Microscale Strategies for Generating Cell-Encapsulating Hydrogels
Abstract
:1. Introduction
2. Hydrogels for Cell Encapsulation
2.1. Hydrogel Crosslinking Strategies
2.2. Hydrogel Degradation
3. Microscale Technologies
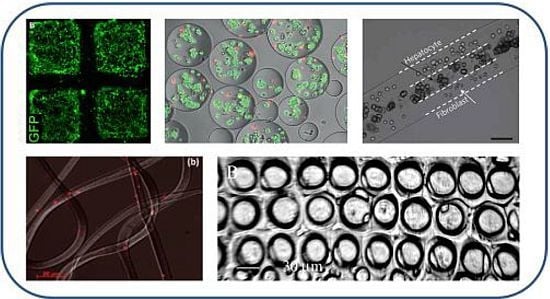
3.1. Soft Lithography

3.2. Photolithography
3.3. Microfluidics
3.3.1. Hydrodynamic Focusing


3.3.2. Jetting in a Coaxial Configuration

3.4. Extrusion of Gels for Cell Encapsulation
3.4.1. Electrospraying and Spinning

3.4.2. Bioprinting
4. Conclusions and Outlook
Acknowledgments
References
- Bonassar, L.J.; Vacanti, C.A. Tissue engineering: The first decade and beyond. J. Cell. Biochem. 1998, 30–31, 297–303. [Google Scholar] [CrossRef]
- Nichol, J.; Khademhosseini, A. Modular tissue engineering: Engineering biological tissues from the bottom up. Soft Matter 2009, 5, 1312–1319. [Google Scholar] [CrossRef]
- Khademhosseini, A.; Langer, R.; Borenstein, J.; Vacanti, J.P. Microscale technologies for tissue engineering and biology. Proc. Natl. Acad. Sci. USA 2006, 103, 2480–2487. [Google Scholar]
- Khademhosseini, A.; Vacanti, J.; Langer, R. Tissue engineering: Next generation tissue constructs and challenges to clinical practice. Sci. Am. 2009, 300, 64–71. [Google Scholar] [CrossRef]
- Brandl, F.; Sommer, F.; Goepferich, A. Rational design of hydrogels for tissue engineering: Impact of physical factors on cell behavior. Biomaterials 2007, 28, 134–146. [Google Scholar] [CrossRef]
- Inamdar, N.K.; Borenstein, J.T. Microfluidic cell culture models for tissue engineering. Curr. Opin. Biotechnol. 2011, 22, 1–9. [Google Scholar] [CrossRef]
- Kaji, H.; Camci-Unal, G.; Langer, R.; Khademhosseini, A. Engineering systems for the generation of patterned co-cultures for controlling cell-cell interactions. Biochim. Biophys. Acta 2011, 1810, 239–250. [Google Scholar] [CrossRef]
- Park, H.; Cannizzaro, C.; Vunjak-Novakovic, G.; Langer, R.; Vacanti, C.A.; Farokhzad, O.C. Nanofabrication and microfabrication of functional materials for tissue engineering. Tissue Eng. 2007, 13, 1867–1877. [Google Scholar] [CrossRef]
- Brouzesa, E.; Medkova, M.; Savenelli, N.; Marran, D.; Twardowski, M.; Hutchison, J.B.; Rothberg, J.M.; Link, D.R.; Perrimon, N.; Samuels, M.L. Droplet microfluidic technology for single-cell highthroughput screening. Proc. Natl. Acad. Sci. USA. 2009, 106, 14195–14200. [Google Scholar]
- Clausell-Tormos, J.; Lieber, D.; Baret, J.C.; El-Harrak, A.; Miller, O.J.; Frenz, L.; Blouwolff, J.; Humphry, K.J.; Köster, S.; Duan, H.; Holtze, C.; Weitz, D.A.; Griffiths, A.D.; Merten, C.A. Droplet-based microfluidic platforms for the encapsulation and screening of mammalian cells and multicellular organisms. Chem. Biol. 2008, 15, 427–437. [Google Scholar] [CrossRef]
- Jayasinghe, S.N.; Irvine, S.; McEwan, J.R. Cell electrospinning highly concentrated cellular suspensions containing primary living organisms into cell-bearing threads and scaffolds. Nanomedicine 2007, 2, 555–567. [Google Scholar] [CrossRef]
- Townsend-Nicholson, A.; Jayasinghe, S.N. Cell electrospinning: A unique biotechnique for encapsulating living organisms for generating active biological microthreads/scaffolds. Biomacromolecules 2006, 7, 3364–3369. [Google Scholar] [CrossRef]
- Sant, S.; Hwang, C.; Lee, S.; Khademhosseini, A. Hybrid PGS-PCL microfibrous scaffolds with improved mechanical and biological properties. J. Tissue Eng. Regen. Med. 2011, 5, 283–291. [Google Scholar] [CrossRef]
- Abeyewickreme, A.; Kwok, A.; McEwan, J.R.; Jayasinghe, S.N. Bio-electrospraying embryonic stem cells: Interrogating cellular viability and pluripotency. Integr. Biol. 2009, 1, 160–166. [Google Scholar]
- Liu, V.A.; Bhatia, S.N. Three-Dimensional Photopatterning of Hydrogels Containing Living Cells. Biomed. Microdevices 2002, 4, 257–266. [Google Scholar] [CrossRef]
- Kim, Y.S.; Suh, K.Y.; Lee, H.H. Fabrication of three-dimensional microstructures by soft molding. Appl. Phys. Lett. 2001, 79, 2285–2287. [Google Scholar] [CrossRef]
- Whitesides, G.M.; Ostuni, E.; Takayama, S.; Jiang, X.; Ingber, D. Soft lithography in biology and biochemistry. Annu. Rev. Biomed. Eng. 2001, 3, 335–373. [Google Scholar] [CrossRef]
- Nichol, J.W.; Koshy, S.T.; Bae, H.; Hwang, C.M.; Yamanlar, S.; Khademhosseini, A. Cell-laden microengineered gelatin methacrylate hydrogels. Biomaterials 2010, 31, 5536–5544. [Google Scholar] [CrossRef]
