The Double Life-Saving Approach of Abdominal Radical Trachelectomy during Pregnancy for Early-Stage Cervical Cancer—An Overview of the Literature and Our Institutional Experience
Abstract
:1. Introduction
2. Materials and Methods
3. Results
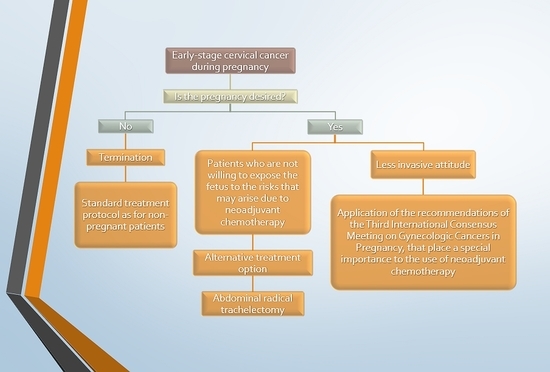
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Bray, F.; Ferlay, J.; Soerjomataram, I.; Siegel, R.L.; Torre, L.A.; Jemal, A. Global cancer statistics 2018: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J. Clin. 2018, 68, 394–424. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Demeter, A.; Sziller, I.; Csapó, Z.; Szánthó, A.; Papp, Z. Outcome of pregnancies after cold-knife conization of the uterine cervix during pregnancy. Eur. J. Gynaecol. Oncol. 2002, 23, 207–210. Available online: https://www.ncbi.nlm.nih.gov/pubmed/12094956 (accessed on 26 April 2020). [PubMed]
- Nicol, A.F.; de Andrade, C.V.; Brusadelli, M.G.; Lodin, H.M.; Wells, S.I.; Nuovo, G.J. The distribution of novel biomarkers in carcinoma-in-situ, microinvasive, and squamous cell carcinoma of the uterine cervix. Ann. Diagn. Pathol. 2019, 38, 115–122. [Google Scholar] [CrossRef] [PubMed]
- Vitale, S.G.; Valenti, G.; Rapisarda, A.M.C.; Cali, I.; Marilli, I.; Zigarelli, M.; Sarpietro, G.; Cianci, A. P16INK4a as a progression/regression tumour marker in LSIL cervix lesions: Our clinical experience. Eur. J. Gynaecol. Oncol. 2016, 37, 685–688. [Google Scholar] [PubMed]
- Ramirez, P.T.; Schmeler, K.M.; Soliman, P.T.; Frumovitz, M. Fertility preservation in patients with early cervical cancer: Radical trachelectomy. Gynecol. Oncol. 2008, 110, S25–S28. [Google Scholar] [CrossRef]
- Amant, F.; Berveiller, P.; Boere, I.A.; Cardonick, E.; Fruscio, R.; Fumagalli, M.; Halaska, M.J.; Hasenburg, A.; Johansson, A.L.; Lambertini, M.; et al. Gynecologic cancers in pregnancy: Guidelines based on a third international consensus meeting. Ann. Oncol. 2019, 30, 1601–1612. [Google Scholar] [CrossRef] [Green Version]
- Ungár, L.; Pálfalvi, L.; Hogg, R.; Siklós, P.; Boyle, D.C.; Del Priore, G.; Smith, J.R. Abdominal radical trachelectomy: A fertility-preserving option for women with early cervical cancer. BJOG Int. J. Obstet. Gynaecol. 2005, 112, 366–369. [Google Scholar] [CrossRef]
- Smith, J.R.; Boyle, D.C.M.; Corless, D.J.; Ungar, L.; Lawson, A.D.; Priore, G.D.; McCall, J.M.; Lindsay, I.; Bridges, J.E. Abdominal radical trachelectomy: A new surgical technique for the conservative management of cervical carcinoma. BJOG Int. J. Obstet. Gynaecol. 1997, 104, 1196–1200. [Google Scholar] [CrossRef] [Green Version]
- Aburel, E. Erweiterte abdominelle Exstirpation der Cervix und des Isthmus in den Anfangsstadien des Collumearcinoms (Carcinoma in situ und Mikrocarcinom). Arch. für Gynäkologie 1973, 214, 106–108. [Google Scholar] [CrossRef]
- Ungár, L.; Smith, J.R.; Pálfalvi, L.; Del Priore, G. Abdominal radical trachelectomy during pregnancy to preserve pregnancy and fertility. Obstet. Gynecol. 2006, 108, 811–814. [Google Scholar] [CrossRef]
- Mandic, A.; Novakovic, P.; Nincic, D.; Zivaljevic, M.; Rajovic, J. Radical abdominal trachelectomy in the 19th gestation week in patients with early invasive cervical carcinoma: Case study and overview of literature. Am. J. Obstet. Gynecol. 2009, 201, e6–e8. [Google Scholar] [CrossRef] [PubMed]
