Blockchain Paradigm for Healthcare: Performance Evaluation
Abstract
:1. Introduction
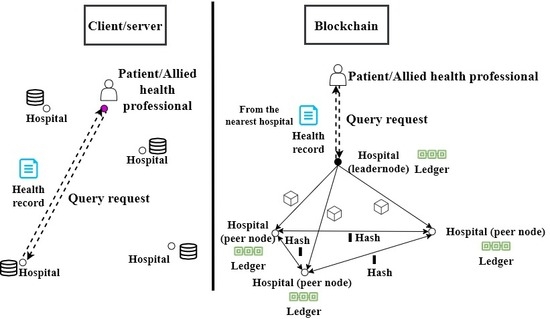
- While the blockchain characteristics are suitable for implementing a healthcare system, these mechanisms are still costly considering execution time and amount of data transferred for ledger update.
- In spite of these costly mechanisms, notable performance can be achieved thanks to the blockchain model, especially in a patient-centric approach. In this approach, the patients and/or the physicians are constantly visiting the health records to construct a cohesive view from different hospitals for a better diagnosis or prognosis of diseases using artificial intelligence.
2. Related Work
3. Blockchain Paradigm
- Infrastructure layer: It includes the network nodes (known as participants), network modules and storage provisions. There are three types of participants: (1) simple which only performs the transactions, (2) validating which performs and validates transactions, and has a copy of the ledger and (3) mining which generates a new block and has a copy of the ledger.
- Platform layer: It includes modules for communication between the blockchain participants.
- Computing layer: It includes the underlying blockchain mechanisms for immutability, availability, finality, provenance, privacy and security.
- Application layer: It enables the blockchain participants to communicate with the application.
3.1. Features of Blockchain
- Decentralization: A centralized third-party is not required as the ledger is updated after the majority of the participants in the network reaches a consensus.
- Immutability: A block in the ledger is hashed using its contents and the hash of the previous block. Consequently, any modification in a block will modify all the following blocks in the ledger. This makes the modification of a block in blockchain computationally difficult because the ledger is replicated among peers. In case data are entered by error, these data are corrected by issuing a new transaction.
- Transparency: Any change in the network is recorded as a transaction and can be viewed by all the participants maintaining a copy of the ledger.
- Traceability: The replication of any event in the network enables convenient tracing and audit trail.
- Trustless: Participants unknown to each other can perform transactions among each other as the consensus mechanism maintains the trust in the network.
3.2. Transaction Execution Mechanism
- Transaction proposal: The user hashes the transaction using a hashing algorithm. The user’s private key is then used to encrypt this hashed value. The result is known as the digital signature. The digital signature along with the data is broadcasted to the network.
- Transaction validation: The transaction is validated by each validating node. This is by authenticating the user identity and ensuring the data integrity. The identity is authenticated by decrypting the signature and the integrity is ensured by hashing the transaction and comparing it with the decrypted result. The valid transaction is sent to the mining node.
- Block generation: The mining node (selected based on the consensus protocol used) verifies the valid transactions and groups them in a block in a way that the block size does not exceed a predetermined threshold. It hashes the transactions data, block version, timestamp and previous block’s hash value, and then hashes this hash value to obtain the hash of the block. The miner broadcasts the block to the network.
- Replication: The validating and mining nodes verify the validity of the block as part of the consensus protocol. Once valid, each node updates its copy of the ledger by appending the block.
3.3. Benefits to Healthcare
- Fault tolerance: In a client/server-based system the patients’ health data are managed in a centralized database. Once the data are lost, they cannot be recovered. The replication characteristic of blockchain aids in fault tolerance.
- Data sharing: In the current client/server systems, a patient’s data are scattered over multiple hospitals’ databases. The sharing of data among different hospitals and medical organizations is a complex process. However, in a blockchain-based platform, the patients’ data recorded in the ledger is replicated among all the hospitals in the network.
- Interoperability: In a client/server-based system, each hospital stores the patients’ data in a different database using heterogeneous data formats and structures resulting in interoperability challenges. The synchronized and replicated ledger in the blockchain solves this issue.