- Tekin, H.; Anaya, M.; Brigham, M.D.; Naumann, C.; Langer, R.; Khademhosseini, A. Stimuli-responsive microwells for formation and retrieval of cell aggregates. Lab Chip 2010, 10, 2411–2418. [Google Scholar] [CrossRef]
- Mironov, V.; Reis, N.; Derby, B. Bioprinting: A Beginning. Tissue Eng. 2006, 12, 632–634. [Google Scholar]
- Mironov, V.; Prestwich, G.; Forgacs, G. Bioprinting living structures. J. Mater. Chem. 2007, 17, 2054–2060. [Google Scholar] [CrossRef]
- Jakab, K.; Damon, B.; Neagu, A.; Kachurin, A.; Forgacs, G. Three-dimensional tissue constructs built by bioprinting. Biorheology 2006, 43, 509–513. [Google Scholar]
- Karoly, J.; Cyrille, N.; Francoise, M.; Keith, M.; Gordana, V.-N.; Gabor, F. Tissue engineering by self-assembly and bio-printing of living cells. Biofabrication 2010, 2, 022001. [Google Scholar] [CrossRef]
- Yanagawa, F.; Kaji, H.; Jang, Y.-H.; Bae, H.; Du, Y.; Fukuda, J.; Qi, H.; Khademhosseini, A. Directed assembly of cell-laden microgels for building porous three-dimensional tissue constructs. J. Biomed. Mater. Res. A 2011, 97, 93–102. [Google Scholar]
- Maquet, V.; Martin, D.; Scholtes, F.; Franzen, R.; Schoenen, J.; Moonen, G.; Jerome, R. Poly(d,l-lactide) foams modified by poly(ethylene oxide)-block-poly(d,l-lactide) copolymers and a-FGF: In vitro and in vivo evaluation for spinal cord regeneration. Biomaterials 2001, 22, 1137–1146. [Google Scholar] [CrossRef]
- Ambre, A.H.; Katti, K.S.; Katti, D.R. Nanoclay based composite scaffolds for bone tissue engineering applications. J. Nanotechnol. Eng. Med. 2010, 1, 031013:1–031013:9. [Google Scholar]
- Khademhosseini, A.; Eng, G.; Yeh, J.; Fukuda, J.; Blumling, J.; Langer, R.; Burdick, J.A. Micromolding of photocrosslinkable hyaluronic acid for cell encapsulation and entrapment. J. Biomed. Mater. Res. A 2006, 79, 522–532. [Google Scholar]
- Xiao, W.; He, J.; Nichol, J.W.; Wang, L.; Hutson, C.B.; Wang, B.; Du, Y.; Fan, H.; Khademhosseini, A. Synthesis and characterization of photocrosslinkable gelatin and silk fibroin interpenetrating polymer network hydrogels. Acta Biomater. 2011, 7, 2384–2393. [Google Scholar] [CrossRef]
- Jeon, O.; Bouhadir, K.H.; Mansour, J.M.; Alsberg, E. Photocrosslinked alginate hydrogels with tunable biodegradation rates and mechanical properties. Biomaterials 2009, 30, 2724–2734. [Google Scholar] [CrossRef]
- Ifkovits, J.L.; Burdick, J.A. Review: Photopolymerizable and degradable biomaterials for tissue engineering applications. Tissue Eng. 2007, 13, 2369–2385. [Google Scholar] [CrossRef]
- Hutson, C.B.; Nichol, J.W.; Aubin, H.; Bae, H.; Yamanlar, S.; Al-Haque, S.; Koshy, S.T.; Khademhosseini, A. Synthesis and characterization of tunable poly(ethylene glycol): Gelatin methacrylate composite hydrogels. Tissue Eng. A 2011, 17, 1713–1723. [Google Scholar] [CrossRef]
- Cruise, G.M.; Scharp, D.S.; Hubbell, J.A. Characterization of permeability and network structure of interfacially photopolymerized poly(ethylene glycol) diacrylate hydrogels. Biomaterials 1998, 19, 1287–1294. [Google Scholar] [CrossRef]
- Chan-Park, M.B.; Yan, Y.; Neo, W.K.; Zhou, W.; Zhang, J.; Yue, C.Y. Fabrication of high aspect ratio poly(ethylene glycol)-containing microstructures by UV embossing. Langmuir 2003, 19, 4371–4380. [Google Scholar] [CrossRef]
- Revzin, A.; Tompkins, R.G.; Toner, M. Surface engineering with poly(ethylene glycol) photolithography to create high-density cell arrays on glass. Langmuir 2003, 19, 9855–9862. [Google Scholar]
- Khademhosseini, A.; Yeh, J.; Jon, S.; Eng, G.; Suh, K.Y.; Burdick, J.A.; Langer, R. Molded polyethylene glycol microstructures for capturing cells within microfluidic channels. Lab Chip 2004, 4, 425–430. [Google Scholar] [CrossRef]
- Bahney, C.S.; Lujan, T.J.; Hsu, C.W.; Bottlang, M.; West, J.L.; Johnstone, B. Visible light photoinitiation of mesenchymal stem cell-laden bioresponsive hydrogels. Eur. Cells Mater. 2011, 22, 43–55. [Google Scholar]
- Nguyen, K.T.; West, J.L. Photopolymerizable hydrogels for tissue engineering applications. Biomaterials 2002, 23, 4307–4314. [Google Scholar] [CrossRef]
- Dare, E.V.; Griffith, M.; Poitras, P.; Kaupp, J.A.; Waldman, S.D.; Carlsson, D.J.; Dervin, G.; Mayoux, C.; Hincke, M.T. Genipin cross-linked fibrin hydrogels for in vitro human articular cartilage tissue-engineered regeneration. Cells Tissues Organs 2009, 190, 313–325. [Google Scholar] [CrossRef]