- Yi, X.; Ding, J.; Zhang, Y.; Liu, X.; Cheng, H.; Li, X.; Zhou, X.; Hua, K. Laparoscopic radical trachelectomy followed by chemotherapy in a pregnant patient with invasive cervical cancer. Int. J. Gynecol. Obstet. 2015, 131, 101–102. [Google Scholar] [CrossRef] [PubMed]
- Abu-Rustum, N.R.; Tal, M.N.; DeLair, D.; Shih, K.; Sonoda, Y. Radical abdominal trachelectomy for stage IB1 cervical cancer at 15-week gestation. Gynecol. Oncol. 2010, 116, 151–152. [Google Scholar] [CrossRef] [PubMed]
- Karateke, A.; Cam, C.; Celik, C.; Baykal, B.; Tug, N.; Ozbasli, E.; Tosun, O.A. Radical trachelectomy in late pregnancy: Is it an option? Eur. J. Obstet. Gynecol. Reprod. Biol. 2010, 152, 112–113. [Google Scholar] [CrossRef]
- Enomoto, T.; Yoshino, K.; Fujita, M.; Miyoshi, Y.; Ueda, Y.; Koyama, S.; Kimura, T.; Tomimatsu, T.; Kimura, T. A successful case of abdominal radical trachelectomy for cervical cancer during pregnancy. Eur. J. Obstet. Gynecol. Reprod. Biol. 2011, 158, 365–366. [Google Scholar] [CrossRef]
- Aoki, Y.; Inamine, M.; Ohishi, S.; Nagai, Y.; Masamoto, H. Radical abdominal trachelectomy for IB1 cervical cancer at 17 weeks of gestation: A case report and literature review. Case Rep. Obstet. Gynecol. 2014, 2014, 1–4. [Google Scholar] [CrossRef] [Green Version]
- Căpîlna, M.E.; Szabo, B.; Rusu, S.C.; Becsi, J.; Szasz, F.C.; Morariu, M.; Moldovan, B.; Pascanu, I.M. Abdominal radical trachelectomy (ART) performed during pregnancy: A case report. Eur. J. Gynaecol. Oncol. 2017, 38, 129–131. [Google Scholar] [CrossRef]
- Rodolakis, A.; Thomakos, N.; Sotiropoulou, M.; Kypriotis, K.; Valsamidis, D.; Bourgioti, C.; Moulopoulou, L.E.; Vlachos, G.; Loutradis, D. Abdominal radical trachelectomy for early-stage cervical cancer during pregnancy: A provocative surgical approach. Overview of the literature and a single-institute experience. Int. J. Gynecol. Cancer 2018, 28, 1743–1750. [Google Scholar] [CrossRef]
- Yoshihara, K.; Ishiguro, T.; Chihara, M.; Shima, E.; Adachi, S.; Isobe, M.; Haino, K.; Yamaguchi, M.; Sekine, M.; Kashima, K.; et al. The safety and effectiveness of abdominal radical trachelectomy for early-stage cervical cancer during pregnancy. Int. J. Gynecol. Cancer 2018, 28, 782–787. [Google Scholar] [CrossRef] [Green Version]
- Kyrgiou, M.; Horwell, D.H.; Farthing, A. Laparoscopic radical abdominal trachelectomy for the management of stage IB1 cervical cancer at 14 weeks’ gestation: Case report and review of the literature. BJOG Int. J. Obstet. Gynaecol. 2015, 122, 1138–1143. [Google Scholar] [CrossRef] [Green Version]
- Creasman, W.T. Cancer and pregnancy. Ann. N. Y. Acad. Sci. 2001, 943, 281–286. [Google Scholar] [CrossRef] [PubMed]
- Sonoda, Y. A new indication for trachelectomy. BJOG Int. J. Obstet. Gynaecol. 2015, 122, 1144. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Căpîlna, M.E.; Moldovan, B.; Szabo, B. Pelvic exenteration—Our initial experience in 15 cases. Eur. J. Gynaecol. Oncol. 2015, 36, 142–145. [Google Scholar] [PubMed]
- de Haan, J.; Verheecke, M.; Van Calsteren, K.; Van Calster, B.; Shmakov, R.G.; Gziri, M.M.; Halaska, M.J.; Fruscio, R.; Lok, C.A.; Boere, I.A.; et al. Oncological management and obstetric and neonatal outcomes for women diagnosed with cancer during pregnancy: A 20-year international cohort study of 1170 patients. Lancet Oncol. 2018, 19, 337–346. [Google Scholar] [CrossRef]
