Poly (Ether-Ether-Ketone) for Biomedical Applications: From Enhancing Bioactivity to Reinforced-Bioactive Composites—An Overview
Abstract
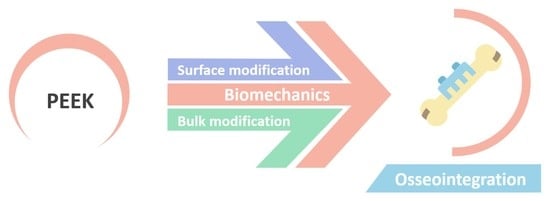
:1. Introduction
2. Drawbacks in Metallic Implant Devices
3. Peek Synthesis
4. Peek Bioactivity
4.1. Surface Modification
4.1.1. Chemical Modification
4.1.2. Physical Modification
4.1.3. Limitations of Chemical and Physical Treatments
4.1.4. Surface Coating
4.2. Bulk Modification
4.2.1. Bioactive Composites of PEEK
4.2.2. Reinforced PEEK Composites
4.3. PEEK on Biomedical Field: Applications and Future Prospectives
5. Final Considerations
Author Contributions
Funding
Institutional Review Board Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Abbreviations
| Description | Abbreviation |
| 316L SS | 316L stainless steel |
| accelerated neutral atom beam | ANAB |
| additive manufacturing | AM |
| calcium | Ca |
| calcium metasilicate | CaSiO3 |
| carbon fiber reinforced | CFR |
| computed tomography | CT |
| fused deposition modeling | FDM |
| hydroxyapatite | HA |
| metal-on-metal | MoM |
| metal-on-polymer | MoP |
| modified HA | mHA |
| nanorod HA | nHA |
| poly(ether-ether-ketone) | PEEK |
| silanized zinc oxide | s-ZnO |
| simulated body fluid | SBF |
| strain energy density | SED |
| strontium | Sr |
| tantalum | Ta |
| titanium | Ti |
| titanium dioxide | TiO2 |
| ultra-high molecular weight polyethylene | UHMWPE |
| ultraviolet | UV |
| zinc oxide | ZnO |
References
- Li, Y.; Liao, C.; Tjong, S.C. Synthetic Biodegradable Aliphatic Polyester Nanocomposites Reinforced with Nanohydroxyapatite and/or Graphene Oxide for Bone Tissue Engineering Applications. Nanomaterials 2019, 9, 590. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Huzum, B.; Curpan, A.S.; Puha, B.; Serban, D.N.; Veliceasa, B.; Necoara, R.M.; Alexa, O.; Serban, I.L. Connections between Orthopedic Conditions and Oxidative Stress: Current Perspective and the Possible Relevance of Other Factors, Such as Metabolic Implications, Antibiotic Resistance, and COVID-19. Medicina 2022, 58, 439. [Google Scholar] [CrossRef] [PubMed]
- Chen, Y.; Lin, K.; Yeh, S.-H.; Wang, C.-H.; Pan, A.-W.; Chen, H.-L.; Chen, C.-J. Associations among quality of life, activities, and participation in elderly residents with joint contractures in long-term care facilities: A cross-sectional study. BMC Geriatr. 2022, 22, 197. [Google Scholar] [CrossRef] [PubMed]
- Martel-Pelletier, J.; Barr, A.J.; Cicuttini, F.M.; Conaghan, P.G.; Cooper, C.; Goldring, M.B.; Goldring, S.R.; Jones, G.; Teichtahl, A.J.; Pelletier, J.-P. Osteoarthritis. Nat. Rev. Dis. Prim. 2016, 2, 16072. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Algahtany, M.A. Association between orthopedic fractures and traumatic spinal injury due to road traffic accidents. Appl. Bionics Biomech. 2021, 2021, 1–10. [Google Scholar] [CrossRef]
- Wu, Z.; Chan, B.; Low, J.; Chu, J.J.H.; Hey, H.W.D.; Tay, A. Microbial resistance to nanotechnologies: An important but understudied consideration using antimicrobial nanotechnologies in orthopaedic implants. Bioact. Mater. 2022, 16, 249–270. [Google Scholar] [CrossRef]
- Fragogeorgi, E.A.; Rouchota, M.; Georgiou, M.; Velez, M.; Bouziotis, P.; Loudos, G. In vivo imaging techniques for bone tissue engineering. J. Tissue Eng. 2019, 10, 204173141985458. [Google Scholar] [CrossRef] [Green Version]
- Borciani, G.; Montalbano, G.; Baldini, N.; Cerqueni, G.; Vitale-Brovarone, C.; Ciapetti, G. Co–culture systems of osteoblasts and osteoclasts: Simulating in vitro bone remodeling in regenerative approaches. Acta Biomater. 2020, 108, 22–45. [Google Scholar] [CrossRef]
- Senra, M.R.; Marques, M.d.F.V. Synthetic Polymeric Materials for Bone Replacement. J. Compos. Sci. 2020, 4, 191. [Google Scholar] [CrossRef]
- Bai, L.; Gong, C.; Chen, X.; Sun, Y.; Zhang, J.; Cai, L.; Zhu, S.; Xie, S.Q. Additive Manufacturing of Customized Metallic. Metals 2019, 9, 1004. [Google Scholar] [CrossRef]
- Panayotov, I.V.; Orti, V.; Cuisinier, F.; Yachouh, J. Polyetheretherketone (PEEK) for medical applications. J. Mater. Sci. Mater. Med. 2016, 27, 118. [Google Scholar] [CrossRef]
- Dworak, M.; Rudawski, A.; Markowski, J.; Blazewicz, S. Dynamic mechanical properties of carbon fibre-reinforced PEEK composites in simulated body-fluid. Compos. Struct. 2017, 161, 428–434. [Google Scholar] [CrossRef]
- Zhang, D.; Zhang, Y.; Chen, K.; Zhang, X.; Xu, H. Reducing Taper Fretting Corrosion in Artificial Hip Joints Using a PEEK Femoral Head. J. Mater. Eng. Perform. 2021, 30, 4619–4628. [Google Scholar] [CrossRef]
- Small, G. Outstanding physical properties make PEEK ideal for sealing applications. Seal. Technol. 2014, 2014, 9–12. [Google Scholar] [CrossRef]
- Ma, R.; Tang, T. Current strategies to improve the bioactivity of PEEK. Int. J. Mol. Sci. 2014, 15, 5426–5445. [Google Scholar] [CrossRef] [Green Version]
- Niinomi, M.; Nakai, M.; Hieda, J. Development of new metallic alloys for biomedical applications. Acta Biomater. 2012, 8, 3888–3903. [Google Scholar] [CrossRef]
- Hallab, N.J.; Jacobs, J.J. Dental Applications. In Biomaterials Science; Sakiyama-Elbert, S.E., Zhang, G., Yaszemski, M.J., Eds.; Elsevier Inc.: London, UK, 2020; pp. 1119–1133. [Google Scholar]
- Kurtz, S.M. An Overview of PEEK Biomaterials. In PEEK Biomaterials Handbook; Kurtz, S.M., Ed.; Elsevier Inc.: Amsterdam, The Netherlands, 2019; pp. 3–9. ISBN 9780128125243. [Google Scholar]