- Bigi, A.; Cojazzi, G.; Panzavolta, S.; Roveri, N.; Rubini, K. Stabilization of gelatin films by crosslinking with genipin. Biomaterials 2002, 23, 4827–4832. [Google Scholar] [CrossRef]
- Thalmann, C.; Lötzbeyer, T. Enzymatic cross-linking of proteins with tyrosinase. Eur. Food Res. Technol. 2002, 214, 276–281. [Google Scholar] [CrossRef]
- Sanborn, T.J.; Messersmith, P.B.; Barron, A.E. In situ crosslinking of a biomimetic peptide-PEG hydrogel via thermally triggered activation of factor XIII. Biomaterials 2002, 23, 2703–2710. [Google Scholar] [CrossRef]
- Davis, N.E.; Ding, S.; Forster, R.E.; Pinkas, D.M.; Barron, A.E. Modular enzymatically crosslinked protein polymer hydrogels for in situ gelation. Biomaterials 2010, 31, 7288–7297. [Google Scholar] [CrossRef]
- Kuo, C.K.; Ma, P.X. Ionically crosslinked alginate hydrogels as scaffolds for tissue engineering: Part 1. Structure, gelation rate and mechanical properties. Biomaterials 2001, 22, 511–521. [Google Scholar] [CrossRef]
- Hennink, W.E.; van Nostrum, C.F. Novel crosslinking methods to design hydrogels. Adv. Drug Deliv. Rev. 2002, 54, 13–36. [Google Scholar] [CrossRef]
- Gohil, J.; Bhattacharya, A.; Ray, P. Studies on the crosslinking of poly (vinyl alcohol). J. Polym. Res. 2006, 13, 161–169. [Google Scholar] [CrossRef]
- Maolin, Z.; Ning, L.; Jun, L.; Min, Y.; Jiuqiang, L.; Hongfei, H. Radiation preparation of PVA-g-NIPAAm in a homogeneous system and its application in controlled release. Radiat. Phys. Chem. 2000, 57, 481–484. [Google Scholar]
- Li, S.; Molina, I.; Martinez, M.B.; Vert, M. Hydrolytic and enzymatic degradations of physically crosslinked hydrogels prepared from PLA/PEO/PLA triblock copolymers. J. Mater. Sci. Mater. Med. 2002, 13, 81–86. [Google Scholar] [CrossRef]
- Levesque, S.G.; Shoichet, M.S. Synthesis of enzyme-degradable, peptide-cross-linked dextran hydrogels. Bioconjug. Chem. 2007, 18, 874–885. [Google Scholar] [CrossRef]
- Lee, K.Y.; Bouhadir, K.H.; Mooney, D.J. Controlled degradation of hydrogels using multi-functional cross-linking molecules. Biomaterials 2004, 25, 2461–2466. [Google Scholar] [CrossRef]
- Cha, C.; Kohman, R.H.; Kong, H. Biodegradable polymer crosslinker: Independent control of stiffness, toughness, and hydrogel degradation rate. Adv. Funct. Mater. 2009, 19, 3056–3062. [Google Scholar] [CrossRef]
- Bastioli, C. Handbook of Biodegradable Polymers; Rapra Technology Limited: Shawbury, UK, 2005. [Google Scholar]
- Nicodemus, G.D.; Bryant, S.J. Cell encapsulation in biodegradable hydrogels for tissue engineering applications. Tissue Eng. B Rev. 2008, 14, 149–165. [Google Scholar] [CrossRef]
- Wu, D.-Q.; Sun, Y.-X.; Xu, X.-D.; Cheng, S.-X.; Zhang, X.-Z.; Zhuo, R.-X. Biodegradable and pH-sensitive hydrogels for cell encapsulation and controlled drug release. Biomacromolecules 2008, 9, 1155–1162. [Google Scholar] [CrossRef]
- Ishihara, M.; Obara, K.; Ishizuka, T.; Fujita, M.; Sato, M.; Masuoka, K.; Saito, Y.; Yura, H.; Matsui, T.; Hattori, H.; Kikuchi, M.; Kurita, A. Controlled release of fibroblast growth factors and heparin from photocrosslinked chitosan hydrogels and subsequent effect on in vivo vascularization. J. Biomed. Mater. Res. A 2003, 64A, 551–559. [Google Scholar] [CrossRef]
- Slaughter, B.V.; Khurshid, S.S.; Fisher, O.Z.; Khademhosseini, A.; Peppas, N.A. Hydrogels in regenerative medicine. Adv. Mater. 2009, 21, 3307–3329. [Google Scholar] [CrossRef]
- Verma, S.; Garkhal, K.; Mittal, A.; Kumar, N. Biodegradable polymers for emerging clinical use in tissue engineering. In Biodegradable Polymers in Clinical Use and Clinical Development; Domb, A.J., Kumar, N., Ezra, A., Eds.; John Wiley & Sons, Inc.: Hoboken, NJ, USA, 2011; pp. 565–629. [Google Scholar]
- Mufamadi, M.S.; Pillay, V.; Choonara, Y.E.; du Toit, L.C.; Modi, G.; Naidoo, D.; Ndesendo, V.M.K. A review on composite liposomal technologies for specialized drug delivery. J. Drug Deliv. 2011, 2011, 939851:1–939851:19. [Google Scholar]
- Vorhies, J.S.; Nemunaitis, J.J. Synthetic vs. natural/biodegradable polymers for delivery of shrna-based cancer therapies. Methods Mol. Biol. 2008, 480, 11–29. [Google Scholar]
- Nuttelman, C.R.; Henry, S.M.; Anseth, K.S. Synthesis and characterization of photocrosslinkable, degradable poly(vinyl alcohol)-based tissue engineering scaffolds. Biomaterials 2002, 23, 3617–3626. [Google Scholar] [CrossRef]