- Amant, F.; Vandenbroucke, T.; Verheecke, M.; Fumagalli, M.; Halaska, M.J.; Boere, I.; Han, S.; Gziri, M.M.; Peccatori, F.; Rob, L.; et al. Pediatric outcome after maternal cancer diagnosed during pregnancy. N. Engl. J. Med. 2015, 373, 1824–1834. [Google Scholar] [CrossRef]
- Amant, F.; Van Calsteren, K.; Halaska, M.J.; Gziri, M.M.; Hui, W.; Lagae, L.; Willemsen, M.A.; Kapusta, L.; Van Calster, B.; Wouters, H.; et al. Long-term cognitive and cardiac outcomes after prenatal exposure to chemotherapy in children aged 18 months or older: An observational study. Lancet Oncol. 2012, 13, 256–264. [Google Scholar] [CrossRef]
- Maggen, C.; Wolters, V.E.; Cardonick, E.; Fumagalli, M.; Halaska, M.J.; Lok, C.A.; de Haan, J.; Van Tornout, K.; Van Calsteren, K.; Amant, F. Pregnancy and cancer: The INCIP project. Curr. Oncol. Rep. 2020, 22, 1–10. [Google Scholar] [CrossRef] [Green Version]
- Geijteman, E.C.T.; Wensveen, C.W.M.; Duvekot, J.J.; Van Zuylen, L. A child with severe hearing loss associated with maternal cisplatin treatment during pregnancy. Obstet. Gynecol. 2014, 124, 454–456. [Google Scholar] [CrossRef]
- Song, Y.; Liu, Y.; Lin, M.; Sheng, B.; Zhu, X. Efficacy of neoadjuvant platinum-based chemotherapy during the second and third trimester of pregnancy in women with cervical cancer: An updated systematic review and meta-analysis. Drug Des. Dev. Ther. 2019, 13, 79–102. [Google Scholar] [CrossRef] [Green Version]
- Maggen, C.; Dierickx, D.; Lugtenburg, P.; Laenen, A.; Cardonick, E.; Smakov, R.G.; Bellido, M.; Cabrera-Garcia, A.; Gziri, M.M.; Halaska, M.J.; et al. Obstetric and maternal outcomes in patients diagnosed with Hodgkin lymphoma during pregnancy: A multicentre, retrospective, cohort study. Lancet Haematol. 2019, 6, e551–e561. [Google Scholar] [CrossRef]
- Cao, D.Y.; Yang, J.X.; Wu, X.H.; Chen, Y.L.; Li, L.; Liu, K.J.; Cui, M.H.; Xie, X.; Wu, Y.M.; Kong, B.H.; et al. Comparisons of vaginal and abdominal radical trachelectomy for early-stage cervical cancer: Preliminary results of a multi-center research in China. Br. J. Cancer 2013, 109, 2778–2782. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Chiva, L.; Zanagnolo, V.; Querleu, D.; Martin-Calvo, N.; Arévalo-Serrano, J.; Căpîlna, M.E.; Fagotti, A.; Kucukmetin, A.; Mom, C.; Chakalova, G.; et al. SUCCOR study: An international European cohort observational study comparing minimally invasive surgery versus open abdominal radical hysterectomy in patients with stage IB1 cervical cancer. Int. J. Gynecol. Cancer 2020. [Google Scholar] [CrossRef] [PubMed]
- Salvo, G.; Ramirez, P.T.; Leitao, M.; Cibula, D.; Fotopoulou, C.; Kucukmetin, A.; Rendon, G.; Perrotta, M.; Ribeiro, R.; Vieira, M.; et al. International radical trachelectomy assessment: IRTA study. Int. J. Gynecol. Cancer 2019, 29, 635–638. [Google Scholar] [CrossRef] [PubMed]
- Căpîlna, M.E.; Szabo, B.; Becsi, J.; Ioanid, N.; Moldovan, B. Radical trachelectomy performed during pregnancy: A review of the literature. Int. J. Gynecol. Cancer 2016, 26, 758–762. [Google Scholar] [CrossRef]