- Sumner, D.R. Long-term implant fixation and stress-shielding in total hip replacement. J. Biomech. 2015, 48, 797–800. [Google Scholar] [CrossRef]
- Cheruvu, B.; Venkatarayappa, I.; Goswami, T. Stress Shielding in Cemented Hip Implants Assessed from Computed Tomography. Biomed. J. Sci. Tech. Res. 2019, 18, 1–5. [Google Scholar] [CrossRef]
- Knutsen, A.R.; Lau, N.; Longjohn, D.B.; Ebramzadeh, E.; Sangiorgio, S.N. Periprosthetic femoral bone loss in total hip arthroplasty: Systematic analysis of the effect of stem design. HIP Int. 2017, 27, 26–34. [Google Scholar] [CrossRef]
- Wang, H.; Feng, Q.; Li, N.; Xu, S. Evaluation of metal-ceramic bond characteristics of three dental Co-Cr alloys prepared with different fabrication techniques. J. Prosthet. Dent. 2016, 116, 916–923. [Google Scholar] [CrossRef]
- Čapek, J.; Machová, M.; Fousová, M.; Kubásek, J.; Vojtěch, D.; Fojt, J.; Jablonská, E.; Lipov, J.; Ruml, T. Highly porous, low elastic modulus 316L stainless steel scaffold prepared by selective laser melting. Mater. Sci. Eng. C 2016, 69, 631–639. [Google Scholar] [CrossRef] [PubMed]
- Brizuela, A.; Herrero-Climent, M.; Rios-Carrasco, E.; Rios-Santos, J.; Pérez, R.; Manero, J.; Gil Mur, J. Influence of the Elastic Modulus on the Osseointegration of Dental Implants. Materials 2019, 12, 980. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Wypych, G. Handbook of Polymers, 2nd ed.; ChemTec Publishing: Toronto, ON, Canada, 2016; ISBN 9781895198928. [Google Scholar]
- Ødegaard, K.S.; Torgersen, J.; Elverum, C.W. Structural and Biomedical Properties of Common Additively Manufactured Biomaterials: A Concise Review. Metals 2020, 10, 1677. [Google Scholar] [CrossRef]
- Yang, C.C.; Tang, C.L.; Tzeng, C.Y.; Tsou, H.K. Metallosis after traumatic loosening of Bryan cervical disc arthroplasty: A case report and literature review. Eur. Spine J. 2018, 27, 415–420. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Mallon, S.; Bussis, K.; Beswick, Z.; North, W.T.; Soliman, S.B. Ultrasonographic and radiographic findings of polyethylene component displacement with severe metallosis and metal-induced synovitis following total knee arthroplasty. Knee 2019, 26, 941–950. [Google Scholar] [CrossRef]
- Sochol, K.M.; Charen, D.A.; Andelman, S.M.; Parsons, B.O. Cutaneous metallosis following reverse total shoulder arthroplasty. J. Shoulder Elb. Surg. 2018, 27, e230–e233. [Google Scholar] [CrossRef]
- Lanting, B.A.; Teeter, M.G.; Howard, J.L.; MacDonald, S.J.; Van Citters, D.W. Metal-on-Metal Compared With Metal-on-Polyethylene: The Effect on Trunnion Corrosion in Total Hip Arthroplasty. J. Arthroplasty 2017, 32, 2574–2579. [Google Scholar] [CrossRef]
- Fung, E.S.; Monnot, A.; Kovochich, M.; Unice, K.M.; Tvermoes, B.E.; Galbraith, D.; Finley, B.L.; Paustenbach, D.J. Characteristics of Cobalt-Related Cardiomyopathy in Metal Hip Implant Patients: An Evaluation of 15 Published Reports. Cardiovasc. Toxicol. 2018, 18, 206–220. [Google Scholar] [CrossRef]
- Mohan, N.; Kasprowicz, E. Identification and Management of Cobalt Toxicity: A Case Report of Rapidly Progressing Toxicity after Hip Arthroplasty Revision. Med. Forum 2016, 17, 17–20. [Google Scholar] [CrossRef] [Green Version]
- Peters, R.M.; Willemse, P.; Rijk, P.C.; Hoogendoorn, M.; Zijlstra, W.P. Fatal Cobalt Toxicity after a Non-Metal-on-Metal Total Hip Arthroplasty. Case Rep. Orthop. 2017, 2017, 1–5. [Google Scholar] [CrossRef]
- Ho, V.M.; Arac, A.; Shieh, P.B. Hearing and Vision Loss in an Older Man. JAMA Neurol. 2018, 75, 1439–1440. [Google Scholar] [CrossRef]
- Di Puccio, F.; Mattei, L. Biotribology of artificial hip joints. World J. Orthop. 2015, 6, 77–94. [Google Scholar] [CrossRef]
- Oliveira, C.A.; Candelária, I.S.; Oliveira, P.B.; Figueiredo, A.; Caseiro-Alves, F. Metallosis: A diagnosis not only in patients with metal-on-metal prostheses. Eur. J. Radiol. Open 2015, 2, 3–6. [Google Scholar] [CrossRef] [Green Version]
- Sporer, S.M.; Chalmers, P.N. Cutaneous Manifestation of Metallosis in a Metal-on-Metal Total Hip Arthroplasty After Acetabular Liner Dissociation. J. Arthroplasty 2012, 27, 1580.e13–1580.e16. [Google Scholar] [CrossRef]
- Garnier, R.; Poupon, J.; Djebrani-Oussedik, N.; Langrand, J. Titanium cutaneous metallosis after reverse total shoulder arthroplasty. JSES Rev. Rep. Tech. 2022, 2, 1–4. [Google Scholar] [CrossRef]
- Salem, K.H.; Lindner, N.; Tingart, M.; Elmoghazy, A.D. Severe metallosis-related osteolysis as a cause of failure after total knee replacement. J. Clin. Orthop. Trauma 2020, 11, 165–170. [Google Scholar] [CrossRef]
- Schoon, J.; Ort, M.J.; Huesker, K.; Geissler, S.; Rakow, A. Diagnosis of Metal Hypersensitivity in Total Knee Arthroplasty: A Case Report. Front. Immunol. 2019, 10, 1–8. [Google Scholar] [CrossRef]
- Eliaz, N. Corrosion of Metallic Biomaterials: A Review. Materials 2019, 12, 407. [Google Scholar] [CrossRef] [Green Version]
- Wei, Z.; Tian, P.; Liu, X.; Zhou, B. In vitro degradation, hemolysis, and cytocompatibility of PEO/PLLA composite coating on biodegradable AZ31 alloy. J. Biomed. Mater. Res. Part B Appl. Biomater. 2015, 103, 342–354. [Google Scholar] [CrossRef]
- Wong, H.M.; Yeung, K.W.K.; Lam, K.O.; Tam, V.; Chu, P.K.; Luk, K.D.K.; Cheung, K.M.C. A biodegradable polymer-based coating to control the performance of magnesium alloy orthopaedic implants. Biomaterials 2010, 31, 2084–2096. [Google Scholar] [CrossRef]
