances in Polymer-based Wound Dressings for the Treatment of Diabetic Foot Ulcer: An Overview of State-of-the-art. Curr. Drug Targets 2017, 18, 527–550. [Google Scholar] [CrossRef] [PubMed]
- Rebelo, R.; Fernandes, M.; Fangueiro, R. Biopolymers in medical implants: A brief review. Procedia Eng. 2017, 200, 236–243. [Google Scholar] [CrossRef]
- Alven, S.; Peter, S.; Mbese, Z.; Aderibigbe, B.A. Polymer-Based Wound Dressing Materials Loaded with Bioactive Agents: Potential Materials for the Treatment of Diabetic Wounds. Polymers 2022, 14, 724. [Google Scholar] [CrossRef] [PubMed]
- Moeini, A.; Pedram, P.; Makvandi, P.; Malinconico, M.; Ayala, G.G. Wound healing and antimicrobial effect of active secondary metabolites in chitosan-based wound dressings: A review. Carbohydr. Polym. 2020, 233, 115839. [Google Scholar] [CrossRef] [PubMed]
- Okur, N.Ü.; Hökenek, N.; Okur, M.E.; Ayla, Ş.; Yoltaş, A.; Siafaka, P.I.; Cevher, E. An alternative approach to wound healing field; new composite films from natural polymers for mupirocin dermal delivery. Saudi Pharm. J. 2019, 27, 738–752. [Google Scholar] [CrossRef] [PubMed]
- Bacakova, L.; Zikmundova, M.; Pajorova, J.; Broz, A.; Filova, E.; Blanquer, A.; Matejka, R.; Stepanovska, J.; Mikes, P.; Jencova, V.; et al. Nanofibrous scaffolds for skin tissue engineering and wound healing based on synthetic polymers. Appl. Nanobiotechnol. 2019, 1, 2019. [Google Scholar]
- Biswas, M.C.; Jony, B.; Nandy, P.K.; Chowdhury, R.A.; Halder, S.; Kumar, D.; Ramakrishna, S.; Hassan, M.; Ahsan, M.A.; Hoque, M.E.; et al. Recent advancement of biopolymers and their potential biomedical applications. J. Polym. Environ. 2021, 1–24. [Google Scholar] [CrossRef]
- Memic, A.; Abdullah, T.; Mohammed, H.S.; Joshi Navare, K.; Colombani, T.; Bencherif, S.A. Latest progress in electrospun nanofibers for wound healing applications. ACS Appl. Bio Mater. 2019, 2, 952–969. [Google Scholar] [CrossRef]
- Alves, T.F.; Morsink, M.; Batain, F.; Chaud, M.V.; Almeida, T.; Fernandes, D.A.; da Silva, C.F.; Souto, E.B.; Severino, P. Applications of natural, semi-synthetic, and synthetic polymers in cosmetic formulations. Cosmetics 2020, 7, 75. [Google Scholar] [CrossRef]
- Ilyas, R.A.; Sapuan, S.M. The preparation methods and processing of natural fibre bio-polymer composites. Curr. Org. Synth. 2019, 16, 1068–1070. [Google Scholar] [CrossRef] [PubMed]
- Biswal, T. Biopolymers for tissue engineering applications: A review. Mater. Today Proc. 2021, 41, 397–402. [Google Scholar] [CrossRef]
- Negut, I.; Dorcioman, G.; Grumezescu, V. Scaffolds for wound healing applications. Polymers 2020, 12, 2010. [Google Scholar] [CrossRef]
- Keshvardoostchokami, M.; Majidi, S.S.; Huo, P.; Ramachandran, R.; Chen, M.; Liu, B. Electrospun nanofibers of natural and synthetic polymers as artificial extracellular matrix for tissue engineering. Nanomaterials 2020, 11, 21. [Google Scholar] [CrossRef]
- Liu, X.; Xu, H.; Zhang, M.; Yu, D.G. Electrospun medicated nanofibers for wound healing. Membranes 2021, 11, 770. [Google Scholar] [CrossRef]