- Lutolf, M.P.; Raeber, G.P.; Zisch, A.H.; Tirelli, N.; Hubbell, J.A. Cell-responsive synthetic hydrogels. Adv. Mater. 2003, 15, 888–892. [Google Scholar] [CrossRef]
- Schmedlen, R.H.; Masters, K.S.; West, J.L. Photocrosslinkable polyvinyl alcohol hydrogels that can be modified with cell adhesion peptides for use in tissue engineering. Biomaterials 2002, 23, 4325–4332. [Google Scholar] [CrossRef]
- Xia, Y.; Whitesides, G.M. Soft Lithography. Angew. Chem. Int. Ed. 1998, 37, 550–575. [Google Scholar] [CrossRef]
- Xia, Y.; McClelland, J.J.; Gupta, R.; Qin, D.; Zhao, X.-M.; Sohn, L.L.; Celotta, R.J.; Whitesides, G.M. Replica molding using polymeric materials: A practical step toward nanomanufacturing. Adv. Mater. 1997, 9, 147–149. [Google Scholar] [CrossRef]
- Zhang, Y.; Lo, C.-W.; Taylor, J.A.; Yang, S. Replica molding of high-aspect-ratio polymeric nanopillar arrays with high fidelity. Langmuir 2006, 22, 8595–8601. [Google Scholar] [CrossRef]
- Teruo, F. PDMS-based microfluidic devices for biomedical applications. Microelectron. Eng. 2002, 61–62, 907–914. [Google Scholar] [CrossRef]
- Regehr, K.J.; Domenech, M.; Koepsel, J.T.; Carver, K.C.; Ellison-Zelski, S.J.; Murphy, W.L.; Schuler, L.A.; Alarid, E.T.; Beebe, D.J. Biological implications of polydimethylsiloxane-based microfluidic cell culture. Lab Chip 2009, 9, 2132–2139. [Google Scholar] [CrossRef]
- Moeller, H.-C.; Mian, M.K.; Shrivastava, S.; Chung, B.; Khademhosseini, A. A microwell array system for stem cell culture. Biomaterials 2008, 29, 752–763. [Google Scholar] [CrossRef]
- Zhao, X.-M.; Xia, Y.; Whitesides, G.M. Fabrication of three-dimensional micro-structures: Microtransfer molding. Adv. Mater. 1996, 8, 837–840. [Google Scholar] [CrossRef]
- Tekin, H.; Tsinman, T.; Sanchez, J.G.; Jones, B.J.; Camci-Unal, G.; Nichol, J.W.; Langer, R.; Khademhosseini, A. Responsive micromolds for sequential patterning of hydrogel microstructures. J. Am. Chem. Soc. 2011, 133, 12944–12947. [Google Scholar]
- Tekin, H.; Sanchez, J.G.; Tsinman, T.; Langer, R.; Khademhosseini, A. Thermoresponsive platforms for tissue engineering and regenerative medicine. AIChE J. 2011, 57, 3249–3258. [Google Scholar] [CrossRef]
- Chu, M.K.L.; Chen, J.; Gordijo, C.R.; Chiang, S.; Ivovic, A.; Koulajian, K.; Giacca, A.; Wu, X.Y.; Sun, Y. In vitro and in vivo testing of glucose-responsive insulin-delivery microdevices in diabetic rats. Lab Chip 2012, 12, 2533–2539. [Google Scholar] [CrossRef]
- Kim, E.; Xia, Y.; Whitesides, G.M. Micromolding in capillaries: Applications in materials science. J. Am. Chem. Soc. 1996, 118, 5722–5731. [Google Scholar]
- Blümel, A.; Klug, A.; Eder, S.; Scherf, U.; Moderegger, E.; List, E.J.W. Micromolding in capillaries and microtransfer printing of silver nanoparticles as soft-lithographic approach for the fabrication of source/drain electrodes in organic field-effect transistors. Org. Electron. 2007, 8, 389–395. [Google Scholar] [CrossRef]
- Zhao, X.-M.; Stoddart, A.; Smith, S.P.; Kim, E.; Xia, Y.; Prentiss, M.; Whitesides, G.M. Fabrication of single-mode polymeric waveguides using micromolding in capillaries. Adv. Mater. 1996, 8, 420–424. [Google Scholar] [CrossRef]
- Delamarche, E.; Bernard, A.; Schmid, H.; Michel, B.; Biebuyck, H. Patterned delivery of immunoglobulins to surfaces using microfluidic networks. Science 1997, 276, 779–781. [Google Scholar] [CrossRef]
- Ling, Y.; Rubin, J.; Deng, Y.; Huang, C.; Demirci, U.; Karp, J.M.; Khademhosseini, A. A cell-laden microfluidic hydrogel. Lab Chip 2007, 7, 756–762. [Google Scholar] [CrossRef]
- Du, Y.; Ghodousi, M.; Lo, E.; Vidula, M.K.; Emiroglu, O.; Khademhosseini, A. Surface-directed assembly of cell-laden microgels. Biotechnol. Bioeng. 2009, 105, 655–662. [Google Scholar]
- Fisher, J.P.; Dean, D.; Engel, P.S.; Mikos, A.G. Photoinitiated polymerization of biomaterials. Mater. Res. 2001, 31, 171–181. [Google Scholar] [CrossRef]
- Yang, S.; Ford, J.; Ruengruglikit, C.; Huang, Q.; Aizenberg, J. Synthesis of photoacid crosslinkable hydrogels for the fabrication of soft, biomimetic microlens arrays. J. Mater. Chem. 2005, 15, 4200–4202. [Google Scholar] [CrossRef]
- Maldovan, M.; Thomas, E.L. Periodic Materials and Interference Lithography; Wiley: Weinheim, Germany, 2009. [Google Scholar]
