Insights into the Relationship between Periodontitis and Systemic Sclerosis Based on the New Periodontitis Classification (2018): A Cross-Sectional Study
Abstract
:1. Introduction
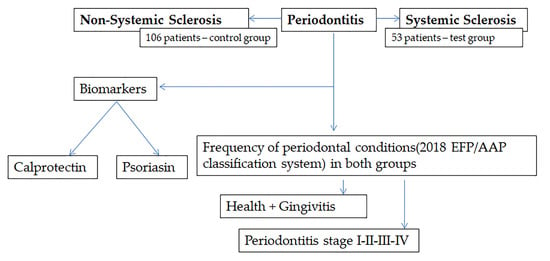
2. Materials and Methods
2.1. Study Design
2.2. Participants, Inclusion Criteria, and Sample Size Calculation
2.3. Evaluation of Demographic and Systemic Medical Characteristics
2.4. Systemic Sclerosis-Associated Variables of Interest
2.5. Periodontal Parameters of Interest and Assessment Method: Case Definitions of Periodontal Conditions
2.5.1. Parameters of Interest and Assessment Method
2.5.2. Case Definition of Periodontal Conditions
2.6. Saliva Sampling and Salivary Flow Rate Measurement
2.7. Quantification of Salivary S100A8 and S100A9/Immunoenzymatic Testing (ELISA)
2.8. Statistical Analysis
3. Results
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Correction Statement
References
- Lescoat, A.; Huang, S.; Carreira, P.E.; Siegert, E.; de Vries-Bouwstra, J.; Distler, J.H.W.; Smith, V.; Del Galdo, F.; Anic, B.; Damjanov, N.; et al. Cutaneous Manifestations, Clinical Characteristics, and Prognosis of Patients with Systemic Sclerosis Sine Scleroderma: Data from the International EUSTAR Database. JAMA Dermatol. 2023, 159, 837–847. [Google Scholar] [CrossRef] [PubMed]
- Zhang, S.; Zhu, J.; Zhu, Y.; Zhang, X.; Wu, R.; Li, S.; Su, Y. Oral Manifestations of Patients with Systemic Sclerosis: A Meta-Analysis for Case-Controlled Studies. BMC Oral Health 2021, 21, 250. [Google Scholar] [CrossRef] [PubMed]
- Ciurea, A.; Rednic, N.V.; Soancă, A.; Micu, I.C.; Stanomir, A.; Oneț, D.; Șurlin, P.; Filipescu, I.; Roman, A.; Stratul, Ș.I.; et al. Current Perspectives on Periodontitis in Systemic Sclerosis: Associative Relationships, Pathogenic Links, and Best Practices. Diagnostics 2023, 13, 841. [Google Scholar] [CrossRef] [PubMed]
- Oral Disorders Collaborators. Global, Regional, and National Levels and Trends in Burden of Oral Conditions from 1990 to 2017: A Systematic Analysis for the Global Burden of Disease 2017 Study. J. Dent. Res. 2020, 99, 362–373. [Google Scholar] [CrossRef] [PubMed]
- Wu, C.-Z.; Yuan, Y.-H.; Liu, H.-H.; Li, S.-S.; Zhang, B.-W.; Chen, W.; An, Z.-J.; Chen, S.-Y.; Wu, Y.-Z.; Han, B.; et al. Epidemiologic Relationship between Periodontitis and Type 2 Diabetes Mellitus. BMC Oral Health 2020, 20, 204. [Google Scholar] [CrossRef] [PubMed]
- Sanz, M.; Del Castillo, A.M.; Jepsen, S.; Gonzalez-Juanatey, J.R.; D’Aiuto, F.; Bouchard, P.; Chapple, I.; Dietrich, T.; Gotsman, I.; Graziani, F.; et al. Periodontitis and Cardiovascular Diseases: Consensus Report. J. Clin. Periodontol. 2020, 47, 268–288. [Google Scholar] [CrossRef] [PubMed]
- Costea, C.A.; Christodorescu, R.; Soancă, A.; Roman, A.; Micu, I.C.; Stratul, Ș.I.; Rusu, D.; Popescu, D.M.; Popa-Wagner, A.; Bulboacă, A.E. Periodontitis in Ischemic Stroke Patients: Case Definition Challenges of the New Classification Scheme (2018). J. Clin. Med. 2022, 11, 520. [Google Scholar] [CrossRef] [PubMed]