- Zhong, Y.; Xiao, H.; Seidi, F.; Jin, Y. Natural polymer-based antimicrobial hydrogels without synthetic antibiotics as wound dressings. Biomacromolecules 2020, 21, 2983–3006. [Google Scholar] [CrossRef]
- Liu, W.; Ou-Yang, W.; Zhang, C.; Wang, Q.; Pan, X.; Huang, P.; Zhang, C.; Li, Y.; Kong, D.; Wang, W. Synthetic polymeric antibacterial hydrogel for methicillin-resistant staphylococcus aureus-infected wound healing: Nanoantimicrobial self-assembly, drug-and cytokine-free strategy. ACS Nano 2020, 14, 12905–12917. [Google Scholar] [CrossRef]
- Vivcharenko, V.; Przekora, A. Modifications of wound dressings with bioactive agents to achieve improved pro-healing properties. Appl. Sci. 2021, 11, 4114. [Google Scholar] [CrossRef]
- Aycan, D.; Selmi, B.; Kelel, E.; Yildirim, T.; Alemdar, N. Conductive polymeric film loaded with ibuprofen as a wound dressing material. Eur. Polym. J. 2019, 121, 109308. [Google Scholar] [CrossRef]
- Mir, M.; Murtaza, N.A.; Barakullah, A.; Gulzar, A.; Arshad, M.; Fatima, S.; Asad, M. Synthetic polymeric biomaterials for wound healing: A review. Prog. Biomater. 2018, 1, 1–21. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Aljghami, M.E.; Saboor, S.; Amini-Nik, S. Emerging innovative wound dressings. Ann. Biomed. Eng. 2019, 47, 659–675. [Google Scholar] [CrossRef] [PubMed]
- Shimizu, R.; Kishi, K. Skin Graft. Plast. Surg. Int. 2012, 5, 160–8582. [Google Scholar] [CrossRef] [PubMed]
- Ng, S.F.; Jumaat, N. Carboxymethyl cellulose wafers containing antimicrobials: A modern drug delivery system for wound infections. Eur. J. Pharm. Sci. 2014, 51, 173–179. [Google Scholar] [CrossRef]
- Ambekar, R.S.; Kandasubramanian, B. Advancements in nanofibers for wound dressing: A review. Eur. Polym. J. 2019, 117, 304–336. [Google Scholar] [CrossRef]
- Saghazadeh, S.; Rinoldi, C.; Schot, M.; Kashaf, S.S.; Sharifi, F.; Jalilian, E.; Nuutila, K.; Giatsidis, G.; Mostafalu, P.; Derakhshandeh, H.; et al. Drug delivery systems and materials for wound healing applications. Adv. Drug Deliv. Rev. 2018, 127, 138–166. [Google Scholar] [CrossRef]
- Du, H.; Liu, W.; Zhang, M.; Si, C.; Zhang, X.; Li, B. Cellulose nanocrystals and cellulose nanofibrils based hydrogels for biomedical applications. Carbohydr. Polym. 2019, 209, 130–144. [Google Scholar] [CrossRef]
- Nuutila, K.; Samandari, M.; Endo, Y.; Zhang, Y.; Quint, J.; Schmidt, T.A.; Tamayol, A.; Sinha, I. In vivo printing of growth factor-eluting adhesive scaffolds improves wound healing. Bioact. Mater. 2022, 8, 296–308. [Google Scholar] [CrossRef]
- Pan, Z.; Ye, H.; Wu, D. Recent advances on polymeric hydrogels as wound dressings. APL Bioeng. 2021, 5, 011504. [Google Scholar] [CrossRef]
- Koehler, J.; Brandl, F.P.; Goepferich, A.M. Hydrogel wound dressings for bioactive treatment of acute and chronic wounds. Eur. Polym. J. 2018, 100, 1–11. [Google Scholar] [CrossRef]
- Karahaliloğlu, Z.; Ercan, B.; Denkbaş, E.B.; Webster, T.J. Nanofeatured silk fibroin membranes for dermal wound healing applications. J. Biomed. Mater. Res. Part A 2015, 103, 135–144. [Google Scholar] [CrossRef] [PubMed]