- Amant, F.; Halaska, M.J.; Fumagalli, M.; Steffensen, K.D.; Lok, C.; Van Calsteren, K.; Han, S.N.; Mir, O.; Fruscio, R.; Uzan, C.; et al. Gynecologic cancers in pregnancy: Guidelines of a second international consensus meeting. Int. J. Gynecol. Cancer 2014, 24, 394–403. [Google Scholar] [CrossRef]
- Douligeris, A.; Prodromidou, A.; Psomiadou, V.; Iavazzo, C.; Vorgias, G. Abdominal radical trachelectomy during pregnancy: A systematic review of the literature. J. Gynecol. Obstet. Hum. Reprod. 2020, 49, 101607. [Google Scholar] [CrossRef]
- Gizzo, S.; Ancona, E.; Saccardi, C.; Patrelli, T.S.; Berretta, R.; Anis, O.; Noventa, M.; Bertocco, A.; Fagherazzi, S.; Longone, M.; et al. Radical trachelectomy: The first step of fertility preservation in young women with cervical cancer (Review). Oncol. Rep. 2013, 30, 2545–2554. [Google Scholar] [CrossRef]
- Okugawa, K.; Kobayashi, H.; Sonoda, K.; Kaneki, E.; Kawano, Y.; Hidaka, N.; Egashira, K.; Fujita, Y.; Yahata, H.; Kato, K. Oncologic and obstetric outcomes and complications during pregnancy after fertility-sparing abdominal trachelectomy for cervical cancer: A retrospective review. Int. J. Clin. Oncol. 2017, 22, 340–346. [Google Scholar] [CrossRef]
- Kasuga, Y.; Miyakoshi, K.; Nishio, H.; Akiba, Y.; Otani, T.; Fukutake, M.; Ikenoue, S.; Ochiai, D.; Matsumoto, T.; Tanaka, K.; et al. Mid-trimester residual cervical length and the risk of preterm birth in pregnancies after abdominal radical trachelectomy: A retrospective analysis. BJOG Int. J. Obstet. Gynaecol. 2017, 124, 1729–1735. [Google Scholar] [CrossRef] [Green Version]
- Park, K.J.; Soslow, R.A.; Sonoda, Y.; Barakat, R.R.; Abu-Rustum, N.R. Frozen-section evaluation of cervical adenocarcinoma at time of radical trachelectomy: Pathologic pitfalls and the application of an objective scoring system. Gynecol. Oncol. 2008, 110, 316–323. [Google Scholar] [CrossRef] [Green Version]
- Cǎpîlna, M.E.; Szabo, B.; Rusu, S.C.; Becsi, J.; Moldovan, B.; Neagoe, R.M.; Muhlfay, G. Anatomical variations of the obturator veins and their surgical implications. Eur. J. Gynaecol. Oncol. 2017, 38, 263–265. [Google Scholar] [PubMed]

| Publication | Gestational Age at Surgery, wk. | Stage | Histology | Status of Uterine Arteries | Duration of Surgery | Estimated Blood Loss, mL | Pregnancy Outcome, wk. | Neonatal Outcome | Oncological Outcome |
|---|---|---|---|---|---|---|---|---|---|
| Abdominal Radical Trachelectomy | |||||||||
| Ungar et al., 2006 [10] | 7 | IB1 | SCC | Both preserved | NR | NR | Mis.—1st wk. after surgery | - | NED |
| Ungar et al., 2006 [10] | 8 | IB1 | SCC | Both preserved | NR | NR | Mis.—1st wk. after surgery | - | NED |
| Ungar et al., 2006 [10] | 9 | IB1 | SCC | Both preserved | NR | NR | 38 wk. | Good | NED |
| Ungar et al., 2006 [10] | 13 | IB1 | SCC | Both preserved | NR | NR | Mis.—3rd wk. after surgery | - | NED |
| Ungar et al., 2006 [10] | 18 | IB1 | SCC | Both preserved | NR | NR | 39 wk. | Good | NED |
| Mandic et al., 2009 [11] | 19 | IB1 | SCC | NR | 5 h | 450 | 36 wk. (PROM) | Good | NED |
| Abu-Rustum et al., 2009 [13] | 15 | IB1 | Lymphoepithelial | Left ligature | 3.5 h | 1600 | 39 wk. | Good | NR |
| Karateke et al., 2010 [14] | 22 | IB2 | SCC | Bilateral ligature | 4 h | 200 | Mis.—fetal death a few hours after surgery | - | NR |
| Enomoto et al., 2011 [15] | 15 | IB1 | SCC | Right ligature | 7.5 h | 960 | 37 wk. | Good | NED |