- Pan, W.; Wang, Q.; Chen, Q. The Cytokine Network Involved in the Host Immune Response to Periodontitis. Int. J. Oral Sci. 2019, 11, 30. [Google Scholar] [CrossRef]
- da Silva, G.S.G.; de Melo, M.L.M.; Leão, J.C.; Carvalho, A.T.; Porter, S.; Duarte, A.L.B.P.; Dantas, A.T.; Gueiros, L.A. Oral Features of Systemic Sclerosis: A Case-Control Study. Oral Dis. 2019, 25, 1995–2002. [Google Scholar] [CrossRef]
- Wood, R.E.; Lee, P. Analysis of the Oral Manifestations of Systemic Sclerosis (Scleroderma). Oral Surg. Oral Med. Oral Pathol. 1988, 65, 172–178. [Google Scholar] [CrossRef]
- Leung, W.K.; Chu, C.H.; Mok, M.Y.; Yeung, K.W.S.; Ng, S.K.S. Periodontal Status of Adults with Systemic Sclerosis: Case-Control Study. J. Periodontol. 2011, 82, 1140–1145. [Google Scholar] [CrossRef] [PubMed]
- Chu, C.H.; Yeung, C.M.K.; Lai, I.A.; Leung, W.K.; Mok, M.Y. Oral Health of Chinese People with Systemic Sclerosis. Clin. Oral. Investig. 2011, 15, 931–939. [Google Scholar] [CrossRef] [PubMed]
- Baron, M.; Hudson, M.; Tatibouet, S.; Steele, R.; Lo, E.; Gravel, S.; Gyger, G.; El Sayegh, T.; Pope, J.; Fontaine, A.; et al. The Canadian Systemic Sclerosis Oral Health Study: Orofacial Manifestations and Oral Health-Related Quality of Life in Systemic Sclerosis Compared with the General Population. Rheumatology 2014, 53, 1386–1394. [Google Scholar] [CrossRef] [PubMed]
- Elimelech, R.; Mayer, Y.; Braun-Moscovici, Y.; Machtei, E.E.; Balbir-Gurman, A. Periodontal Conditions and Tumor Necrosis Factor-Alpha Level in Gingival Crevicular Fluid of Scleroderma Patients. Isr. Med. Assoc. J. 2015, 17, 549–553. [Google Scholar]
- Iordache, C.; Antohe, M.-E.; Chirieac, R.; Ancuța, E.; Țănculescu, O.; Ancuța, C. Volumetric Cone Beam Computed Tomography for the Assessment of Oral Manifestations in Systemic Sclerosis: Data from an EUSTAR Cohort. J. Clin. Med. 2019, 8, 1620. [Google Scholar] [CrossRef] [PubMed]
- Isola, G.; Williams, R.C.; Lo Gullo, A.; Ramaglia, L.; Matarese, M.; Iorio-Siciliano, V.; Cosio, C.; Matarese, G. Risk Association between Scleroderma Disease Characteristics, Periodontitis, and Tooth Loss. Clin. Rheumatol. 2017, 36, 2733–2741. [Google Scholar] [CrossRef]
- Isola, G.; Palazzo, G.; Polizzi, A.; Murabito, P.; Giuffrida, C.; Lo Gullo, A. Association of Systemic Sclerosis and Periodontitis with Vitamin D Levels. Nutrients 2021, 13, 705. [Google Scholar] [CrossRef]
- Mayer, Y.; Elimelech, R.; Balbir-Gurman, A.; Braun-Moscovici, Y.; Machtei, E.E. Periodontal Condition of Patients with Autoimmune Diseases and the Effect of Anti-Tumor Necrosis Factor-α Therapy. J. Periodontol. 2013, 84, 136–142. [Google Scholar] [CrossRef]
- Pischon, N.; Hoedke, D.; Kurth, S.; Lee, P.; Dommisch, H.; Steinbrecher, A.; Pischon, T.; Burmester, G.R.; Buttgereit, F.; Detert, J.; et al. Increased Periodontal Attachment Loss in Patients with Systemic Sclerosis. J. Periodontol. 2016, 87, 763–771. [Google Scholar] [CrossRef]