- Khorasani, M.T.; Joorabloo, A.; Moghaddam, A.; Shamsi, H.; MansooriMoghadam, Z. Incorporation of ZnO nanoparticles into heparinised polyvinyl alcohol/chitosan hydrogels for wound dressing application. Int. J. Biol. Macromol. 2018, 114, 1203–1215. [Google Scholar] [CrossRef] [PubMed]
- Halim, A.S.; Khoo, T.L.; Yussof, S.J. Biologic and synthetic skin substitutes: An overview. Indian J. Plast. Surg. 2010, 43, S23–S28. [Google Scholar] [CrossRef] [PubMed]
- Liu, M.; Zhang, H.; Min, D.; Miao, X.; Li, F.; Dong, L.; Xing, J.; Guo, G.; Wang, X. Dual layered wound dressing with simultaneous temperature & antibacterial regulation properties. Mater. Sci. Eng. C 2019, 94, 1077–1082. [Google Scholar]
- Eskandarinia, A.; Kefayat, A.; Gharakhloo, M.; Agheb, M.; Khodabakhshi, D.; Khorshidi, M.; Sheikhmoradi, V.; Rafienia, M.; Salehi, H. A propolis enriched polyurethane-hyaluronic acid nanofibrous wound dressing with remarkable antibacterial and wound healing activities. Int. J. Biol. Macromol. 2020, 149, 467–476. [Google Scholar] [CrossRef]
- Negut, I.; Grumezescu, V.; Grumezescu, A.M. Treatment strategies for infected wounds. Molecules 2018, 23, 2392. [Google Scholar] [CrossRef]
- Gupta, A.; Briffa, S.M.; Swingler, S.; Gibson, H.; Kannappan, V.; Adamus, G.; Kowalczuk, M.; Martin, C.; Radecka, I. Synthesis of silver nanoparticles using curcumin-cyclodextrins loaded into bacterial cellulose-based hydrogels for wound dressing applications. Biomacromolecules 2020, 21, 1802–1811. [Google Scholar] [CrossRef]
- Fahimirad, S.; Ajalloueian, F. Naturally-derived electrospun wound dressings for target delivery of bio-active agents. Int. J. Pharm. 2019, 566, 307–328. [Google Scholar] [CrossRef]
- Naseri-Nosar, M.; Ziora, Z.M. Wound dressings from naturally-occurring polymers: A review on homopolysaccharide-based composites. Carbohydr. Polym. 2018, 189, 379–398. [Google Scholar] [CrossRef]
- Kiti, K.; Suwantong, O. Bilayer wound dressing based on sodium alginate incorporated with curcumin-β-cyclodextrin inclusion complex/chitosan hydrogel. Int. J. Biol. Macromol. 2020, 164, 4113–4124. [Google Scholar] [CrossRef]
- Ahmad, S.; Ahmad, M.; Manzoor, K.; Purwar, R.; Ikram, S. A review on latest innovations in natural gums based hydrogels: Preparations & applications. Int. J. Biol. Macromol. 2019, 136, 870–890. [Google Scholar] [PubMed]
- Mahmood, H.; Khan, I.U.; Asif, M.; Khan, R.U.; Asghar, S.; Khalid, I.; Khalid, S.H.; Irfan, M.; Rehman, F.; Shahzad, Y.; et al. In vitro and in vivo evaluation of gellan gum hydrogel films: Assessing the co impact of therapeutic oils and ofloxacin on wound healing. Int. J. Biol. Macromol. 2021, 166, 483–495. [Google Scholar] [CrossRef] [PubMed]
- Palumbo, F.S.; Federico, S.; Pitarresi, G.; Fiorica, C.; Giammona, G. Gellan gum-based delivery systems of therapeutic agents and cells. Carbohydr. Polym. 2019, 229, 115430. [Google Scholar] [CrossRef] [PubMed]