- Lin, C.-C.; Raza, A.; Shih, H. PEG hydrogels formed by thiol-ene photo-click chemistry and their effect on the formation and recovery of insulin-secreting cell spheroids. Biomaterials 2011, 32, 9685–9695. [Google Scholar] [CrossRef]
- Albrecht, D.R.; Tsang, V.L.; Sah, R.L.; Bhatia, S.N. Photo- and electropatterning of hydrogel-encapsulated living cell arrays. Lab Chip 2005, 5, 111–118. [Google Scholar] [CrossRef]
- Bencherif, S.A.; Siegwart, D.J.; Srinivasan, A.; Horkay, F.; Hollinger, J.O.; Washburn, N.R.; Matyjaszewski, K. Nanostructured hybrid hydrogels prepared by a combination of atom transfer radical polymerizaiton and free radical polymerization. Biomaterials 2009, 30, 5270–5278. [Google Scholar]
- Park, Y.D.; Tirelli, N.; Hubbell, J.A. Photopolymerized hyaluronic acid-based hydrogels and interpenetrating networks. Biomaterials 2003, 24, 893–900. [Google Scholar] [CrossRef]
- Ng, L.-T.; Jönsson, S.; Swami, S.; Lindgren, K. Synthesis of hydrogel for drug delivery studies utilizing photoinitiator-free photopolymerization based on the donor/acceptor pair, N-vinylpyrrolidinone and hydroxypentyl maleimide. Polym. Int. 2002, 51, 1398–1403. [Google Scholar] [CrossRef]
- Dendukuri, D.; Gu, S.S.; Pregibon, D.C.; Hatton, T.A.; Doyle, P.S. Stop-flow lithography in a microfluidic device. Lab Chip 2007, 7, 818–828. [Google Scholar] [CrossRef]
- Kasko, A.M.; Wong, D.Y. Two-photon lithography in the future of cell-based therapeutics and regenerative medicine: A review of techniques for hydrogel patterning and controlled release. Future Med. Chem. 2010, 2, 1669–1680. [Google Scholar] [CrossRef]
- Jeon, S.; Malyarchuk, V.; Rogers, J.A.; Wiederrecht, G.P. Fabricating three dimensional nanostructures using two photon lithography in a single exposure step. Opt. Express 2006, 14, 2300–2308. [Google Scholar] [CrossRef]
- Lee, S.-H.; Moon, J.J.; West, J.L. Three-dimensional micropatterning of bioactive hydrogels via two-photon laser scanning photolithography for guided 3D cell migration. Biomaterials 2008, 29, 2962–2968. [Google Scholar]
- Squires, T.; Quake, S. Microfluidics: Fluid physics at the nanoliter scale. Rev. Mod. Phys. 2005, 77, 977–1026. [Google Scholar] [CrossRef]
- Whitesides, G.M. The origins and the future of microfluidics. Nature 2006, 442, 368–373. [Google Scholar] [CrossRef]
- Flaim, C.J.; Chien, S.; Bhatia, S.N. An extracellular matrix microarray for probing cellular differentiation. Nat. Methods 2005, 2, 119–125. [Google Scholar] [CrossRef]
- Anderson, D.G.; Levenberg, S.; Langer, R. Nanoliter-scale synthesis of arrayed biomaterials and application to human embryonic stem cells. Nat. biotechnol. 2004, 22, 863–866. [Google Scholar] [CrossRef]
- Young, E.W.; Beebe, D.J. Fundamentals of microfluidic cell culture in controlled microenvironments. Chem. Soc. Rev. 2010, 39, 1036–1048. [Google Scholar]
- Lim, J.Y.; Kim, W.H.; Kim, J.; Park, S.I. Involvement of TGF-beta1 signaling in cardiomyocyte differentiation from P19CL6 cells. Mol. cells 2007, 24, 431–436. [Google Scholar]
- Atencia, J.; Beebe, D.J. Controlled microfluidic interfaces. Nature 2005, 437, 648–655. [Google Scholar] [CrossRef]
- Whitesides, G.M.; Stroock, A.D. Flexible methods for mircofluidics. Phys. Today 2001, 54, 42–48. [Google Scholar] [CrossRef]
- Wu, M.-H.; Huang, S.-B.; Lee, G.-B. Microfluidic cell culture systems for drug research. Lab Chip 2010, 10, 939–956. [Google Scholar] [CrossRef]
- Dittrich, P.S.; Manz, A. Lab-on-a-chip: microfluidics in drug discovery. Nat. Rev. Drug Discov. 2006, 5, 210–218. [Google Scholar] [CrossRef]
- Yeo, L.Y.; Chang, H.-C.; Chan, P.P.Y.; Friend, J.R. Microfluidic devices for bioapplications. Small 2011, 7, 12–48. [Google Scholar] [CrossRef]
- Gupta, K.; Kim, D.-H.; Ellison, D.; Smith, C.; Kundu, A.; Tuan, J.; Suh, K.-Y.; Levchenko, A. Lab-on-a-chip devices as an emerging platform for stem cell biology. Lab Chip 2010, 10, 2019–2031. [Google Scholar] [CrossRef]
- Van Noort, D.; Ong, S.M.; Zhang, C.; Zhang, S.; Arooz, T.; Yu, H. Stem cells in microfluidics. Biotechnol. Progr. 2009, 25, 52–60. [Google Scholar] [CrossRef]
- Wlodkowic, D.; Cooper, J.M. Tumors on chips: Oncology meets microfluidics. Curr. Opin. Chem. Biol. 2010, 14, 556–567. [Google Scholar] [CrossRef]
- Chung, S.; Sudo, R.; Vickerman, V.; Zervantonakis, I.K.; Kamm, R.D. Microfluidic platforms for studies of angiogenesis, cell migration, and cell–cell interactions. Annu. Biomed. Eng. 2010, 38, 1164–1177. [Google Scholar] [CrossRef]