- Wen, J.; Lei, J.; Chen, J.; Gou, J.; Li, Y.; Li, L. An intelligent coating based on pH-sensitive hybrid hydrogel for corrosion protection of mild steel. Chem. Eng. J. 2020, 392, 123742. [Google Scholar] [CrossRef]
- Khoury, J.; Maxwell, M.; Cherian, R.E.; Bachand, J.; Kurz, A.C.; Walsh, M.; Assad, M.; Svrluga, R.C. Enhanced bioactivity and osseointegration of PEEK with accelerated neutral atom beam technology. J. Biomed. Mater. Res. Part B Appl. Biomater. 2017, 105, 531–543. [Google Scholar] [CrossRef] [PubMed]
- Green, S. Compounds and Composite Materials. In PEEK Biomaterials Handbook; Kurtz, S.M., Ed.; Elsevier Inc.: Oxford, UK, 2019; pp. 27–51. ISBN 9780128125243. [Google Scholar]
- Mulliken, G.H.; Bichot, N.P.; Ghadooshahy, A.; Sharma, J.; Kornblith, S.; Philcock, M.; Desimone, R. Custom-fit radiolucent cranial implants for neurophysiological recording and stimulation. J. Neurosci. Methods 2015, 241, 146–154. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Shimizu, T.; Fujibayashi, S.; Yamaguchi, S.; Otsuki, B.; Okuzu, Y.; Matsushita, T.; Kokubo, T.; Matsuda, S. In vivo experimental study of anterior cervical fusion using bioactive polyetheretherketone in a canine model. PLoS ONE 2017, 12, e0184495. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Boriani, S.; Tedesco, G.; Ming, L.; Ghermandi, R.; Amichetti, M.; Fossati, P.; Krengli, M.; Mavilla, L.; Gasbarrini, A. Carbon-fiber-reinforced PEEK fixation system in the treatment of spine tumors: A preliminary report. Eur. Spine J. 2018, 27, 874–881. [Google Scholar] [CrossRef]
- Liu, Y.; Zhang, J.; Pang, Z. Numerical and experimental investigation into the subsequent thermal cycling during selective laser melting of multi-layer 316L stainless steel. Opt. Laser Technol. 2018, 98, 23–32. [Google Scholar] [CrossRef]
- Koutsoukis, T.; Zinelis, S.; Eliades, G.; Al-Wazzan, K.; Al Rifaiy, M.; Al Jabbari, Y.S. Selective Laser Melting Technique of Co-Cr Dental Alloys: A Review of Structure and Properties and Comparative Analysis with Other Available Techniques. J. Prosthodont. 2015, 24, 303–312. [Google Scholar] [CrossRef]
- Fu, C.H.; Guo, Y.B. Three-Dimensional Temperature Gradient Mechanism in Selective Laser Melting of Ti-6Al-4V. J. Manuf. Sci. Eng. 2014, 136, 061004. [Google Scholar] [CrossRef]
- Kurtz, S.M. Synthesis and Processing of PEEK for Surgical Implants. In PEEK Biomaterials Handbook; Kurtz, S.M., Ed.; Elsevier Inc.: Oxford, UK, 2019; pp. 11–25. ISBN 9780128125243. [Google Scholar]
- Fink, J.K. High Performance Polymers, 2nd ed.; Elsevier Inc.: Oxford, UK, 2014; ISBN 9780323312226. [Google Scholar]
- Green, S.; Schlegel, J. A polyaryletherketone biomaterial for use in medical implant applications. In Proceedings of the Polymers for the Medical Industry: Conference Proceedings, Brussels, Belgium, 14–15 May 2001; pp. 1–7. [Google Scholar]
- Kurtz, S.M.; Devine, J.N. PEEK biomaterials in trauma, orthopedic, and spinal implants. Biomaterials 2007, 28, 4845–4869. [Google Scholar] [CrossRef] [Green Version]
- Kemmish, D.J.; Wilson, B. Aromatic Polyetherketones. U.S. Patent 6,909,015 B2, 21 June 2005. [Google Scholar]
- Li, K.; Yeung, C.Y.; Yeung, K.W.K.; Tjong, S.C. Sintered hydroxyapatite/polyetheretherketone nanocomposites: Mechanical behavior and biocompatibility. Adv. Eng. Mater. 2012, 14, 155–165. [Google Scholar] [CrossRef]
- Ma, R.; Fang, L.; Luo, Z.; Zheng, R.; Song, S.; Weng, L.; Lei, J. Fabrication and characterization of modified-hydroxyapatite/polyetheretherketone coating materials. Appl. Surf. Sci. 2014, 314, 341–347. [Google Scholar] [CrossRef]
- Mahjoubi, H.; Buck, E.; Manimunda, P.; Farivar, R.; Chromik, R.; Murshed, M.; Cerruti, M. Surface phosphonation enhances hydroxyapatite coating adhesion on polyetheretherketone and its osseointegration potential. Acta Biomater. 2017, 47, 149–158. [Google Scholar] [CrossRef]
- Olivares-Navarrete, R.; Hyzy, S.L.; Slosar, P.J.; Schneider, J.M.; Schwartz, Z.; Boyan, B.D. Implant materials generate different peri-implant inflammatory factors: Poly-ether-ether-ketone promotes fibrosis and microtextured titanium promotes osteogenic factors. Spine 2015, 40, 399–404. [Google Scholar] [CrossRef]
- Davis, R.; Singh, A.; Jackson, M.J.; Coelho, R.T.; Prakash, D.; Charalambous, C.P.; Ahmed, W.; Da Silva, L.R.R.; Lawrence, A.A. A comprehensive review on metallic implant biomaterials and their subtractive manufacturing. Int. J. Adv. Manuf. Technol. 2022, 120, 1473–1530. [Google Scholar] [CrossRef]
- Li, J.J.; Zreiqat, H. Tissue response to biomaterials. Encycl. Biomed. Eng. 2019, 1–3, 270–277. [Google Scholar] [CrossRef]
- Kasemo, B. Biological surface science Bengt. Surf. Sci. 2002, 500, 656–677. [Google Scholar] [CrossRef]
- Almasi, D.; Iqbal, N.; Sadeghi, M.; Sudin, I.; Abdul Kadir, M.R.; Kamarul, T. Preparation Methods for Improving PEEK’s Bioactivity for Orthopedic and Dental Application: A Review. Int. J. Biomater. 2016, 2016, 8202653. [Google Scholar] [CrossRef] [Green Version]
- Michiardi, A.; Aparicio, C.; Ratner, B.D.; Planell, J.A.; Gil, J. The influence of surface energy on competitive protein adsorption on oxidized NiTi surfaces. Biomaterials 2007, 28, 586–594. [Google Scholar] [CrossRef]
- Liamas, E.; Kubiak-Ossowska, K.; Black, R.A.; Thomas, O.R.T.; Zhang, Z.J.; Mulheran, P.A. Adsorption of Fibronectin Fragment on Surfaces Using Fully Atomistic Molecular Dynamics Simulations. Int. J. Mol. Sci. 2018, 19, 3321. [Google Scholar] [CrossRef] [Green Version]