- Padil, V.V.; Cheong, J.Y.; AkshayKumar, K.P.; Makvandi, P.; Zare, E.N.; Torres-Mendieta, R.; Varma, R.S. Electrospun fibers based on carbohydrate gum polymers and their multifaceted applications. Carbohydr. Polym. 2020, 247, 116705. [Google Scholar] [CrossRef]
- Das, M.; Giri, T.K. Hydrogels based on gellan gum in cell delivery and drug delivery. J. Drug Deliv. Sci. Technol. 2020, 56, 101586. [Google Scholar] [CrossRef]
- Oliveira, J.T.; Santos, T.C.; Martins, L.; Picciochi, R.; Marques, A.P.; Castro, A.G.; Reis, R.L. Gellan gum injectable hydrogels for cartilage tissue engineering applications: In vitro studies and preliminary in vivo evaluation. Tissue Eng. Part A 2010, 16, 343–353. [Google Scholar] [CrossRef]
- Muthukumar, T.; Song, J.E.; Khang, G. Biological role of gellan gum in improving scaffold drug delivery, cell adhesion properties for tissue engineering applications. Molecules 2019, 24, 4514. [Google Scholar] [CrossRef]
- Zia, K.M.; Tabasum, S.; Khan, M.F.; Akram, N.; Akhter, N.; Noreen, A.; Zuber, M. Recent trends on gellan gum blends with natural and synthetic polymers: A review. Int. J. Biol. Macromol. 2019, 109, 1068–1087. [Google Scholar] [CrossRef]
- Mat-Amin, K.A.; Gilmore, K.J.; Matic, J.; Poon, S.; Walker, M.J.; Wilson, M.R.; in het Panhuis, M. Polyelectrolyte complex materials consisting of antibacterial and cell-supporting layers. Macromol. Biosci. 2012, 3, 374–382. [Google Scholar] [CrossRef]
- Francesko, A.; Petkova, P.; Tzanov, T. Hydrogel dressings for advanced wound management. Curr. Med. Chem. 2018, 25, 5782–5797. [Google Scholar] [CrossRef]
- Rezvani, G.E.; Khalili, S.; Nouri, K.S.; Esmaeely, N.R.; Ramakrishna, S. Wound dressings: Current advances and future directions. J. Appl. Polym. Sci. 2019, 136, 47738. [Google Scholar] [CrossRef]
- Sun, G.; Shen, Y.I.; Harmon, J.W. Engineering Pro-Regenerative Hydrogels for Scarless Wound Healing. Adv. Healthc. Mater. 2018, 7, 1800016. [Google Scholar] [CrossRef] [PubMed]
- Weller, C.; Team, V. Interactive dressings and their role in moist wound management. Adv. Text. Wound Care 2019, 7, 105–134. [Google Scholar]
- Kamoun, E.A.; Kenawy, E.R.S.; Chen, X. A review on polymeric hydrogel membranes for wound dressing applications: PVA-based hydrogel dressings. J. Adv. Res. 2017, 8, 217–233. [Google Scholar] [CrossRef]
- Shukla, R.; Kashaw, S.K.; Jain, A.P.; Lodhi, S. Fabrication of Apigenin loaded gellan gum–chitosan hydrogels (GGCH-HGs) for effective diabetic wound healing. Int. J. Biol. Macromol. 2016, 91, 1110–1119. [Google Scholar] [CrossRef] [PubMed]
- Shanmugapriya, K.; Kim, H.; Kang, H.W. Fucoidan-loaded hydrogels facilitates wound healing using photodynamic therapy by in vitro and in vivo evaluation. Carbohydr. Polym. 2020, 247, 116624. [Google Scholar] [CrossRef] [PubMed]
- Pacelli, S.; Paolicelli, P.; Moretti, G.; Petralito, S.; Di Giacomo, S.; Vitalone, A.; Casadei, M.A. Gellan gum methacrylate and laponite as an innovative nanocomposite hydrogel for biomedical applications. Eur. Polym. J. 2016, 77, 114–123. [Google Scholar] [CrossRef]