- Jud, P.; Wimmer, G.; Meinitzer, A.; Strohmaier, H.; Schwantzer, G.; Moazedi-Fürst, F.; Schweiger, L.; Brodmann, M.; Hafner, F.; Arefnia, B. Periodontal Disease and Its Association to Endothelial Dysfunction and Clinical Changes in Limited Systemic Sclerosis: A Case-Control Study. J. Periodontal Res. 2023, 58, 621–633. [Google Scholar] [CrossRef]
- Almeida, T.G.; Ferreira, A.R.H.; da Silva, F.S.; Chaves, C.C.; Assunção, B.N.; Martins, P.S.; das Dores, A.S.; de Moura, R.M.F.; Andrade, J.A.; Santos, F.P.S.T.; et al. Oral Health Education for Systemic Sclerosis Patients: A Booklet Report. PEC Innov. 2023, 2, 100154. [Google Scholar] [CrossRef]
- Kotsiou, O.S.; Papagiannis, D.; Papadopoulou, R.; Gourgoulianis, K.I. Calprotectin in Lung Diseases. Int. J. Mol. Sci. 2021, 22, 1706. [Google Scholar] [CrossRef]
- Wang, S.; Song, R.; Wang, Z.; Jing, Z.; Wang, S.; Ma, J. S100A8/A9 in Inflammation. Front. Immunol. 2018, 9, 1298. [Google Scholar] [CrossRef] [PubMed]
- Gao, H.; Xu, J.; He, L.; Meng, H.; Hou, J. Calprotectin Levels in Gingival Crevicular Fluid and Serum of Patients with Chronic Pe-Riodontitis and Type 2 Diabetes Mellitus before and after Initial Periodontal Therapy. J. Periodontal Res. 2021, 56, 121–130. [Google Scholar] [CrossRef] [PubMed]
- Wei, L.; Liu, M.; Xiong, H. Role of Calprotectin as a Biomarker in Periodontal Disease. Mediat. Inflamm. 2019, 2019, 3515026. [Google Scholar] [CrossRef] [PubMed]
- Johnstone, K.F.; Herzberg, M.C. Antimicrobial Peptides: Defending the Mucosal Epithelial Barrier. Front. Oral Health 2022, 3, 958480. [Google Scholar] [CrossRef] [PubMed]
- Kido, J.-I.; Kido, R.; Suryono; Kataoka, M.; Fagerhol, M.K.; Nagata, T. Calprotectin Release from Human Neutrophils Is Induced by Porphyromonas Gingivalis Lipopolysaccharide via the CD-14–Toll-like Receptor–Nuclear Factor κB Pathway. J. Periodontal Res. 2003, 38, 557–563. [Google Scholar] [CrossRef]
- Hiroshima, Y.; Sakamoto, E.; Yoshida, K.; Abe, K.; Naruishi, K.; Yamamoto, T.; Shinohara, Y.; Kido, J.-I.; Geczy, C.L. Advanced Glycation End-Products and Porphyromonas Gingivalis Lipopolysaccharide Increase Calprotectin Expression in Human Gingival Epithelial Cells. J. Cell. Biochem. 2018, 119, 1591–1603. [Google Scholar] [CrossRef]
- Champaiboon, C.; Sappington, K.J.; Guenther, B.D.; Ross, K.F.; Herzberg, M.C. Calprotectin S100A9 Calcium-Binding Loops I and II Are Essential for Keratinocyte Resistance to Bacterial Invasion. J. Biol. Chem. 2009, 284, 7078–7090. [Google Scholar] [CrossRef]
- Jukic, A.; Bakiri, L.; Wagner, E.F.; Tilg, H.; Adolph, T.E. Calprotectin: From Biomarker to Biological Function. Gut 2021, 70, 1978–1988. [Google Scholar] [CrossRef]
- Silvin, A.; Chapuis, N.; Dunsmore, G.; Goubet, A.-G.; Dubuisson, A.; Derosa, L.; Almire, C.; Hénon, C.; Kosmider, O.; Droin, N.; et al. Elevated Calprotectin and Abnormal Myeloid Cell Subsets Discriminate Severe from Mild COVID-19. Cell 2020, 182, 1401–1418.e18. [Google Scholar] [CrossRef] [PubMed]