- Tagaya, M.; Ikoma, T.; Hanagata, N.; Tanaka, J. Analytical Investigation of Protein Mediation Between Biomaterials and Cells. Mater. Express 2012, 2, 1–22. [Google Scholar] [CrossRef]
- Dos Santos, F.S.F.; Vieira, M.; Da Silva, H.N.; Tomás, H.; Fook, M.V.L. Surface Bioactivation of Polyether Ether Ketone (PEEK) by Sulfuric Acid and Piranha Solution: Influence of the Modification Route in Capacity for Inducing Cell Growth. Biomolecules 2021, 11, 1260. [Google Scholar] [CrossRef] [PubMed]
- Zheng, Y.; Liu, L.; Xiong, C.; Zhang, L. Enhancement of bioactivity on modified polyetheretherketone surfaces with –COOH, –OH and –PO4H2 functional groups. Mater. Lett. 2018, 213, 84–87. [Google Scholar] [CrossRef]
- Ouyang, L.; Zhao, Y.; Jin, G.; Lu, T.; Li, J.; Qiao, Y.; Ning, C.; Zhang, X.; Chu, P.K.; Liu, X. Influence of sulfur content on bone formation and antibacterial ability of sulfonated PEEK. Biomaterials 2016, 83, 115–126. [Google Scholar] [CrossRef] [PubMed]
- Liu, X.; Huang, L.; Zhang, H.; Liu, Y.; Wu, C.; Luo, Q.; Yin, F.; Yan, X.; Zhao, J.; Su, Y.; et al. Facile Amidogen Bio-Activation Method Can Boost the Soft Tissue Integration on 3D Printed Poly–Ether–Ether–Ketone Interface. Adv. Mater. Interfaces 2021, 8, 2100547. [Google Scholar] [CrossRef]
- Chen, M.; Ouyang, L.; Lu, T.; Wang, H.; Meng, F.; Yang, Y.; Ning, C.; Ma, J.; Liu, X. Enhanced Bioactivity and Bacteriostasis of Surface Fluorinated Polyetheretherketone. ACS Appl. Mater. Interfaces 2017, 9, 16824–16833. [Google Scholar] [CrossRef]
- Terpiłowski, K.; Wiącek, A.E.; Jurak, M. Influence of nitrogen plasma treatment on the wettability of polyetheretherketone and deposited chitosan layers. Adv. Polym. Technol. 2018, 37, 1557–1569. [Google Scholar] [CrossRef] [Green Version]
- Gan, K.; Liu, H.; Jiang, L.; Liu, X.; Song, X.; Niu, D.; Chen, T.; Liu, C. Bioactivity and antibacterial effect of nitrogen plasma immersion ion implantation on polyetheretherketone. Dent. Mater. 2016, 32, e263–e274. [Google Scholar] [CrossRef]
- Wang, H.; Lu, T.; Meng, F.; Zhu, H.; Liu, X. Enhanced osteoblast responses to poly ether ether ketone surface modified by water plasma immersion ion implantation. Colloids Surfaces B Biointerfaces 2014, 117, 89–97. [Google Scholar] [CrossRef]
- Zhao, Y.; Wong, H.M.; Lui, S.C.; Chong, E.Y.W.; Wu, G.; Zhao, X.; Wang, C.; Pan, H.; Cheung, K.M.C.; Wu, S.; et al. Plasma Surface Functionalized Polyetheretherketone for Enhanced Osseo-Integration at Bone-Implant Interface. ACS Appl. Mater. Interfaces 2016, 8, 3901–3911. [Google Scholar] [CrossRef]
- Wiacek, A.E.; Terpiłowski, K.; Jurak, M.; Worzakowska, M. Low-temperature air plasma modification of chitosan-coated PEEK biomaterials. Polym. Test. 2016, 50, 325–334. [Google Scholar] [CrossRef]
- Riveiro, A.; Maçon, A.L.B.; Del Val, J.; Comesaña, R.; Pou, J. Laser surface texturing of polymers for biomedical applications. Front. Phys. 2018, 6, 16. [Google Scholar] [CrossRef]
- Riveiro, A.; Soto, R.; Comesaña, R.; Boutinguiza, M.; Del Val, J.; Quintero, F.; Lusquiños, F.; Pou, J. Laser surface modification of PEEK. Appl. Surf. Sci. 2012, 258, 9437–9442. [Google Scholar] [CrossRef]
- Zheng, Y.; Xiong, C.; Wang, Z.; Li, X.; Zhang, L. A combination of CO2 laser and plasma surface modification of poly(etheretherketone) to enhance osteoblast response. Appl. Surf. Sci. 2015, 344, 79–88. [Google Scholar] [CrossRef]
- Verma, M.; Rana, A.; Vidyasagar, K.E.C.; Kalyansundaram, D.; Saha, S. Protein Patterning on Microtextured Polymeric Nanobrush Templates Obtained by Nanosecond Fiber Laser. Macromol. Biosci. 2022, 2100454, 2100454. [Google Scholar] [CrossRef]
- Romano, A.; Angelini, A.; Rossegger, E.; Palmara, G.; Castellino, M.; Frascella, F.; Chiappone, A.; Chiadò, A.; Sangermano, M.; Schlögl, S.; et al. Laser-Triggered Writing and Biofunctionalization of Thiol-Ene Networks. Macromol. Rapid Commun. 2020, 41, 2000084. [Google Scholar] [CrossRef]
- Wakelin, E.A.; Yeo, G.C.; McKenzie, D.R.; Bilek, M.M.M.; Weiss, A.S. Plasma ion implantation enabled bio-functionalization of PEEK improves osteoblastic activity. APL Bioeng. 2018, 2, 026109. [Google Scholar] [CrossRef] [Green Version]
- Mehdizadeh Omrani, M.; Kumar, H.; Mohamed, M.G.A.; Golovin, K.; Milani, A.S.; Hadjizadeh, A.; Kim, K. Polyether ether ketone surface modification with plasma and gelatin for enhancing cell attachment. J. Biomed. Mater. Res. Part B Appl. Biomater. 2021, 109, 622–629. [Google Scholar] [CrossRef]
- Przykaza, K.; Woźniak, K.; Jurak, M.; Wiącek, A.E. Characteristics of Polypeptide/Phospholipid Monolayers on Water and the Plasma-Activated Polyetheretherketone Support. J. Surfactants Deterg. 2019, 22, jsde-12323. [Google Scholar] [CrossRef]
- He, Y.; Wang, C.; Wang, C.; Xiao, Y.; Lin, W. An Overview on Collagen and Gelatin-Based Cryogels: Fabrication, Classification, Properties and Biomedical Applications. Polymers 2021, 13, 2299. [Google Scholar] [CrossRef]
- Rodrigues, I.C.P.; Woigt, L.F.; Pereira, K.D.; Luchessi, A.D.; Lopes, É.S.N.; Webster, T.J.; Gabriel, L.P. Low-cost hybrid scaffolds based on polyurethane and gelatin. J. Mater. Res. Technol. 2020, 9, 7777–7785. [Google Scholar] [CrossRef]
- Khoury, J.; Selezneva, I.; Pestov, S.; Tarassov, V.; Ermakov, A.; Mikheev, A.; Lazov, M.; Kirkpatrick, S.R.; Shashkov, D.; Smolkov, A. Surface bioactivation of PEEK by neutral atom beam technology. Bioact. Mater. 2019, 4, 132–141. [Google Scholar] [CrossRef] [PubMed]