- Avoidance of tests repetition: Currently the patients’ data are scattered across different healthcare providers, a patient often needs to repeat various laboratory and pathological tests. This not only incurs huge medical bills but also has adverse effects on the human body. The replicated blockchain ledger aids in avoiding medical tests.
- Security: The existing client/server-based system is prone to different cyber-attacks such as phishing and hacking. The stolen health records can be used to buy medical equipment by creating a fake ID or combining a patient number with a false provider to claim medical insurance. Table 1 shows the number of health data records breached in America based on a report by the Health Insurance Portability and Accountability Act (HIPAA) [50], and the cost per breached health record based on a report by the Federal Bureau [51] between 2009–2019. This cost of health record breach includes the expenses for forensic experts, outsourcing hotline support, the value of customer loss and free subscriptions and discounts for future services [52]. The table shows a spike in the number of health records breached in 2015. This is due to the largest health records breach encountered so far by the health insurance company, Anthem, with almost 78.8 million individuals affected as the patients’ records were not encrypted [53]. The immutability feature of blockchain ensures data security.
4. A Blockchain-Based Healthcare System Model
5. Performance Evaluation
5.1. Methods
5.1.1. Application Scenarios
5.1.2. Experimental Environment
5.2. Results Analysis
6. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Jamoom, E.; Yang, N.; Hing, E. Adoption of Certified Electronic Health Record Systems and Electronic Information Sharing in Physician Offices: United States, 2013 and 2014; Technical Report 236, NCHS Data Brief; U.S. Department of Health and Human Services, Centers for Disease Control and Prevention, National Center for Health Statistics: Hyattsville, MD, USA, 2016.
- The HIPAA Privacy Rule. Available online: https://www.hhs.gov/hipaa/for-professionals/privacy/index.html (accessed on 5 March 2020).
- Directive 95/46/EC of the European Parliament and of the Council of 24 October 1995 on the Protection of Individuals with Regard to the Processing of Personal Data and on the Free Movement of Such Data. Available online: https://eur-lex.europa.eu/legal-content/EN/TXT/?uri=CELEX%3A31995L0046 (accessed on 5 March 2020).
- Nakamoto, S. Bitcoin: A Peer-to-Peer Electronic Cash System. Available online: https://bitcoin.org/bitcoin.pdf (accessed on 20 July 2020).
- Ismail, L.; Hameed, H.; AlShamsi, M.; AlHammadi, M.; AlDhanhani, N. Towards a Blockchain Deployment at UAE University: Performance Evaluation and Blockchain Taxonomy. In Proceedings of the 2019 International Conference on Blockchain Technology, Honolulu, HI, USA, 15–18 March 2019; Association for Computing Machinery: New York, NY, USA, 2019; pp. 30–38. [Google Scholar]
- Ismail, L.; Materwala, H. A Review of Blockchain Architecture and Consensus Protocols: Use Cases, Challenges, and Solutions. Symmetry 2019, 11, 1198. [Google Scholar] [CrossRef] [Green Version]
- Hölbl, M.; Kompara, M.; Kamišalić, A.; Nemec Zlatolas, L. A systematic review of the use of blockchain in healthcare. Symmetry 2018, 10, 470. [Google Scholar] [CrossRef] [Green Version]
- Dagher, G.G.; Mohler, J.; Milojkovic, M.; Marella, P.B. Ancile: Privacy-preserving framework for access control and interoperability of electronic health records using blockchain technology. Sustain. Cities Soc. 2018, 39, 283–297. [Google Scholar] [CrossRef]
- Fan, K.; Wang, S.; Ren, Y.; Li, H.; Yang, Y. Medblock: Efficient and secure medical data sharing via blockchain. J. Med. Syst. 2018, 42, 136. [Google Scholar] [CrossRef] [PubMed]
- Uddin, M.A.; Stranieri, A.; Gondal, I.; Balasubramanian, V. Continuous patient monitoring with a patient centric agent: A block architecture. IEEE Access 2018, 6, 32700–32726. [Google Scholar] [CrossRef]
- Who Owns Medical Records: 50 State Comparison. Available online: http://www.healthinfolaw.org/comparative-analysis/who-owns-medical-records-50-state-comparison (accessed on 5 March 2020).