| Aoki et al., 2014 [16] | 17 | IB1 | SCC | Both preserved | 6 h | 2510 | 38 wk. | Good | NED |
| Căpîlna et al., 2015 [17] | 17 | IB2 | SCC | Left ligature | 6 h | 500 | 38 wk. | Good | NED |
| Căpîlna et al., 2016 | 15 | IB3 | SCC | Both preserved | 5.5 h | 800 | Mis.—2nd wk. after surgery (PPROM) | - | NED |
| Căpîlna et al., 2016 | 15 | IB3 | SCC | Both preserved | 6 h | 500 | Mis.—2nd wk. after surgery (PPROM) | - | NED (CRT following surgery) |
| Căpîlna et al., 2016 | 17 | IB2 | SCC | Left ligature | 5 h | 500 | 39 wk. | Good | NED |
| Căpîlna et al., 2019 | 32 (C-section + ART) | IB3 | SCC | Both ligation | 5 h | 900 | 32 wk. | Good | NED |
| Rodolakis et al., 2018 [18] | 14 | IB1 | SCC | Both preserved | 4.5 h | 1800 | 36 wk. | Good | NED |
| Rodolakis et al., 2018 [18] | 14 | IB1 | SCC | Both preserved | 4 h | 2000 | 32 wk. | Good | NED |
| Yoshihara et al., 2018 [19] | 15 | IB1 | SCC | Both preserved | 8.5 h | 1275 | 33 wk. (PROM) | Good | NED (CT following surgery) |
| Yoshihara et al., 2018 [19] | 17 | IB1 | SCC | Left ligature | 6.5 h | 600 | 37 wk. | Good | NED |
| Yoshihara et al., 2018 [19] | 15 | IB1 | SCC | Both preserved | 6 h | 1270 | 30 wk. | Good | NED (CT following surgery) |
| Yoshihara et al., 2018 [19] | 15 | IB1 | SCC | Bilateral ligature | 5 h | 935 | 33 wk. | Good | NED (CT following surgery) |
| Yoshihara et al., 2018 [19] | 15 | IB1 | AC | Both preserved | 5.5 h | 1415 | 37 wk. | Good | NED |
| Yoshihara et al., 2018 [19] | 17 | IB1 | SCC | Left ligature | 6.5 h | 2010 | 31 wk. | Good | NED (CT following surgery) |
| Laparoscopic Abdominal Radical Trachelectomy | |||||||||
| Kyrgiou et al., 2015 [20] | 14 | IB1 | AC | Both preserved | 4 h | 200 | 36 wk. | Good | NED |
| Yi et al., 2015 [12] | 18 | IB1 | Papillary mucinous AC | N/A | N/A | N/A | 34 wk. | Good | N/A |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Stanca, M.; Ciobanu, V.; Gheorghe, M.; Kiss, S.L.; Cozlea, A.L.; Căpîlna, M.E. The Double Life-Saving Approach of Abdominal Radical Trachelectomy during Pregnancy for Early-Stage Cervical Cancer—An Overview of the Literature and Our Institutional Experience. J. Pers. Med. 2021, 11, 29. https://doi.org/10.3390/jpm11010029
Stanca M, Ciobanu V, Gheorghe M, Kiss SL, Cozlea AL, Căpîlna ME. The Double Life-Saving Approach of Abdominal Radical Trachelectomy during Pregnancy for Early-Stage Cervical Cancer—An Overview of the Literature and Our Institutional Experience. Journal of Personalized Medicine. 2021; 11(1):29. https://doi.org/10.3390/jpm11010029
Chicago/Turabian StyleStanca, Mihai, Victoria Ciobanu, Mihai Gheorghe, Szilard Leo Kiss, Alexandra Lavinia Cozlea, and Mihai Emil Căpîlna. 2021. "The Double Life-Saving Approach of Abdominal Radical Trachelectomy during Pregnancy for Early-Stage Cervical Cancer—An Overview of the Literature and Our Institutional Experience" Journal of Personalized Medicine 11, no. 1: 29. https://doi.org/10.3390/jpm11010029
APA StyleStanca, M., Ciobanu, V., Gheorghe, M., Kiss, S. L., Cozlea, A. L., & Căpîlna, M. E. (2021). The Double Life-Saving Approach of Abdominal Radical Trachelectomy during Pregnancy for Early-Stage Cervical Cancer—An Overview of the Literature and Our Institutional Experience. Journal of Personalized Medicine, 11(1), 29. https://doi.org/10.3390/jpm11010029