- Zheng, Y.; Liu, L.; Ma, Y.; Xiao, L.; Liu, Y. Enhanced Osteoblasts Responses to Surface-Sulfonated Polyetheretherketone via a Single-Step Ultraviolet-Initiated Graft Polymerization. Ind. Eng. Chem. Res. 2018, 57, 10403–10410. [Google Scholar] [CrossRef]
- Zheng, Y.; Liu, L.; Xiao, L.; Zhang, Q.; Liu, Y. Enhanced osteogenic activity of phosphorylated polyetheretherketone via surface-initiated grafting polymerization of vinylphosphonic acid. Colloids Surf. B Biointerfaces 2019, 173, 591–598. [Google Scholar] [CrossRef] [PubMed]
- Kim, K.H.; Im, S.H.; Park, B.J. Long-term stable hydrophilic surface modification of poly(ether ether ketone) via the multilayered chemical grafting method. J. Appl. Polym. Sci. 2018, 135, 46042. [Google Scholar] [CrossRef]
- Štefaníková, R.; Kretková, T.; Kuzminova, A.; Hanuš, J.; Vaidulych, M.; Kylián, O.; Biederman, H. Influence of atmospheric pressure dielectric barrier discharge on wettability and drying of poly(ether-ether-ketone) foils. Polym. Degrad. Stab. 2018, 150, 114–121. [Google Scholar] [CrossRef]
- Poulsson, A.H.C.; Eglin, D.; Geoff Richards, R. Surface Modification Techniques of PEEK, Including Plasma Surface Treatment. In PEEK Biomaterials Handbook; Kurtz, S.M., Ed.; Elsevier Inc.: Oxford, UK, 2019; pp. 179–201. ISBN 9780128125243. [Google Scholar]
- Han, C.-M.; Jang, T.-S.; Kim, H.-E.; Koh, Y.-H. Creation of nanoporous TiO2 surface onto polyetheretherketone for effective immobilization and delivery of bone morphogenetic protein. J. Biomed. Mater. Res. Part A 2014, 102, 793–800. [Google Scholar] [CrossRef]
- Wen, J.; Lu, T.; Wang, X.; Xu, L.; Wu, Q.; Pan, H.; Wang, D.; Liu, X.; Jiang, X. In Vitro and in Vivo Evaluation of Silicate-Coated Polyetheretherketone Fabricated by Electron Beam Evaporation. ACS Appl. Mater. Interfaces 2016, 8, 13197–13206. [Google Scholar] [CrossRef]
- Tsou, H.-K.; Chi, M.-H.; Hung, Y.-W.; Chung, C.-J.; He, J.-L. In Vivo Osseointegration Performance of Titanium Dioxide Coating Modified Polyetheretherketone Using Arc Ion Plating for Spinal Implant Application. Biomed Res. Int. 2015, 2015, 328943. [Google Scholar] [CrossRef] [Green Version]
- Walsh, W.R.; Bertollo, N.; Christou, C.; Schaffner, D.; Mobbs, R.J. Plasma-sprayed titanium coating to polyetheretherketone improves the bone-implant interface. Spine J. 2015, 15, 1041–1049. [Google Scholar] [CrossRef]
- Lu, T.; Wen, J.; Qian, S.; Cao, H.; Ning, C.; Pan, X.; Jiang, X.; Liu, X.; Chu, P.K. Enhanced osteointegration on tantalum-implanted polyetheretherketone surface with bone-like elastic modulus. Biomaterials 2015, 51, 173–183. [Google Scholar] [CrossRef]
- Lu, T.; Qian, S.; Meng, F.; Ning, C.; Liu, X. Enhanced osteogenic activity of poly ether ether ketone using calcium plasma immersion ion implantation. Colloids Surf. B Biointerfaces 2016, 142, 192–198. [Google Scholar] [CrossRef] [Green Version]
- Almasi, D.; Izman, S.; Assadian, M.; Ghanbari, M.; Abdul Kadir, M.R. Crystalline ha coating on PEEK via chemical deposition. Appl. Surf. Sci. 2014, 314, 1034–1040. [Google Scholar] [CrossRef]
- Johansson, P.; Jimbo, R.; Naito, Y.; Kjellin, P.; Currie, F.; Wennerberg, A. Polyether ether ketone implants achieve increased bone fusion when coated with nano-sized hydroxyapatite: A histomorphometric study in rabbit bone. Int. J. Nanomed. 2016, 11, 1435–1442. [Google Scholar] [CrossRef] [Green Version]
- Buck, E.; Li, H.; Cerruti, M. Surface Modification Strategies to Improve the Osseointegration of Poly(etheretherketone) and Its Composites. Macromol. Biosci. 2020, 20, 1900271. [Google Scholar] [CrossRef]
- Kienle, A.; Graf, N.; Wilke, H.J. Does impaction of titanium-coated interbody fusion cages into the disc space cause wear debris or delamination? Spine J. 2016, 16, 235–242. [Google Scholar] [CrossRef] [Green Version]
- Torstrick, F.B.; Lin, A.S.P.; Potter, D.; Safranski, D.L.; Sulchek, T.A.; Gall, K.; Guldberg, R.E. Porous PEEK improves the bone-implant interface compared to plasma-sprayed titanium coating on PEEK. Biomaterials 2018, 185, 106–116. [Google Scholar] [CrossRef]
- Robotti, P.; Zappini, G. Thermal Plasma Spray Deposition of Titanium and Hydroxyapatite on PEEK Implants. In PEEK Biomaterials Handbook; Kurtz, S.M., Ed.; Elsevier Inc.: Oxford, UK, 2019; pp. 147–177. ISBN 9780128125243. [Google Scholar]
- Sun, L.; Berndt, C.C.; Gross, K.A.; Kucuk, A. Material Fundamentals and Clinical Performance of Plasma- Sprayed Hydroxyapatite Coatings: A Review. J. Biomed. Mater. Res. 2001, 58, 570–592. [Google Scholar] [CrossRef]
- Wu, X.; Liu, X.; Wei, J.; Ma, J.; Deng, F.; Wei, S. Nano-TiO2/PEEK bioactive composite as a bone substitute material: In vitro and in vivo studies. Int. J. Nanomed. 2012, 7, 1215–1225. [Google Scholar] [CrossRef] [Green Version]
- Zhang, J.; Wei, W.; Yang, L.; Pan, Y.; Wang, X.; Wang, T.; Tang, S.; Yao, Y.; Hong, H.; Wei, J. Stimulation of cell responses and bone ingrowth into macro-microporous implants of nano-bioglass/polyetheretherketone composite and enhanced antibacterial activity by release of hinokitiol. Colloids Surf. B Biointerfaces 2018, 164, 347–357. [Google Scholar] [CrossRef]
- Ma, R.; Yu, Z.; Tang, S.; Pan, Y.; Wei, J.; Tang, T. Osseointegration of nanohydroxyapatite- or nano-calcium silicate-incorporated polyetheretherketone bioactive composites in vivo. Int. J. Nanomed. 2016, 11, 6023–6033. [Google Scholar] [CrossRef]