- Gao, H.Y.; Huang, B.X.; Hou, J.X.; Meng, H.X. Preliminary study on the expression and distribution of S100A8 and S100A9 in healthy and experimental periodontitis tissues. Zhonghua Kou Qiang Yi Xue Za Zhi 2020, 55, 402–407. [Google Scholar] [CrossRef]
- Gao, H.; Hou, J.; Meng, H.; Zhang, X.; Zheng, Y.; Peng, L. Proinflammatory Effects and Mechanisms of Calprotectin on Human Gingival Fibroblasts. J. Periodontal Res. 2017, 52, 975–983. [Google Scholar] [CrossRef] [PubMed]
- Zheng, Y.; Hou, J.; Peng, L.; Zhang, X.; Jia, L.; Wang, X.; Wei, S.; Meng, H. The Pro-Apoptotic and pro-Inflammatory Effects of Calprotectin on Human Periodontal Ligament Cells. PLoS ONE 2014, 9, e110421. [Google Scholar] [CrossRef] [PubMed]
- Zreiqat, H.; Howlett, C.R.; Gronthos, S.; Hume, D.; Geczy, C.L. S100A8/S100A9 and Their Association with Cartilage and Bone. J. Mol. Histol. 2007, 38, 381–391. [Google Scholar] [CrossRef] [PubMed]
- Charoenpong, H.; Osathanon, T.; Pavasant, P.; Limjeerajarus, N.; Keawprachum, B.; Limjeerajarus, C.N.; Cheewinthamrongrod, V.; Palaga, T.; Lertchirakarn, V.; Ritprajak, P. Mechanical Stress Induced S100A7 Expression in Human Dental Pulp Cells to Augment Osteoclast Differentiation. Oral Dis. 2019, 25, 812–821. [Google Scholar] [CrossRef] [PubMed]
- Takahashi, T.; Asano, Y.; Yamashita, T.; Nakamura, K.; Saigusa, R.; Miura, S.; Ichimura, Y.; Toyama, T.; Hirabayashi, M.; Taniguchi, T.; et al. A Potential Contribution of Psoriasin to Vascular and Epithelial Abnormalities and Inflammation in Systemic Sclerosis. J. Eur. Acad. Dermatol. Venereol. 2018, 32, 291–297. [Google Scholar] [CrossRef]
- Giusti, L.; Sernissi, F.; Donadio, E.; Ciregia, F.; Giacomelli, C.; Giannaccini, G.; Mazzoni, M.R.; Lucacchini, A.; Bazzichi, L. Salivary Psoriasin (S100A7) Correlates with Diffusion Capacity of Carbon Monoxide in a Large Cohort of Systemic Sclerosis Patients. J. Transl. Med. 2016, 14, 262. [Google Scholar] [CrossRef]
- Dommisch, H.; Skora, P.; Hirschfeld, J.; Olk, G.; Hildebrandt, L.; Jepsen, S. The Guardians of the Periodontium-Sequential and Differential Expression of Antimicrobial Peptides during Gingival Inflammation. Results from in Vivo and in Vitro Studies. J. Clin. Periodontol. 2019, 46, 276–285. [Google Scholar] [CrossRef]
- Dommisch, H.; Staufenbiel, I.; Schulze, K.; Stiesch, M.; Winkel, A.; Fimmers, R.; Dommisch, J.; Jepsen, S.; Miosge, N.; Adam, K.; et al. Expression of Antimicrobial Peptides and Interleukin-8 during Early Stages of Inflammation: An Experimental Gingivitis Study. J. Periodontal Res. 2015, 50, 836–845. [Google Scholar] [CrossRef]
- Eberhard, J.; Pietschmann, R.; Falk, W.; Jepsen, S.; Dommisch, H. The Immune Response of Oral Epithelial Cells Induced by Single-species and Complex Naturally Formed Biofilms. Oral Microbiol. Immunol. 2009, 24, 325–330. [Google Scholar] [CrossRef] [PubMed]
- Kido, J.; Nakamura, T.; Kido, R.; Ohishi, K.; Yamauchi, N.; Kataoka, M.; Nagata, T. Calprotectin in Gingival Crevicular Fluid Correlates with Clinical and Biochemical Markers of Periodontal Disease. J. Clin. Periodontol. 1999, 26, 653–657. [Google Scholar] [CrossRef] [PubMed]