- Introduction-HealthVault Development. Available online: https://docs.microsoft.com/en-us/healthvault/introduction/introduction (accessed on 5 March 2020).
- MTBC PHR: Personal Health Records for Patients. Available online: https://phr.mtbc.com/phrdefault.aspx (accessed on 5 March 2020).
- OpenClinical e-Health Applications: MyPHR. Available online: http://www.openclinical.org/publicApp_myPHR.html (accessed on 5 March 2020).
- Capzule PHR: Your Family Health Data in One App. (Personal Medical/Health Records). Available online: https://www.capzule.com/ (accessed on 5 March 2020).
- My Medical—The Personal Medical Record for You, The Patient. Available online: http://mymedicalapp.com/ (accessed on 5 March 2020).
- Individual Electronic Healthrecord-GenexEHR. Available online: https://www.genexehr.com/individual-electronic-healthrecord (accessed on 5 March 2020).
- Saravanan, M.; Shubha, R.; Marks, A.M.; Iyer, V. SMEAD: A secured mobile enabled assisting device for diabetics monitoring. In Proceedings of the 2017 IEEE International Conference on Advanced Networks and Telecommunications Systems (ANTS), Bhubaneswar, India, 17–20 December 2017; IEEE: Piscataway, NJ, USA, 2017; pp. 1–6. [Google Scholar]
- Liang, X.; Zhao, J.; Shetty, S.; Liu, J.; Li, D. Integrating blockchain for data sharing and collaboration in mobile healthcare applications. In Proceedings of the 2017 IEEE 28th Annual International Symposium on Personal, Indoor, and Mobile Radio Communications (PIMRC), Montreal, QC, Canada, 8–13 October 2017; IEEE: Piscataway, NJ, USA, 2017; pp. 1–5. [Google Scholar]
- Patel, V. A framework for secure and decentralized sharing of medical imaging data via blockchain consensus. Health Inf. J. 2019, 25, 1398–1411. [Google Scholar] [CrossRef]
- Juneja, A.; Marefat, M. Leveraging blockchain for retraining deep learning architecture in patient-specific arrhythmia classification. In Proceedings of the 2018 IEEE EMBS International Conference on Biomedical & Health Informatics (BHI), Las Vegas, NV, USA, 4–7 March 2018; IEEE: Piscataway, NJ, USA, 2018; pp. 393–397. [Google Scholar]
- Griggs, K.N.; Ossipova, O.; Kohlios, C.P.; Baccarini, A.N.; Howson, E.A.; Hayajneh, T. Healthcare blockchain system using smart contracts for secure automated remote patient monitoring. J. Med. Syst. 2018, 42, 130. [Google Scholar] [CrossRef]
- Kleinaki, A.S.; Mytis-Gkometh, P.; Drosatos, G.; Efraimidis, P.S.; Kaldoudi, E. A blockchain-based notarization service for biomedical knowledge retrieval. Comput. Struct. Biotechnol. J. 2018, 16, 288–297. [Google Scholar] [CrossRef]
- Mytis-Gkometh, P.; Drosatos, G.; Efraimidis, P.; Kaldoudi, E. Notarization of knowledge retrieval from biomedical repositories using blockchain technology. In Precision Medicine Powered by pHealth and Connected Health; Springer: Singapore, 2018; pp. 69–73. [Google Scholar]
- Wu, H.; Shang, Y.; Wang, L.; Shi, L.; Jiang, K.; Dong, J. A Patient-Centric Interoperable Framework for Health Information Exchange via Blockchain. In Proceedings of the 2019 2nd International Conference on Blockchain Technology and Applications, Xi’an, China, 9–11 December 2019; Association for Computing Machinery: New York, NY, USA, 2019; pp. 76–80. [Google Scholar]
- Wang, H.; Song, Y. Secure cloud-based EHR system using attribute-based cryptosystem and blockchain. J. Med. Syst. 2018, 42, 152. [Google Scholar] [CrossRef]
- Zhang, X.; Poslad, S. Blockchain support for flexible queries with granular access control to electronic medical records (EMR). In Proceedings of the 2018 IEEE International Conference on Communications (ICC), Kansas City, MO, USA, 20–24 May 2018; IEEE: Piscataway, NJ, USA, 2018; pp. 1–6. [Google Scholar]