- Muktar, M.Z.; Ismail, W.I.W.; Razak, S.I.A.; Razali, M.H.; Amin, K.A.M. Accelerated wound healing of physically cross linked gellan gum-virgin coconut oil hydrogel containing manuka honey. ASM Sci J. 2018, 11, 166–182. [Google Scholar]
- Ng, J.Y.; Zhu, X.; Mukherjee, D.; Zhang, C.; Hong, S.; Kumar, Y.; Ee, P.L.R. Pristine gellan gum–collagen interpenetrating network hydrogels as mechanically enhanced anti-inflammatory biologic wound dressings for burn wound therapy. ACS Appl. Bio Mater. 2021, 4, 1470–1482. [Google Scholar] [CrossRef]
- Xu, Z.; Li, Z.; Jiang, S.; Bratlie, K.M. Chemically modified gellan gum hydrogels with tunable properties for use as tissue engineering scaffolds. ACS Omega 2018, 3, 6998–7007. [Google Scholar] [CrossRef]
- Li, W.; Jian, X.; Zou, Y.; Wu, L.; Huang, H.; Li, H.; Yu, B. The fabrication of a gellan gum-based hydrogel loaded with magnesium ions for the synergistic promotion of skin wound healing. Front. Bioeng. Biotechnol. 2021, 9, 709679. [Google Scholar] [CrossRef] [PubMed]
- Özkahraman, B.; Özbaş, Z.; Bayrak, G.; Tamahkar, E.; Perçin, I.; Kılıç Süloğlu, A.; Boran, F. Characterization and antibacterial activity of gelatin–gellan gum bilayer wound dressing. Int. J. Polym. Mater. Polym. Biomater. 2021, 10, 1–12. [Google Scholar] [CrossRef]
- Sebria, N.J.M.; Amin, K.A.M. Gellan gum/ibuprofen hydrogel for dressing application: Mechanical properties, release activity and biocompatibility studies. Int. J. Appl. Chem. 2016, 12, 483–498. [Google Scholar]
- Muktar, M.Z.; Bakar, M.A.A.; Amin, K.A.M.; Che Rose, L.; Wan Ismail, W.I.; Razali, M.H.; Panhuis, M. Gellan Gum Hydrogels Filled Edible Oil Microemulsion for Biomedical Materials: Phase Diagram, Mechanical Behavior, and In Vivo Studies. Polymers 2021, 13, 3281. [Google Scholar] [CrossRef] [PubMed]
- Tort, S.; Acartürk, F.; Beşikci, A. Evaluation of three-layered doxycycline-collagen loaded nanofiber wound dressing. Int. J. Pharm. 2017, 529, 642–653. [Google Scholar] [CrossRef]
- Jafari, A.; Amirsadeghi, A.; Hassanajili, S.; Azarpira, N. Bioactive antibacterial bilayer PCL/gelatin nanofibrous scaffold promotes full-thickness wound healing. Int. J. Pharm. 2020, 583, 119413. [Google Scholar] [CrossRef]
- Aduba Jr, D.C.; Yang, H. Polysaccharide fabrication platforms and biocompatibility assessment as candidate wound dressing materials. Bioengineering 2017, 4, 1. [Google Scholar] [CrossRef]
- Thorvaldsson, A.; Silva-Correia, J.; Oliveira, J.M.; Reis, R.L.; Gatenholm, P.; Walkenström, P. Development of nanofiber-reinforced hydrogel scaffolds for nucleus pulposus regeneration by a combination of electrospinning and spraying technique. J. Appl. Polym. Sci. 2013, 128, 1158–1163. [Google Scholar] [CrossRef]
- Lin, W.; Chen, M.; Qu, T.; Li, J.; Man, Y. Three-dimensional electrospun nanofibrous scaffolds for bone tissue engineering. J. Biomed. Mater. Res. Part B Appl. Biomater. 2020, 108, 1311–1321. [Google Scholar] [CrossRef]