- Petrovic, L.; Pohle, D.; Münstedt, H.; Rechtenwald, T.; Schlegel, K.A.; Rupprecht, S. Effect of βTCP filled polyetheretherketone on osteoblast cell proliferation in vitro. J. Biomed. Sci. 2006, 13, 41–46. [Google Scholar] [CrossRef] [PubMed]
- Von Wilmonsky, C.; Lutz, R.; Meisel, U.; Srour, S.; Rupprecht, S.; Toyoshima, T.; Nkenke, E.; Schlegel, K.A.; Pohle, D.; Münstedt, H.; et al. In vivo evaluation of B-TCP containing 3D laser sintered poly(ether ether ketone) composites in pigs. J. Bioact. Compat. Polym. 2009, 24, 169–184. [Google Scholar] [CrossRef] [Green Version]
- Monich, P.R.; Berti, F.V.; Porto, L.M.; Henriques, B.; Novaes de Oliveira, A.P.; Fredel, M.C.; Souza, J.C.M. Physicochemical and biological assessment of PEEK composites embedding natural amorphous silica fibers for biomedical applications. Mater. Sci. Eng. C 2017, 79, 354–362. [Google Scholar] [CrossRef] [PubMed]
- Wang, L.; He, S.; Wu, X.; Liang, S.; Mu, Z.; Wei, J.; Deng, F.; Deng, Y.; Wei, S. Polyetheretherketone/nano-fluorohydroxyapatite composite with antimicrobial activity and osseointegration properties. Biomaterials 2014, 35, 6758–6775. [Google Scholar] [CrossRef] [PubMed]
- Wong, K.L.; Wong, C.T.; Liu, W.C.; Pan, H.B.; Fong, M.K.; Lam, W.M.; Cheung, W.L.; Tang, W.M.; Chiu, K.Y.; Luk, K.D.K.; et al. Mechanical properties and in vitro response of strontium-containing hydroxyapatite/polyetheretherketone composites. Biomaterials 2009, 30, 3810–3817. [Google Scholar] [CrossRef]
- Ma, R.; Guo, D. Evaluating the bioactivity of a hydroxyapatite-incorporated polyetheretherketone biocomposite. J. Orthop. Surg. Res. 2019, 14, 32. [Google Scholar] [CrossRef]
- Ma, R.; Weng, L.; Bao, X.; Ni, Z.; Song, S.; Cai, W. Characterization of in situ synthesized hydroxyapatite/polyetheretherketone composite materials. Mater. Lett. 2012, 71, 117–119. [Google Scholar] [CrossRef]
- Zhong, G.; Vaezi, M.; Mei, X.; Liu, P.; Yang, S. Strategy for Controlling the Properties of Bioactive Poly-Ether-Ether-Ketone/Hydroxyapatite Composites for Bone Tissue Engineering Scaffolds. ACS Omega 2019, 4, 19238–19245. [Google Scholar] [CrossRef] [Green Version]
- Ma, R.; Li, Q.; Wang, L.; Zhang, X.; Fang, L.; Luo, Z.; Xue, B.; Ma, L. Mechanical properties and in vivo study of modified-hydroxyapatite/polyetheretherketone biocomposites. Mater. Sci. Eng. C 2017, 73, 429–439. [Google Scholar] [CrossRef] [Green Version]
- Converse, G.L.; Yue, W.; Roeder, R.K. Processing and tensile properties of hydroxyapatite-whisker-reinforced polyetheretherketone. Biomaterials 2007, 28, 927–935. [Google Scholar] [CrossRef]
- Wang, L.; Weng, L.; Song, S.; Zhang, Z.; Tian, S.; Ma, R. Characterization of polyetheretherketone-hydroxyapatite nanocomposite materials. Mater. Sci. Eng. A 2011, 528, 3689–3696. [Google Scholar] [CrossRef]
- Ma, R.; Weng, L.; Bao, X.; Song, S.; Zhang, Y. In vivo biocompatibility and bioactivity of in situ synthesized hydroxyapatite/polyetheretherketone composite materials. J. Appl. Polym. Sci. 2012, 127, 2581–2587. [Google Scholar] [CrossRef]
- Fabris, D.; Moura, J.P.A.; Fredel, M.C.; Souza, J.C.M.; Silva, F.S.; Henriques, B. Biomechanical analyses of one-piece dental implants composed of titanium, zirconia, PEEK, CFR-PEEK, or GFR-PEEK: Stresses, strains, and bone remodeling prediction by the finite element method. J. Biomed. Mater. Res.Part B Appl. Biomater. 2022, 110, 79–88. [Google Scholar] [CrossRef]
- Uri, O.; Folman, Y.; Laufer, G.; Behrbalk, E. A Novel Spine Fixation System Made Entirely of Carbon-Fiber-Reinforced PEEK Composite: An In Vitro Mechanical Evaluation. Adv. Orthop. 2020, 2020, 4796136. [Google Scholar] [CrossRef]
- Deng, Y.; Zhou, P.; Liu, X.; Wang, L.; Xiong, X.; Tang, Z.; Wei, J.; Wei, S. Preparation, characterization, cellular response and in vivo osseointegration of polyetheretherketone/nano-hydroxyapatite/carbon fiber ternary biocomposite. Colloids Surf. B Biointerfaces 2015, 136, 64–73. [Google Scholar] [CrossRef]
- Tan, J.; Natarajan, E.; Lim, W.; Ramesh, S.; Ang, C.; Parasuraman, S.; Singh, D.K.J. Effects of bone-plate materials on the healing process of fractured tibia bone under time-varying conditions: A finite element analysis. Mater. Res. Express 2021, 8, 095308. [Google Scholar] [CrossRef]
- Zhou, K.; Yang, H. Effects of Bone-Plate Material on the Predicted Stresses in the Tibial Shaft Comminuted Fractures: A Finite Element Analysis. J. Investig. Surg. 2020, 35, 132–140. [Google Scholar] [CrossRef]
- Loeb, A.E.; Mitchell, S.L.; Osgood, G.M.; Shafiq, B. Catastrophic Failure of a Carbon-Fiber-Reinforced Polyetheretherketone Tibial Intramedullary Nail. J. Bone Jt. Surg. 2018, 8, e83. [Google Scholar] [CrossRef]
- Merolli, A.; Rocchi, L.; De Spirito, M.; Federico, F.; Morini, A.; Mingarelli, L.; Fanfani, F. Debris of carbon-fibers originated from a CFRP (PEEK) wrist-plate triggered a destruent synovitis in human. J. Mater. Sci. Mater. Med. 2016, 27, 50. [Google Scholar] [CrossRef]
- Tullberg, T. Failure of a Carbon Fiber Implant. Spine 1998, 23, 1804–1806. [Google Scholar] [CrossRef]
- Díez-Pascual, A.M.; Díez-Vicente, A.L. Nano-TiO2 Reinforced PEEK/PEI Blends as Biomaterials for Load-Bearing Implant Applications. ACS Appl. Mater. Interfaces 2015, 7, 5561–5573. [Google Scholar] [CrossRef] [PubMed]