- Kido, J.; Bando, M.; Hiroshima, Y.; Iwasaka, H.; Yamada, K.; Ohgami, N.; Nambu, T.; Kataoka, M.; Yamamoto, T.; Shinohara, Y.; et al. Analysis of Proteins in Human Gingival Crevicular Fluid by Mass Spectrometry: Mass Spectrometric Analysis of Gingival Crevicular Fluid. J. Periodontal Res. 2012, 47, 488–499. [Google Scholar] [CrossRef] [PubMed]
- Nakamura, T.; Kido, J.-I.; Kido, R.; Ohishi, K.; Yamauchi, N.; Kataoka, M.; Nagata, T. The Association of Calprotectin Level in Gingival Crevicular Fluid with Gingival Index and the Activities of Collagenase and Aspartate Aminotransferase in Adult Periodontitis Patients. J. Periodontol. 2000, 71, 361–367. [Google Scholar] [CrossRef] [PubMed]
- von Elm, E.; Altman, D.G.; Egger, M.; Pocock, S.J.; Gøtzsche, P.C.; Vandenbroucke, J.P.; STROBE Initiative. The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) Statement: Guidelines for Reporting Observational Studies. Int. J. Surg. 2014, 12, 1495–1499. [Google Scholar] [CrossRef] [PubMed]
- Van Den Hoogen, F.; Khanna, D.; Fransen, J. Classification Criteria for Systemic Sclerosis: An American College of Rheumatology/European League Against Rheumatism Collaborative Initiative: ACR/EULAR Classification Criteria for SSc. Arthritis Rheum. 2013, 65, 2737–2747. [Google Scholar] [CrossRef] [PubMed]
- Faul, F.; Erdfelder, E.; Lang, A.-G.; Buchner, A. G*Power 3: A Flexible Statistical Power Analysis Program for the Social, Behavioral, and Biomedical Sciences. Behav. Res. Methods 2007, 39, 175–191. [Google Scholar] [CrossRef]
- NHIS—Adult Tobacco Use—Glossary. 2019. Available online: https://www.cdc.gov/nchs/nhis/tobacco/tobacco_glossary.htm (accessed on 10 November 2023).
- NHIS—Adult Alcohol Use—Glossary. 2019. Available online: https://www.cdc.gov/nchs/nhis/alcohol/alcohol_glossary.htm (accessed on 10 November 2023).
- Micu, I.C.; Roman, A.; Ticala, F.; Soanca, A.; Ciurea, A.; Objelean, A.; Iancu, M.; Muresan, D.; Caracostea, G.V. Relationship between Preterm Birth and Post-Partum Periodontal Maternal Status: A Hospital-Based Romanian Study. Arch. Gynecol. Obstet. 2020, 301, 1189–1198. [Google Scholar] [CrossRef]
- Eke, P.I.; Page, R.C.; Wei, L.; Thornton-Evans, G.; Genco, R.J. Update of the Case Definitions for Population-based Surveillance of Periodontitis. J. Periodontol. 2012, 83, 1449–1454. [Google Scholar] [CrossRef]
- Ainamo, J.; Bay, I. Problems and Proposals for Recording Gingivitis and Plaque. Int. Dent. J. 1975, 25, 229–235. [Google Scholar]
- Oleary, T.J.; Drake, R.B.; Naylor, J.E. The Plaque Control Record. J. Periodontol. 1972, 43, 38. [Google Scholar] [CrossRef] [PubMed]
- Papapanou, P.N.; Sanz, M.; Buduneli, N. Periodontitis: Consensus Report of Workgroup 2 of the 2017 World Workshop on the Classification of Periodontal and Peri-Implant Diseases and Conditions: Classification and Case Definitions for Periodontitis. J. Clin. Periodontol. 2018, 45, S162–S170. [Google Scholar] [CrossRef] [PubMed]