- Mbese, Z.; Alven, S.; Aderibigbe, B.A. Collagen-based nanofibers for skin regeneration and wound dressing applications. Polymers 2021, 13, 4368. [Google Scholar] [CrossRef]
- Alven, S.; Buyana, B.; Feketshane, Z.; Aderibigbe, B.A. Electrospun nanofibers/nanofibrous scaffolds loaded with silver nanoparticles as effective antibacterial wound dressing materials. Pharmaceutics 2021, 13, 964. [Google Scholar] [CrossRef] [PubMed]
- Mishra, P.; Gupta, P.; Pruthi, V. Cinnamaldehyde incorporated gellan/PVA electrospun nanofibers for eradicating Candida biofilm. Mater. Sci. Eng. C 2021, 119, 111450. [Google Scholar] [CrossRef] [PubMed]
- Vashisth, P.; Pruthi, V. Synthesis and characterization of crosslinked gellan/PVA nanofibers for tissue engineering application. Mater. Sci. Eng. C 2016, 67, 304–312. [Google Scholar] [CrossRef] [PubMed]
- Vashisth, P.; Srivastava, A.K.; Nagar, H.; Raghuwanshi, N.; Sharan, S.; Nikhil, K.; Pruthi, V. Drug functionalized microbial polysaccharide based nanofibers as transdermal substitute. Nanomed. Nanotechnol. Biol. Med. 2016, 12, 1375–1385. [Google Scholar] [CrossRef]
- Vashisth, P.; Pruthi, P.A.; Singh, R.P.; Pruthi, V. Process optimization for fabrication of gellan based electrospun nanofibers. Carbohydr. Polym. 2014, 109, 16–21. [Google Scholar] [CrossRef]
- Vashisth, P.; Pruthi, P.A.; Singh, R.P.; Pruthi, V. Evaluation Of Gellan Based Electrospun Nanofibers For Wound Healing. Proc. Nanoconference 2014, 4, 514–517. [Google Scholar]
- Palumbo, F.S.; Federico, S.; Pitarresi, G.; Fiorica, C.; Scaffaro, R.; Maio, A.; Giammona, G. Effect of alkyl derivatization of gellan gum during the fabrication of electrospun membranes. J. Ind. Text. 2021, 51, 2467S–2482S. [Google Scholar] [CrossRef]
- Graça, M.F.; Miguel, S.P.; Cabral, C.S.; Correia, I.J. Hyaluronic acid—Based wound dressings: A review. Carbohydr. Polym. 2020, 241, 116364. [Google Scholar] [CrossRef]
- Boateng, J.S.; Matthews, K.H.; Stevens, H.N.; Eccleston, G.M. Wound healing dressings and drug delivery systems: A review. J. Pharm. Sci. 2008, 97, 2892–2923. [Google Scholar] [CrossRef]
- Contardi, M.; Heredia-Guerrero, J.A.; Perotto, G.; Valentini, P.; Pompa, P.P.; Spanò, R.; Bayer, I.S. Transparent ciprofloxacin-povidone antibiotic films and nanofiber mats as potential skin and wound care dressings. Eur. J. Pharm. Sci. 2017, 104, 133–144. [Google Scholar] [CrossRef]
- Ismail, N.A.; Amin, K.A.M.; Majid, F.A.A.; Razali, M.H. Gellan gum incorporating titanium dioxide nanoparticles biofilm as wound dressing: Physicochemical, mechanical, antibacterial properties and wound healing studies. Mater. Sci. Eng. C 2019, 103, 109770. [Google Scholar] [CrossRef] [PubMed]
- Razali, M.H.; Ismail, N.A.; Amin, K.A.M. Titanium dioxide nanotubes incorporated gellan gum bio-nanocomposite film for wound healing: Effect of TiO2 nanotubes concentration. Int. J. Biol. Macromol. 2020, 153, 1117–1135. [Google Scholar] [CrossRef] [PubMed]
- Ismail, N.A.; Amin, K.A.M.; Razali, M.H. Novel gellan gum incorporated TiO2 nanotubes film for skin tissue engineering. Mater. Lett. 2018, 228, 116–120. [Google Scholar] [CrossRef]