- Badr, S.; Gomaa, I.; Abd-Elrahman, E. Multi-tier blockchain framework for IoT-EHRs systems. Procedia Comput. Sci. 2018, 141, 159–166. [Google Scholar] [CrossRef]
- Guo, R.; Shi, H.; Zhao, Q.; Zheng, D. Secure attribute-based signature scheme with multiple authorities for blockchain in electronic health records systems. IEEE Access 2018, 6, 11676–11686. [Google Scholar] [CrossRef]
- Zhang, J.; Xue, N.; Huang, X. A secure system for pervasive social network-based healthcare. IEEE Access 2016, 4, 9239–9250. [Google Scholar] [CrossRef]
- Brogan, J.; Baskaran, I.; Ramachandran, N. Authenticating health activity data using distributed ledger technologies. Comput. Struct. Biotechnol. J. 2018, 16, 257–266. [Google Scholar] [CrossRef]
- Hussein, A.F.; ArunKumar, N.; Ramirez-Gonzalez, G.; Abdulhay, E.; Tavares, J.M.R.; de Albuquerque, V.H.C. A medical records managing and securing blockchain based system supported by a genetic algorithm and discrete wavelet transform. Cogn. Syst. Res. 2018, 52, 1–11. [Google Scholar] [CrossRef] [Green Version]
- Chen, L.; Lee, W.K.; Chang, C.C.; Choo, K.K.R.; Zhang, N. Blockchain based searchable encryption for electronic health record sharing. Future Gener. Comput. Syst. 2019, 95, 420–429. [Google Scholar] [CrossRef]
- Zghaibeh, M.; Farooq, U.; Hasan, N.U.; Baig, I. SHealth: A Blockchain-Based Health System With Smart Contracts Capabilities. IEEE Access 2020, 8, 70030–70043. [Google Scholar] [CrossRef]
- Azaria, A.; Ekblaw, A.; Vieira, T.; Lippman, A. Medrec: Using blockchain for medical data access and permission management. In Proceedings of the 2016 2nd International Conference on Open and Big Data (OBD), Vienna, Austria, 22–24 August 2016; IEEE: Piscataway, NJ, USA, 2016; pp. 25–30. [Google Scholar]
- Li, H.; Zhu, L.; Shen, M.; Gao, F.; Tao, X.; Liu, S. Blockchain-based data preservation system for medical data. J. Med. Syst. 2018, 42, 141. [Google Scholar] [CrossRef] [PubMed]
- Dey, T.; Jaiswal, S.; Sunderkrishnan, S.; Katre, N. HealthSense: A medical use case of Internet of Things and blockchain. In Proceedings of the 2017 International conference on intelligent sustainable systems (ICISS), Palladam, India, 7–8 December 2017; IEEE: Piscataway, NJ, USA, 2017; pp. 486–491. [Google Scholar]
- Yue, X.; Wang, H.; Jin, D.; Li, M.; Jiang, W. Healthcare data gateways: Found healthcare intelligence on blockchain with novel privacy risk control. J. Med. Syst. 2016, 40, 218. [Google Scholar] [CrossRef]
- Wang, S.; Wang, J.; Wang, X.; Qiu, T.; Yuan, Y.; Ouyang, L.; Guo, Y.; Wang, F.Y. Blockchain-powered parallel healthcare systems based on the ACP approach. IEEE Trans. Comput. Soc. Syst. 2018, 5, 942–950. [Google Scholar] [CrossRef]
- Roehrs, A.; da Costa, C.A.; da Rosa Righi, R. OmniPHR: A distributed architecture model to integrate personal health records. J. Biomed. Inf. 2017, 71, 70–81. [Google Scholar] [CrossRef]
- Kaur, H.; Alam, M.A.; Jameel, R.; Mourya, A.K.; Chang, V. A proposed solution and future direction for blockchain-based heterogeneous medicare data in cloud environment. J. Med. Syst. 2018, 42, 156. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Aswin, A.; Basil, K.; Viswan, V.P.; Reji, B.; Kuriakose, B. Design of AYUSH: A Blockchain-Based Health Record Management System. In Inventive Communication and Computational Technologies; Springer: Singapore, 2020; pp. 665–672. [Google Scholar]
- Tanwar, S.; Parekh, K.; Evans, R. Blockchain-based electronic healthcare record system for healthcare 4.0 applications. J. Inf. Secur. Appl. 2020, 50, 102407. [Google Scholar] [CrossRef]
- Bitcoin Mining Consumes More Electricity a Year Than Ireland. Available online: https://www.theguardian.com/technology/2017/nov/27/bitcoin-mining-consumes-electricity-ireland (accessed on 3 May 2020).