- Chapple, I.L.C.; Mealey, B.L.; Van Dyke, T.E.; Bartold, P.M.; Dommisch, H.; Eickholz, P.; Geisinger, M.L.; Genco, R.J.; Glogauer, M.; Goldstein, M.; et al. Periodontal Health and Gingival Diseases and Conditions on an Intact and a Reduced Periodontium: Consensus Report of Workgroup 1 of the 2017 World Workshop on the Classification of Periodontal and Peri-Implant Diseases and Conditions. J. Periodontol. 2018, 89 (Suppl. S1), S74–S84. [Google Scholar] [CrossRef] [PubMed]
- Bellagambi, F.G.; Lomonaco, T.; Salvo, P.; Vivaldi, F.; Hangouët, M.; Ghimenti, S.; Biagini, D.; Di Francesco, F.; Fuoco, R.; Errachid, A. Saliva Sampling: Methods and Devices. An Overview. Trends Analyt. Chem. 2020, 124, 115781. [Google Scholar] [CrossRef]
- Sacon, M.B.; Esteves, C.V.; Florezi, G.P.; Gonçalves, A.F.; Pannuti, C.M.; Lemos Junior, C.A. Comparison of Two Methods for Sialometry: Weighing and Volume Techniques. Clin. Lab. Res. Dent. 2018, 1–7. [Google Scholar] [CrossRef]
- Henson, B.S.; Wong, D.T. Collection, Storage, and Processing of Saliva Samples for Downstream Molecular Applications. Methods Mol. Biol. 2010, 666, 21–30. [Google Scholar] [CrossRef] [PubMed]
- SankeyMATIC. Sankeymatic.com. Available online: https://sankeymatic.com/ (accessed on 10 November 2023).
- Løfblad, L.; Hov, G.G.; Åsberg, A.; Videm, V. Inflammatory Markers and Risk of Cardiovascular Mortality in Relation to Diabetes Status in the HUNT Study. Sci. Rep. 2021, 11, 15644. [Google Scholar] [CrossRef]
- Kim, H.-D.; Karna, S.; Shin, Y.; Vu, H.; Cho, H.-J.; Kim, S. S100A8 and S100A9 in Saliva, Blood and Gingival Crevicular Fluid for Screening Established Periodontitis: A Cross-Sectional Study. BMC Oral Health 2021, 21, 388. [Google Scholar] [CrossRef]
- Kajiura, Y.; Lew, J.-H.; Ikuta, T.; Nishikawa, Y.; Kido, J.-I.; Nagata, T.; Naruishi, K. Clinical Significance of GCF sIL-6R and Calprotectin to Evaluate the Periodontal Inflammation. Ann. Clin. Biochem. 2017, 54, 664–670. [Google Scholar] [CrossRef]
- Zhou, M.; Meng, H.X.; Zhao, Y.B.; Chen, Z.B. Changes of Four Proinflammatory Proteins in Whole Saliva during Experimental Gingivitis. Chin. J. Dent. Res. 2012, 15, 121–127. [Google Scholar]
- Holmström, S.B.; Lira-Junior, R.; Zwicker, S.; Majster, M.; Gustafsson, A.; Åkerman, S.; Klinge, B.; Svensson, M.; Boström, E.A. MMP-12 and S100s in Saliva Reflect Different Aspects of Periodontal Inflammation. Cytokine 2019, 113, 155–161. [Google Scholar] [CrossRef]


| Group | SSc (n = 53) | Control (n = 106) | p-Value |
|---|---|---|---|
| Age (years), median (IQR) | 52 (45–59) | 53 (46.25–61) | 0.544 |
| Sex (female), n (%) | 44 (83.02) | 85 (80.19) | 0.667 |
| Residential area (rural), n (%) | 26 (49.06) | 25 (23.58) | 0.001 |
| Smoking, n (%) | 0.253 | ||
| Yes | 7 (13.21) | 16 (15.09) | |
| Former smoker | 4 (7.55) | 2 (1.89) | |
| No | 42 (79.25) | 88 (83.02) | |
| Alcohol consumption, n (%) | 10 (18.87) | 46 (43.4) | 0.002 |