- Ismail, N.A.; Amin, K.A.M. Mohd. Hasmizam Razali, Antibacterial Study of Gellan Gum (GG) Film Incorporated Norfloxacin. J. Pure Appl. Microbiol. 2019, 13, 1095–1102. [Google Scholar] [CrossRef]
- Azam, N.M.; Amin, K.A.M. The physical and mechanical properties of gellan gum films incorporated manuka honey as wound dressing materials. IOP Conf. Ser. Mater. Sci. Eng. 2017, 209, 012027. [Google Scholar] [CrossRef]
- Ismail, N.A.; Razali, M.H.; Amin, K.A.M. Mechanical and physicochemical properties study on gellan gum thin film prepared using film casting method. AIP Conf. Proc. 2017, 1885, 020045. [Google Scholar]
- Ismail, N.A.; Mohamad, S.F.; Ibrahim, M.A.; Mat Amin, K.A. Evaluation of gellan gum film containing virgin coconut oil for transparent dressing materials. Adv. Biomater. 2014, 2014, 351248. [Google Scholar] [CrossRef] [Green Version]
- Lee, M.W.; Chen, H.J.; Tsao, S.W. Preparation, characterization and biological properties of Gellan gum films with 1-ethyl-3-(3-dimethylaminopropyl) carbodiimide cross-linker. Carbohydr. Polym. 2010, 82, 920–926. [Google Scholar] [CrossRef]
- Lu, Y.; Zhao, X.; Fang, S. Characterization, antimicrobial properties and coatings application of gellan gum oxidized with hydrogen peroxide. Foods 2019, 8, 31. [Google Scholar] [CrossRef]
- Chinnaiyan, S.K.; Pandiyan, R.; Natesan, S.; Chindam, S.; Gouti, A.K.; Sugumaran, A. Fabrication of basil oil Nanoemulsion loaded gellan gum hydrogel—Evaluation of its antibacterial and anti-biofilm potential. J. Drug Deliv. Sci. Technol. 2022, 68, 103129. [Google Scholar] [CrossRef]
- Reczyńska-Kolman, K.; Hartman, K.; Kwiecień, K.; Brzychczy-Włoch, M.; Pamuła, E. Composites Based on Gellan Gum, Alginate and Nisin-Enriched Lipid Nanoparticles for the Treatment of Infected Wounds. Int. J. Mol. Sci. 2021, 23, 321. [Google Scholar] [CrossRef] [PubMed]
- Song, J.E.; Lee, S.E.; Cha, S.R.; Jang, N.K.; Tripathy, N.; Reis, R.L.; Khang, G. Inflammatory response study of gellan gum impregnated duck’s feet derived collagen sponges. J. Biomater. Sci. Polym. Ed. 2016, 27, 1495–1506. [Google Scholar] [CrossRef] [PubMed]
- Yu, I.; Kaonis, S.; Chen, R. A study on degradation behavior of 3D printed gellan gum scaffolds. Procedia CIRP 2017, 65, 78–83. [Google Scholar] [CrossRef]




Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Feketshane, Z.; Alven, S.; Aderibigbe, B.A. Gellan Gum in Wound Dressing Scaffolds. Polymers 2022, 14, 4098. https://doi.org/10.3390/polym14194098
Feketshane Z, Alven S, Aderibigbe BA. Gellan Gum in Wound Dressing Scaffolds. Polymers. 2022; 14(19):4098. https://doi.org/10.3390/polym14194098
Chicago/Turabian StyleFeketshane, Zizo, Sibusiso Alven, and Blessing Atim Aderibigbe. 2022. "Gellan Gum in Wound Dressing Scaffolds" Polymers 14, no. 19: 4098. https://doi.org/10.3390/polym14194098
APA StyleFeketshane, Z., Alven, S., & Aderibigbe, B. A. (2022). Gellan Gum in Wound Dressing Scaffolds. Polymers, 14(19), 4098. https://doi.org/10.3390/polym14194098