- Zervantonakis, I.K.; Kothapalli, C.R.; Chung, S.; Sudo, R.; Kamm, R.D. Microfluidic devices for studying heterotypic cell-cell interactions and tissue specimen cultures under controlled microenvironments. Biomicrofluidics 2011, 5, 013406. [Google Scholar] [CrossRef]
- Ahmed, T.; Shimizu, T.S.; Stocker, R. Microfluidics for bacterial chemotaxis. Integr. Biol. 2010, 2, 604–629. [Google Scholar] [CrossRef]
- Ziolkowska, K.; Kwapiszewski, R.; Brzozka, Z. Microfluidic devices as tools for mimicking the in vivo environment. New J. Chem. 2011, 35, 979–990. [Google Scholar] [CrossRef]
- Paguirigan, A.L.; Beebe, D.J. From the cellular perspective: Exploring differences in the cellular baseline in macroscale and microfluidic cultures. Integr. Biol. 2009, 1, 182–195. [Google Scholar] [CrossRef]
- Meyvantsson, I.; Beebe, D.J. Cell culture models in microfluidic systems. Annu. Rev. Anal. Chem. 2008, 1, 423–449. [Google Scholar] [CrossRef]
- Le Gac, S.; van den Berg, A. Single cells as experimentation units in lab-on-a-chip devices. Trends Biotechnol. 2010, 28, 55–62. [Google Scholar] [CrossRef]
- Domansky, K.; Inman, W.; Serdy, J.; Dash, A.; Lim, M.H.M.; Griffith, L.G. Perfused multiwell plate for 3D liver tissue engineering. Lab Chip 2010, 10, 51–58. [Google Scholar] [CrossRef]
- Sim, W.Y.; Park, S.-W.; Park, S.H.; Min, B.H.; Park, S.R.; Yang, S.S. A pneumatic micro cell chip for the differentiation of human mesenchymal stem cells under mechanical stimulation. Lab Chip 2007, 7, 1775–1782. [Google Scholar] [CrossRef]
- Capron, I.; Costeux, S.; Djabourov, M. Water in water emulsions: Phase separation and rheology of biopolymer solutions. Rheol. Acta 2001, 40, 441–456. [Google Scholar] [CrossRef]
- Stenekes, R.J.H.; Franssen, O.; Bommel, E.M.G.v.; Crommelin, D.J.A.; Hennink, W.E. The use of aqueous PEG/dextran phase separation for the preparation of dextran microspheres. Int. J. Pharm. 1999, 183, 29–32. [Google Scholar] [CrossRef]
- Yasukawa, M.; Kamio, E.; Ono, T. Monodisperse water-in-water-in-oil emulsion droplets. ChemPhysChem. 2011, 12, 263–266. [Google Scholar] [CrossRef]
- Shintaku, H.; Kuwabara, T.; Kawano, S.; Suzuki, T.; Kanno, I.; Kotera, H. Micro cell encapsulation and its hydrogel-beads production using microfluidic device. Microsyst. Technol. 2007, 13, 951–958. [Google Scholar] [CrossRef]
- Haeberle, S.; Naegele, L.; Burger, R.; Stetten, F.V.; Zengerle, R.; Ducre'e, J. Alginate bead fabrication and encapsulation of living cells under centrifugally induced artificial gravity conditions. J. Microencapsul. 2008, 25, 267–274. [Google Scholar] [CrossRef]
- Nisisako, T.; Torii, T.; Takahashi, T.; Takizawa, Y. Synthesis of monodisperse bicolored janus particles with electrical anisotropy using a microfluidic co-flow system. Adv. Mater. 2006, 18, 1152–1156. [Google Scholar] [CrossRef]
- Prasad, N.; Perumal, J.; Choi, C.-H.; Lee, C.-S.; Kim, D.-P. Generation of monodisperse inorganic-organic janus microspheres in a microfluidic device. Adv. Funct. Mater. 2009, 19, 1656–1662. [Google Scholar]
- Seiffert, S. Functional microgels tailored by droplet-based microfluidics. Macromol. Rapid Commun. 2011, 32, 1600–1609. [Google Scholar] [CrossRef]
- Seiffert, S.; Romanowsky, M.B.; Weitz, D.A. Janus microgels produced from functional precursor polymers. Langmuir 2010, 26, 14842–14847. [Google Scholar]
- Abate, A.R.; Kutsovsky, M.; Seiffert, S.; Windbergs, M.; Pinto, L.F.V.; Rotem, A.; Utada, A.S.; Weitz, D.A. Synthesis of monodisperse microparticles from non-newtonian polymer solutions with microfluidic devices. Adv. Mater. 2011, 23, 1757–1760. [Google Scholar]
- Chen, C.-H.; Abate, A.R.; Lee, D.; Terentjev, E.M.; Weitz, D.A. Microfluidic assembly of magnetic hydrogel particles with uniformly anisotropic structure. Adv. Mater. 2009, 21, 3201–3204. [Google Scholar]
- Utada, A.S.; Chu, L.-Y.; Fernandez-Nieves, A.; Link, D.R.; Holtze, C.; Weitz, D.A. Dripping, jetting, drops, and wetting: The magic of microfluidics. MRS Bull. 2007, 32, 702–708. [Google Scholar] [CrossRef]
- Chu, L.-Y.; Utada, A.S.; Shah, R.K.; Kim, J.-W.; Weitz, D.A. Controllable monodisperse multiple emulsions. Angew. Chem. Int. Ed. 2007, 46, 8970–8974. [Google Scholar]