| Education, n (%) | <0.001 | ||
| Primary school | 2 (3.77) | 0 (0) | |
| Gymnasium | 8 (15.09) | 1 (0.94) | |
| High school | 30 (56.6) | 75 (70.75) | |
| University | 12 (22.64) | 30 (28.3) | |
| Vocational school | 1 (1.89) | 0 (0) | |
| BMI (kg/m2), median (IQR) | 25.25 (22.32–30.12) | 26.52 (23.9–29.32) | 0.21 |
| Diabetes, n (%) | 2 (3.77) | 25 (23.58) | 0.002 |
| Hypertension, n (%) | 15 (28.3) | 72 (67.92) | <0.001 |
| Dyslipidemia, n (%) | 26 (49.06) | 57 (53.77) | 0.575 |
| Systemic manifestations in SSc group | |||
| Cardiac score, n (%) | 11 (20.75) * | ||
| 0 | 42 (79.25) | ||
| 1 | 10 (18.87) | ||
| 2 | 1 (1.89) | ||
| Digestive score, n (%) | 33 (62.26) * | ||
| 0 | 20 (37.74) | ||
| 1 | 16 (30.19) | ||
| 2 | 14 (26.42) | ||
| 3 | 2 (3.77) | ||
| 4 | 1 (1.89) | ||
| Musculoskeletal score, n (%) | 43 (81.13) * | ||
| 0 | 10 (18.87) | ||
| 1 | 18 (33.96) | ||
| 2 | 22 (41.51) | ||
| 3 | 1 (1.89) | ||
| 4 | 2 (3.77) | ||
| Interstitial fibrous pneumopathy | 30 (56.6) | ||
| Telangiectasia | 35 (66.04) | ||
| Rodnan score, median (IQR) [range] | 7 (3–10) [0–38] | ||
| Anti-centromere antibodies, n (%) | 19 (35.85) | ||
| Anti-SCL70 antibodies, n (%) | 40 (75.47) |
| Group | SSc | Control | p-Value |
|---|---|---|---|
| (n = 53) | (n = 106) | ||
| OHI (%), median (IQR) | 36 (25–80) | 40.5 (20–71) | 0.591 |
| GBI (%), median (IQR) | 28 (13–45) | 26.5 (12–52) | 0.932 |
| No. of examined teeth, median (IQR) | 17 (11–23) | 17 (11–22.75) | 0.856 |
| Periodontal diagnosis, n (%) | 0.068 | ||
| Periodontal health | 3 (5.66) | 14 (13.21) | |
| Gingivitis | 3 (5.66) | 1 (0.94) | |
| Periodontitis | 47 (88.68) | 91 (85.85) | |
| Stage, n (%) | 0.767 | ||
| Stage I/II | 9 (16.98) | 21 (19.81) | |
| Stage III/IV | 38 (71.7) | 70 (66.04) | |
| Non-periodontitis | 6 (11.32) | 15 (14.15) | |
| Maximum CAL, median (IQR) | 6 (5–7) | 6 (4–8) | 0.706 |
| Median CAL, median (IQR) | 2.2 (1.29–3.29) | 2.5 (0.82–3.34) | 0.72 |
| Minimum CAL, median (IQR) | 0 (0–1) | 0 (0–1) | 0.269 |
| Median PD, median (IQR) | 2 (2–3) | 2 (2–2.38) | 0.701 |
| No. of sites with PD = 5 mm | 3 (1–9) | 3 (0–8.75) | 0.462 |
| No. of sites with PD > 5 mm | 3 (1–11) | 3 (0–11) | 0.628 |
| No. of sites with PD ≥ 6 mm | 0 (0–2) | 0 (0–2) | 0.925 |
| Salivary parameters | |||
| Unstimulated salivary flux (mL/min), median (IQR) | 0.22 (0.14–0.35) | 0.41 (0.38–0.43) | <0.001 |
| Stimulated salivary flux (mL/min), median (IQR) | 1.32 (0.6–2.2) | 2.43 (2.24–2.64) | <0.001 |
| Calprotectin (ng/mL), median (IQR) | 3.12 (2.3–4.15) | 3.51 (2.32–4.39) | 0.461 [n1 = 49, n2 = 98] |
| Psoriasin (ng/mL), median (IQR) | 0.67 (0.19–1.24) | 0.75 (0.36–1.49) | 0.305 [n1 = 14, n2 = 32] |
| Non-Periodontitis | ||||
|---|---|---|---|---|
| Biomarker | SSc (n = 6) | Control (n = 15) | Difference (95% CI) | p-value |
| Calprotectin (ng/mL), median (IQR) | 4.372 (4.11–4.607) | 2.899 (1.669–3.443) | 1.473 (−2.965–86) | 0.045 [n1 = 6, n2 = 14] |
| Psoriasin (ng/mL), median (IQR) | 0.028 (0.028–0.028) | 0.028 (0.028–0.028) | 0 (0–0) | 0.277 [n1 = 0, n2 = 3] |