- Bitcoin Energy Consumption Index. Available online: https://digiconomist.net/bitcoin-energy-consumption (accessed on 3 May 2020).
- Scherer, M. Performance and Scalability of Blockchain Networks and Smart Contracts. Ph.D. Thesis, Umeå University, Faculty of Science and Technology, Department of Computing Science, Umeå, Sweden, 2017. [Google Scholar]
- What is Practical Byzantine Fault Tolerance (pBFT)? Available online: https://crushcrypto.com/what-is-practical-byzantine-fault-tolerance/ (accessed on 3 May 2020).
- Zheng, Z.; Xie, S.; Dai, H.N.; Chen, X.; Wang, H. Blockchain challenges and opportunities: A survey. Int. J. Web Grid Serv. 2018, 14, 352–375. [Google Scholar] [CrossRef]
- Pseudonymity. Available online: https://en.wikipedia.org/wiki/Pseudonymity (accessed on 3 May 2020).
- Healthcare Data Breach Statistics. Available online: https://www.hipaajournal.com/healthcare-data-breach-statistics/ (accessed on 3 May 2020).
- Health Care Systems and Medical Devices at Risk for Increased Cyber Intrusions for Financial Gain. Available online: http://www.calhospital.org/sites/main/files/file-attachments/dp___attachment_fbi_alert.pdf (accessed on 3 May 2020).
- Health Sector Cybersecurity Coordination Center (HC3). A Cost Analysis of Healthcare Sector Data Breaches. Available online: https://content.govdelivery.com/attachments/USDHSCIKR/2019/04/16/file_attachments/1193648/HC3%20-%20HPH%20Breach%20Cost%20whitepaper.pdf (accessed on 28 May 2020).
- The Breach of Anthem Health—The Largest Healthcare Breach in History. Available online: https://resources.infosecinstitute.com/category/healthcare-information-security/healthcare-attack-statistics-and-case-studies/case-study-health-insurer-anthem/#gref (accessed on 24 June 2020).
- Castro, M.; Liskov, B. Practical Byzantine fault tolerance. In Proceedings of the 3rd Symposium on Operating System Design and Implementation (OSDI), New Orleans, LA, USA, 22–25 February 1999; Unisex Association: Berkeley, CA, USA, 1999; pp. 173–186. [Google Scholar]
- Hodge, J.G.; Kaufman, T.; Jaques, C. Legal Issues Concerning Identifiable Health Data Sharing Between State/Local Public Health Authorities and Tribal Epidemiology Centers in Selected US Jurisdiction. 2011. Available online: https://cdn.ymaws.com/www.cste.org/resource/resmgr/PDFs/LegalIssuesTribalJuris.pdf (accessed on 21 June 2020).
- Health Information Privacy Law and Policy | HealthIT.gov. Available online: https://www.healthit.gov/topic/health-information-privacy-law-and-policy (accessed on 21 June 2020).