- Lee, K.G.; Park, T.J.; Soo, S.Y.; Wang, K.W.; Kim, B.I.; Park, J.H.; Lee, C.-S.; Kim, D.H.; Lee, S.J. Synthesis and utilization of E. coli-encapsulated PEG-based microdroplet using a microfluidic chip for biological application. Biotechnol. Bioeng. 2010, 107, 747–751. [Google Scholar] [CrossRef]
- Franco, C.L.; Price, J.; West, J.L. Development and optimization of a dual-photoinitiator, emulsion-based technique for rapid generation of cell-laden hydrogel microspheres. Acta Biomater. 2011, 7, 3267–3276. [Google Scholar] [CrossRef]
- Koh, W.-G.; Pishko, M.V. Fabrication of cell-containing hydrogel microstructures inside microfluidic devices that can be used as cell-based biosensors. Anal. Bioanal. Chem. 2006, 385, 1389–1397. [Google Scholar] [CrossRef]
- Tan, W.-H.; Takeuchi, S. Monodisperse alginate hydrogel microbeads for cell encapsulation. Adv. Mater. 2007, 19, 2696–2701. [Google Scholar] [CrossRef]
- Vijayakumar, K.; Gulati, S.; deMello, A.J.; Edel, J.B. Rapid cell extraction in aqueous two-phase microdroplet systems. Chem. Sci. 2010, 1, 447–452. [Google Scholar] [CrossRef]
- Um, E.; Lee, D.-S.; Pyo, H.-B.; Park, J.-K. Continuous generation of hydrogel beads and encapsulation of biological materials using a microfluidic droplet-merging channel. Microfluid. Nanofluid. 2008, 5, 541–549. [Google Scholar] [CrossRef]
- Tsuda, Y.; Morimoto, Y.; Takeuchi, S. Monodisperse cell-encapsulating peptide microgel beads for 3D cell culture. Langmuir 2010, 26, 2645–2649. [Google Scholar]
- Cordero, M.L.; Gallaire, F.; Baroud, C.N. Quantitative analysis of the dripping and jetting regimes in co-fowing capillary jets. Phys. Fluids 2011, 23, 094111. [Google Scholar] [CrossRef] [Green Version]
- Steinbacher, J.L.; McQuade, D.T. Polymer chemistry in flow: New polymers, beads, capsules, and fibers. J. Polym. Chem. A 2006, 44, 6505–6533. [Google Scholar] [CrossRef]
- Hu, M.; Deng, R.; Schumacher, K.M.; Kurisawa, m.; Ye, H.; Purnamawati, K.; Ying, J.Y. Hydrodynamic spinning of hydrogel fibers. Biomaterials 2009, 31, 863–869. [Google Scholar]
- Kang, E.; Jeong, G.S.; Choi, Y.Y.; Lee, K.H.; Khademhosseini, A.; Lee, S.-H. Digitally tunable physicochemical coding of material composition and topography in continuous microfibres. Nat. Mater. 2011, 10, 877–883. [Google Scholar]
- Yeh, C.-H.; Lin, P.-W.; Lin, Y.-C. Chitosan microfiber fabrication using a microfluidic chip and its application to cell cultures. Microfluid. Nanofluid. 2010, 8, 115–121. [Google Scholar] [CrossRef]
- Honda, T.; Miyazaki, M.; Nakamura, H.; Maeda, H. Controllable polymerization of N-carboxy anhydrides in a microreaction system. Lab Chip 2005, 5, 812–818. [Google Scholar] [CrossRef]
- Ramakrishna, S. An Introduction to Electrospinning and Nanofibers; World Scientific Publishing, SI: Singapore, 2005. [Google Scholar]
- Hong, J.; deMello, A.J.; Jayasinghe, S.N. Bio-electrospraying and droplet-based microfluidics: Control of cell numbers within living residues. Biomed. Mater. 2010, 5, 021001. [Google Scholar] [CrossRef]
- Ward, E.; Chan, E.; Gustafson, K.; Jayasinghe, S.N. Combining bio-electrospraying with gene therapy: A novel biotechnique for the delivery of genetic material via living cells. Analyst 2010, 135, 1042–1049. [Google Scholar] [CrossRef]
- Klein, S.; Kuhn, J.; Avrahami, R.; Tarre, S.; Beliavski, M.; Green, M.; Zussman, E. Encapsulation of bacterial cells in electrospun microtubes. Biomacromolecules 2009, 10, 1751–1756. [Google Scholar] [CrossRef]
- Boland, T.; Tao, X.; Damon, B.J.; Manley, B.; Kesari, P.; Jalota, S.; Bhaduri, S. Drop-on-demand printing of cells and materials for designer tissue constructs. Mater. Sci. Eng. C 2007, 27, 372–376. [Google Scholar] [CrossRef]
- Baudoin, R.; Corlu, A.; Griscom, L.; Legallais, C.; Leclerc, E. Trends in the development of microfluidic cell biochips for in vitro hepatotoxicity. Toxicol. In Vitro 2007, 21, 535–544. [Google Scholar] [CrossRef]
- Ghaemmaghami, A.M.; Hancock, M.J.; Harrington, H.; Kaji, H.; Khademhosseini, A. Biomimetic tissues on a chip for drug discovery. Drug Discov. Today 2011, 17, 173–181. [Google Scholar]
- Wang, X.; Yan, Y.; Zhang, R. Recent trends and challenges in complex organ manufacturing. Tissue Eng. B Rev. 2010, 16, 189–197. [Google Scholar] [CrossRef]
- Mironov, V.; Kasyanov, V.; Markwald, R.R. Organ printing: From bioprinter to organ biofabrication line. Curr. Opin. Biotechnol. 2011, 22, 667–673. [Google Scholar] [CrossRef]