| Stage I/II Periodontitis | ||||
| Biomarker | SSc (n = 9) | Control (n = 21) | Difference (95% CI) | p-value |
| Calprotectin (ng/mL), median (IQR) | 3.45 (2.588–4.635) | 3.358 (1.833–4.263) | 0.092 (−1.657–0.879) | 0.476 [n1 = 9, n2 = 20] |
| Psoriasin (ng/mL), median (IQR) | 0.028 (0.028–0.36) | 0.028 (0.028–0.028) | 0 (0–0.11) | 0.246 [n1 = 1, n2 = 6] |
| Stage III/IV Periodontitis | ||||
| Biomarker | SSc (n = 38) | Control (n = 70) | Difference (95% CI) | p-value |
| Calprotectin (ng/mL), median (IQR) | 2.676 (2.04–3.231) | 3.525 (2.22–4.438) | 0.848 (0–1.285) | 0.049 [n1 = 34, n2 = 64] |
| Psoriasin (ng/mL), median (IQR) | 0.028 (0.028–0.145) | 0.028 (0.028–0.338) | 0 (0–0) | 0.747 [n1 = 13, n2 = 23] |
| p-value * | 0.068 | 0.305 | ||
| p-value † | 0.206 | 0.706 | ||
| Periodontal Conditions | Frequency n (%) | |||
|---|---|---|---|---|
| 2012 CDC/AAP System 2018 EFP/AAP System | 2012 CDC/AAP | 2018 EFP/AAP | ||
| SSc | Control | SSc | Control | |
| Health + Gingivitis | 9 (16.98) | 22 (20.75) | 6 (11.32) | 15 (14.15) |
| Mild Periodontitis—Stage I | 4 (7.54) | 2 (1.88) | 2 (3.77) | 1 (0.94) |
| Moderate Periodontitis—Stage II | 20 (37.73) | 44 (41.50) | 14 (26.41) | 26 (24.52) |
| Severe Periodontitis—Stage III + IV | 20 (37.73) | 38 (35.84) | 31 (58.49) | 64 (60.37) |
| Total | 53 | 106 | 53 | 106 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Ciurea, A.; Stanomir, A.; Șurlin, P.; Micu, I.C.; Pamfil, C.; Leucuța, D.C.; Rednic, S.; Rasperini, G.; Soancă, A.; Țigu, A.B.; et al. Insights into the Relationship between Periodontitis and Systemic Sclerosis Based on the New Periodontitis Classification (2018): A Cross-Sectional Study. Diagnostics 2024, 14, 540. https://doi.org/10.3390/diagnostics14050540
Ciurea A, Stanomir A, Șurlin P, Micu IC, Pamfil C, Leucuța DC, Rednic S, Rasperini G, Soancă A, Țigu AB, et al. Insights into the Relationship between Periodontitis and Systemic Sclerosis Based on the New Periodontitis Classification (2018): A Cross-Sectional Study. Diagnostics. 2024; 14(5):540. https://doi.org/10.3390/diagnostics14050540
Chicago/Turabian StyleCiurea, Andreea, Alina Stanomir, Petra Șurlin, Iulia Cristina Micu, Cristina Pamfil, Daniel Corneliu Leucuța, Simona Rednic, Giulio Rasperini, Andrada Soancă, Adrian Bogdan Țigu, and et al. 2024. "Insights into the Relationship between Periodontitis and Systemic Sclerosis Based on the New Periodontitis Classification (2018): A Cross-Sectional Study" Diagnostics 14, no. 5: 540. https://doi.org/10.3390/diagnostics14050540
APA StyleCiurea, A., Stanomir, A., Șurlin, P., Micu, I. C., Pamfil, C., Leucuța, D. C., Rednic, S., Rasperini, G., Soancă, A., Țigu, A. B., Roman, A., Picoș, A., & Delean, A. G. (2024). Insights into the Relationship between Periodontitis and Systemic Sclerosis Based on the New Periodontitis Classification (2018): A Cross-Sectional Study. Diagnostics, 14(5), 540. https://doi.org/10.3390/diagnostics14050540