- Díez-Pascual, A.M.; Xu, C.; Luque, R. Development and characterization of novel poly(ether ether ketone)/ZnO bionanocomposites. J. Mater. Chem. B 2014, 2, 3065–3078. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Díez-Pascual, A.M.; Díez-Vicente, A.L. Development of nanocomposites reinforced with carboxylated poly(ether ether ketone) grafted to zinc oxide with superior antibacterial properties. ACS Appl. Mater. Interfaces 2014, 6, 3729–3741. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Mulla, M.Z.; Rahman, M.R.T.; Marcos, B.; Tiwari, B.; Pathania, S. Poly lactic acid (PLA) Nanocomposites: Effect of Inorganic Nanoparticles Reinforcement on its Performance and Food Packaging Applications. Molecules 2021, 26, 1967. [Google Scholar] [CrossRef] [PubMed]
- Hao, L.; Hu, Y.; Zhang, Y.; Wei, W.; Hou, X.; Guo, Y.; Hu, X.; Jiang, D. Enhancing the mechanical performance of poly(ether ether ketone)/zinc oxide nanocomposites to provide promising biomaterials for trauma and orthopedic implants. RSC Adv. 2018, 8, 27304–27317. [Google Scholar] [CrossRef] [Green Version]
- Montaño-Machado, V.; Chevallier, P.; Bonilla-Gameros, L.; Copes, F.; Quarta, C.; Kú-Herrera, J.d.J.; Soriano, F.; Padilla-Gainza, V.; Morales, G.; Montovani, D. Develpment of multifunctional materials based on PEEK with improved biological performance.pdf. Materials 2021, 14, 1047. [Google Scholar] [CrossRef]
- Bragaglia, M.; Cherubini, V.; Nanni, F. PEEK-TiO2 composites with enhanced UV resistance. Compos. Sci. Technol. 2020, 199, 108365. [Google Scholar] [CrossRef]
- Zimmer. Available online: https://www.zimmerbiomet.lat/en/medical-professionals/hip/product/versys-epoch-fullcoat.html (accessed on 28 December 2022).
- Saltzman, B.M.; Haughom, B.; Oni, J.K.; Levine, B.R. Chronic Infection Leading to Failure of a Composite Femoral Stem: A Report of Two Cases. HSS J. Musculoskelet. J. Hosp. Speéc. Surg. 2014, 10, 180–185. [Google Scholar] [CrossRef] [Green Version]
- Crossman, N.; Wang, J.S.; Kukreja, M.M.; Kang, P.S. Catastrophic Failure of Zimmer Ver Sys Epoch Femoral Stem at the Fiber Metal Mesh Junction. Biomed. J. Sci. Tech. Res. 2020, 31, 24591–24594. [Google Scholar] [CrossRef]
- Medtronic. Available online: https://www.medtronic.com/us-en/healthcare-professionals/therapies-procedures/spinal-orthopaedic/interbody-science/indications-safety-warnings/anatomic-peek-ptc.html (accessed on 28 December 2022).
- Honigmann, P.; Sharma, N.; Okolo, B.; Popp, U.; Msallem, B.; Thieringer, F.M. Patient-Specific Surgical Implants Made of 3D Printed PEEK: Material, Technology, and Scope of Surgical Application. Biomed Res. Int. 2018, 2018, 4520636. [Google Scholar] [CrossRef]
- Prechtel, A.; Stawarczyk, B.; Hickel, R.; Edelhoff, D.; Reymus, M. Fracture load of 3D printed PEEK inlays compared with milled ones, direct resin composite fillings, and sound teeth. Clin. Oral Investig. 2020, 24, 3457–3466. [Google Scholar] [CrossRef] [Green Version]
- Rinaldi, M.; Ghidini, T.; Cecchini, F.; Brandao, A.; Nanni, F. Additive layer manufacturing of poly (ether ether ketone) via FDM. Compos. Part B Eng. 2018, 145, 162–172. [Google Scholar] [CrossRef]
- Toso, S.M.; Menzel, K.; Motzkus, Y.; Adolphs, N.; Hoffmeister, B.; Raguse, J.-D. Patient-Specific Implant in Prosthetic Craniofacial Reconstruction. J. Craniofac. Surg. 2015, 26, 2133–2135. [Google Scholar] [CrossRef]












| Material | Density (g/cm3) | Melting Temperature (°C) | Reference |
|---|---|---|---|
| Cortical bone | 1.5–2 | - | [23] |
| Trabecular bone | 0.2–0.6 | - | [23] |
| PEEK | 1.4 | 304–391 | [25] |
| 316L stainless steel | 7.99 | 1380 | [23,50] |
| Co-Cr-Mo | 8.3 | 1350–1430 | [51] |
| Ti-6Al-4V | 4.43 | 1655 | [52] |
| Property | Value | Reference |
|---|---|---|
| Elastic modulus | 2.0–4.0 GPa | [25,59] |
| Tensile strength | 84 MPa | [59] |
| Compressive strength | 112 MPa | [59] |
| Elongation at break | 3.5% | [58] |
| Tg | 143 | [56] |
| Tc | 314 | [58] |
| Tm | 343 | [58] |
| Filler | Processing Method | Bioactivity Highlight | Reference |
|---|---|---|---|
| nano-TiO2 | Dispersion in ethanol and compression molding | In vivo studies showed that the percent of bone volume on the n-TiO2/PEEK surface was approximately twice as large as that of PEEK. | [108] |
| nano-bioglass | particle leaching and compression molding | The apatite mineralization ability in simulated body fluid (SBF) was significantly improved in the composite. | [109] |
| nano-calcium silicate | High-speed ball mill and injection molding | In vivo tests revealed that the composite promoted osseointegration at the bone/implant interface compared to PEEK. | [110] |
| β-tricalcium phosphate | laser sintering | In vivo evaluation showed that the composite exhibited bone–implant contact while the control group was encapsulated by fibrous tissue. | [112] |
| natural amorphous silica fibers | Ball mill and compression molding | The addition of fibers into PEEK stimulated the metabolic activity of fibroblasts grown on the composites compared to the metabolic activity of neat PEEK. | [113] |
| HA doped with fluorine | Dispersion in alcohol and compression molding | The composite exhibited enhanced antibacterial activity and osseointegration. | [114] |
| HA doped with Sr | Solvent dispersion and compression molding | The addition of the filler enhanced the bioactivity of the material. | [115] |
| Material | Processing Method | Elastic Modulus (GPa) | Tensile Strength (MPa) | Fracture Strain (%) | Reference |