- Skardal, A.; Zhang, J.; McCoard, L.; Xu, X.; Oottamasathien, S.; Prestwich, G.D. Photocrosslinkable hyaluronan-gelatin hydrogels for two-step bioprinting. Tissue Eng. A 2010, 16, 2675–2685. [Google Scholar] [CrossRef]
- Chaudhuri, J.; Al-Rubeai, M. Bioreactors for Tissue Engineering: Principles, Design and Operation; Springer: Dordrecht, The Netherlands, 2005. [Google Scholar]
- Norotte, C.; Marga, F.S.; Niklason, L.E.; Forgacs, G. Scaffold-free vascular tissue engineering using bioprinting. Biomaterials 2009, 30, 5910–5917. [Google Scholar] [CrossRef]
- Derby, B. Bioprinting: Inkjet printing proteins and hybrid cell-containing materials and structures. J. Mater. Chem. 2008, 18, 5717–5721. [Google Scholar] [CrossRef]
- Nakamura, M.; Kobayashi, A.; Takagi, F.; Watanabe, A.; Hiruma, Y.; Ohuchi, K.; Iwasaki, Y.; Horie, M.; Morita, I.; Takatani, S. Biocompatible inkjet printing technique for designed seeding of individual living cells. Tissue Eng. 2005, 11, 1658–1666. [Google Scholar] [CrossRef]
- Neagu, A.; Jakab, K.; Jamison, R.; Forgacs, G. Role of physical mechanisms in biological self-organization. Phys. Rev. Lett. 2005, 95, 178104:1–178104:4. [Google Scholar]
- Jakab, K.; Norotte, C.; Damon, B.; Marga, F.; Neagu, A.; Besch-Williford, C.L.; Kachurin, A.; Church, K.H.; Park, H.; Mironov, V.; Markwald, R.; Vunjak-Novakovic, G.; Forgacs, G. Tissue engineering by self-assembly of cells printed into topologically defined structures. Tissue Eng. A 2008, 14, 413–421. [Google Scholar] [CrossRef]
- Oberpenning, F.; Meng, J.; Yoo, J.J.; Atala, A. De novo reconstitution of a functional mammalian urinary bladder by tissue engineering. Nat. Biotechnol. 1999, 17, 149–155. [Google Scholar] [CrossRef]
- Lee, W.; Debasitis, J.C.; Lee, V.K.; Lee, J.-H.; Fischer, K.; Edminster, K.; Park, J.-K.; Yoo, S.-S. Multi-layered culture of human skin fibroblasts and keratinocytes through three-dimensional freeform fabrication. Biomaterials 2009, 30, 1587–1595. [Google Scholar] [CrossRef]
- Phillippi, J.A.; Miller, E.; Weiss, L.; Huard, J.; Waggoner, A.; Campbell, P. Microenvironments engineered by inkjet bioprinting spatially direct adult stem cells toward muscle- and bone-like subpopulations. Stem Cells 2008, 26, 127–134. [Google Scholar] [CrossRef]
- Cooper, G.M.; Miller, E.D.; DeCesare, G.E.; Usas, A.; Lensie, E.L.; Bykowski, M.R.; Huard, J.; Weiss, L.E.; Losee, J.E.; Campbell, P.G. Inkjet-based biopatterning of bone morphogenetic protein-2 to spatially control calvarial bone formation. Tissue Eng. A 2010, 16, 1749–1759. [Google Scholar] [CrossRef]
- Grosberg, A.; Alford, P.W.; McCain, M.L.; Parker, K.K. Ensembles of engineered cardiac tissues for physiological and pharmacological study: Heart on a chip. Lab Chip 2011, 11, 4165–4173. [Google Scholar] [CrossRef]
- Kniazeva, T.; Hsiao, J.C.; Charest, J.L.; Borenstein, J.T. A microfluidic respiratory assist device with high gas permeance for artificial lung applications. Biomed. Microdevices 2011, 13, 315–323. [Google Scholar] [CrossRef]
- Sung, J.H.; Yu, J.; Luo, D.; Shuler, M.L.; March, J.C. Microscale 3-D hydrogel scaffold for biomimetic gastrointestinal (GI) tract model. Lab Chip 2011, 11, 389–392. [Google Scholar] [CrossRef]
© 2012 by the authors; licensee MDPI, Basel, Switzerland. This article is an open-access article distributed under the terms and conditions of the Creative Commons Attribution license (http://creativecommons.org/licenses/by/3.0/).
Share and Cite
Selimović, Š.; Oh, J.; Bae, H.; Dokmeci, M.; Khademhosseini, A. Microscale Strategies for Generating Cell-Encapsulating Hydrogels. Polymers 2012, 4, 1554-1579. https://doi.org/10.3390/polym4031554
Selimović Š, Oh J, Bae H, Dokmeci M, Khademhosseini A. Microscale Strategies for Generating Cell-Encapsulating Hydrogels. Polymers. 2012; 4(3):1554-1579. https://doi.org/10.3390/polym4031554
Chicago/Turabian StyleSelimović, Šeila, Jonghyun Oh, Hojae Bae, Mehmet Dokmeci, and Ali Khademhosseini. 2012. "Microscale Strategies for Generating Cell-Encapsulating Hydrogels" Polymers 4, no. 3: 1554-1579. https://doi.org/10.3390/polym4031554
APA StyleSelimović, Š., Oh, J., Bae, H., Dokmeci, M., & Khademhosseini, A. (2012). Microscale Strategies for Generating Cell-Encapsulating Hydrogels. Polymers, 4(3), 1554-1579. https://doi.org/10.3390/polym4031554