- Data Protection Act 1998. Available online: http://www.legislation.gov.uk/ukpga/1998/29/contents (accessed on 21 June 2020).
- The Human Rights Act 1998 | Department of Health. Available online: https://www.health-ni.gov.uk/articles/human-rights-act-1998 (accessed on 21 June 2020).
- The HIPAA Security Rule. Available online: https://www.hhs.gov/hipaa/for-professionals/security/index.html (accessed on 21 June 2020).
- Merkle, R.C. A digital signature based on a conventional encryption function. In Conference on the Theory and Application of Cryptographic Techniques; Springer: Berlin/Heidelberg, Germany, 1987; pp. 369–378. [Google Scholar]
- Ruiz, M.G.; Chaves, A.G.; Ibañez, C.R.; Mazo, J.M.G.; Giraldo, J.C.R.; Echavarria, A.P.; Diaz, E.V.; Restrepo, G.P.; Munera, E.N.M.; Loaiza, B.G.; et al. mantisGRID: A grid platform for DICOM medical images management in Colombia and Latin America. J. Digit. Imaging 2011, 24, 271–283. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- SHA-256 Cryptographic Hash Algorithm. Available online: https://www.movable-type.co.uk/scripts/sha256.html (accessed on 5 March 2020).
- National Hospital Ambulatory Medical Care Survey: 2017 Emergency Department Summary Tables. Available online: https://www.cdc.gov/nchs/data/nhamcs/web_tables/2017_ed_web_tables-508.pdf (accessed on 5 March 2020).
- ns-3 | A Discrete-Event Network Simulator for Internet Systems. Available online: https://www.nsnam.org/ (accessed on 5 March 2020).













| Year | Number of Health Records Breached | Cost per Breached Record (USD) |
|---|---|---|
| 2009 | 0 | 204 |
| 2010 | 6,006,063 | 214 |
| 2011 | 13,407,992 | 194 |
| 2012 | 2,808,042 | 233 |
| 2013 | 7,401,928 | 255 |
| 2014 | 12,946,972 | 308 |
| 2015 | 113,270,000 | 363 |
| 2016 | 27,300,000 | 355 |
| 2017 | 5,138,179 | 380 |
| 2018 | 13,947,909 | 408 |
| 2019 | 41,335,889 | 429 |
| Average Increase in Execution Time (Hours) | |||||
|---|---|---|---|---|---|
| Health Records Update | Health Records Query | ||||
| Increasing variable | Variable increasing factor | Client/server | Blockchain | Client/server | Blockchain |
| Number of health records | +1000 | 2.03 | 14.36 | 2.03 | 0.14 |
| Number of hospitals | +10 | 4.42 | 57.44 | 4.42 | 0.58 |
| Average Increase in Data Transfer (GB) | |||||
|---|---|---|---|---|---|
| Health Records Update | Health Records Query | ||||
| Increasing variable | Variable increasing factor | Client/server | Blockchain | Client/server | Blockchain |
| Number of health records | +1000 | 25.86 | 258.61 | 25.86 | 28.18 |
| Number of hospitals | +10 | 0 | 1034.98 | 0 | 10.34 |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Ismail, L.; Materwala, H. Blockchain Paradigm for Healthcare: Performance Evaluation. Symmetry 2020, 12, 1200. https://doi.org/10.3390/sym12081200
Ismail L, Materwala H. Blockchain Paradigm for Healthcare: Performance Evaluation. Symmetry. 2020; 12(8):1200. https://doi.org/10.3390/sym12081200
Chicago/Turabian StyleIsmail, Leila, and Huned Materwala. 2020. "Blockchain Paradigm for Healthcare: Performance Evaluation" Symmetry 12, no. 8: 1200. https://doi.org/10.3390/sym12081200
APA StyleIsmail, L., & Materwala, H. (2020). Blockchain Paradigm for Healthcare: Performance Evaluation. Symmetry, 12(8), 1200. https://doi.org/10.3390/sym12081200