|---|---|---|---|---|---|
| Cortical bone | - | 7–25 | 50–150 | 1–3 | [23,58] |
| PEEK/ HA | Ball mill/ Injection molding | 7.2 (30 wt% HA) 10.6 (40 wt% HA) | 56 (30 wt% HA) 45 (40 wt% HA) | - | [116] |
| PEEK/ HA | In situ synthesis | - | 106 (2.6 vol% HA) 99 (5.6 vol% HA) 75 (8.7 vol% HA) | - | [117] |
| PEEK/ nHA | Particles dispersion/cold compression/sintering | 4.79 ± 0.16 (15.1 vol% nHA) 5.76 ± 0.09 (21.9 vol% nHA) 6.73 ± 0.12 (29.2 vol% nHA) 7.63 ± 0.09 (38.2 vol% nHA) | 63.9 ± 1.8 (15.1 vol% nHA) 60.5 ± 2.2 (21.9 vol% nHA) 54.3 ± 2.7 (29.2 vol% nHA) 43.1 ± 1.5 (38.2 vol% nHA) | 1.31 ± 0.07 (15.1 vol% nHA) 1.08 ± 0.05 (21.9 vol% nHA) 0.86 ± 0.03 (29.2 vol% nHA) 0.58 ± 0.04 (38.2 vol% nHA) | [58] |
| PEEK/ HA | Mixing/ Hot compression molding | ~0.23 (5 wt% HA) ~0.45 (15 wt% HA) 0.58 (20 wt% HA) | 71.46 (5 wt% HA) ~35 (15 wt% HA) ~11 (20 wt% HA) | - | [119] |
| PEEK/ mHA | Mixing/ Hot compression molding | ~0.36 (5 wt% mHA) ~0.55 (15 wt% mHA) 0.72 (20 wt% mHA) | 76.21 (5 wt% mHA) ~53 (15 wt% mHA) ~40 (20 wt% mHA) | - | [119] |
| Nanoparticle | Processing Method | Key Finds | Reference |
|---|---|---|---|
| Nanorod HA | Particles dispersion/cold compression/sintering | The nanocomposites with 21.6 and 29.2 vol% had tensile strength and fracture strain close to the human cortical bones. Furthermore, the higher volume of nHA triggered better bioactivity and biocompatibility. | [58] |
| HA | Ball mill/ Injection molding | The tensile strength and elastic modulus of the composite with 30 wt% closely match these values for cortical bone. In vivo tests showed a higher bone contact for the composite compared to raw PEEK. | [116] |
| HA | In situ synthesis | The processing method promoted a better interfacial bonding between PEEK and HA, resulting in better mechanical properties. The PEEK/5.6 vol% of HA demonstrated desirable biocompatibility without apparent toxicity to the animal. In addition, the in vivo bioactivity showed that higher HA content promotes a faster new bone tissue growth around the implant made of PEEK/HA. | [117,122] |
| HA | Compression molding | The PEEK/40 vol% composite showed good biocompatibility and the compressive strength was in range with the cortical bone. | [118] |
| mHA | Mixing/ compression molding | The composite with 5 wt% of mHA showed higher tensile strength, 23% higher than pure PEEK. Higher growth of the bone tissue observed in the in vivo test was achieved for the same composite composition with 5 wt% of mHA. | [119] |
| 25 wt% nHA/20 wt% CFR | Melt blending and injection molding | The ternary composite presented an elastic modulus higher than the values usually found for the PEEK/HA composites. Furthermore, the ternary composite improved biocompatibility in vitro and promoted osseointegration in vivo. | [125] |
| s-ZnO | Cryogenic ball-milling/compression molding | The PEEK/sZnO displayed superior stiffness and strength compared to the neat polymer and the composites with ZnO without modification. Moreover, the antibacterial activity was improved with increasing nanoparticle content. | [130] |
| hydroxylated ZnO | Extrusion | The hydroxylated PEEK was grafted in the carboxylated PEEK to prepare masterbatches. Then, the masterbatches were compounded with PEEK. A superior stiffness and strength were exhibited for the composites with polymer-grafted nanoparticles compared to the neat PEEK. Moreover, the antibacterial activity increased raising the nanoparticle content. | [131] |
| s-ZnO | Twin-screw extrusion/injection molding | The addition of s-ZnO increased the tensile strength and elastic modulus. However, the improvement in the mechanical properties was inferior to the [130] study. It can be associated with the processing method, along with the use difference of different silane coupling. Cell viability was enhanced for the PEEK/ZnO composites, as well as the antibacterial activity | [134] |
| ZnO | Co-rotating twin-screw extrusion | The incorporation of ZnO nanoparticles did not improve the mechanical properties. Nonetheless, a positive effect on biological performance was observed after incorporating ZnO. | [135] |
| TiO2 | Planetary mixer/single-screw extrusion | The incorporation of TiO2 lightly increased the material’s stiffness and did not interfere with the tensile strength. | [136] |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Senra, M.R.; Marques, M.d.F.V.; Monteiro, S.N. Poly (Ether-Ether-Ketone) for Biomedical Applications: From Enhancing Bioactivity to Reinforced-Bioactive Composites—An Overview. Polymers 2023, 15, 373. https://doi.org/10.3390/polym15020373
Senra MR, Marques MdFV, Monteiro SN. Poly (Ether-Ether-Ketone) for Biomedical Applications: From Enhancing Bioactivity to Reinforced-Bioactive Composites—An Overview. Polymers. 2023; 15(2):373. https://doi.org/10.3390/polym15020373
Chicago/Turabian StyleSenra, Mônica Rufino, Maria de Fátima Vieira Marques, and Sergio Neves Monteiro. 2023. "Poly (Ether-Ether-Ketone) for Biomedical Applications: From Enhancing Bioactivity to Reinforced-Bioactive Composites—An Overview" Polymers 15, no. 2: 373. https://doi.org/10.3390/polym15020373
APA StyleSenra, M. R., Marques, M. d. F. V., & Monteiro, S. N. (2023). Poly (Ether-Ether-Ketone) for Biomedical Applications: From Enhancing Bioactivity to Reinforced-Bioactive Composites—An Overview. Polymers, 15(2), 373. https://doi.org/10.3390/polym15020373