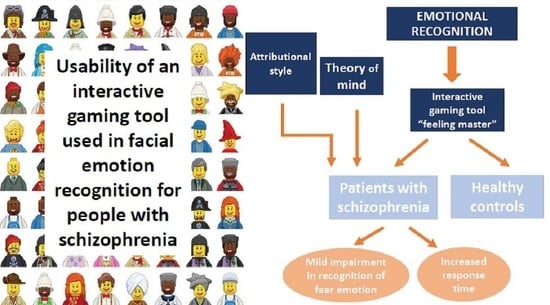
Usability of a Psychotherapeutic Interactive Gaming Tool Used in Facial Emotion Recognition for People with Schizophrenia
Abstract
:1. Introduction
1.1. Impairment in Emotion Recognition in Schizophrenia
1.2. Relation between Emotional Recognition and Other Variables (Clinical and Social)
1.3. Assessment of Emotional Recognition
1.4. Informatics Application Tools for the Assessment
2. Materials and Methods
2.1. Designing Facial Expressions Using Cartoon Techniques and ‘Feeling Master’ Program
2.2. Content Validity and Reliability
2.3. Adaptability
2.4. Participants
2.5. Ethical Aspects
2.6. Assessment
- -
- Personal and Situational Attribution Questionnaire (IPSAQ) assesses the attributional style [40]. The IPSAQ consists of 32 items and each item describes positive and negative social situations. For each item, the participants are requested to identify the most likely cause of the event and then indicate whether that cause was attributed to oneself (internal attributions), other people (personal attributions), or circumstances (situational attributions). From the scores, it is possible to identify two cognitive biases: the externalizing bias (EB) and the personalizing bias (PB).
- -
- Theory of Mind: (ToM) is assessed using the Hinting Task [41], which consists of five written short stories, including social hints that the participants have to guess and explain. Total scores range from 0 to 10, higher scores indicate a better performance.
- -
- ‘Feeling Master’, an interactive gaming tool used in facial emotion recognition: The interactive software application was used to assess facial emotion recognition (FER). When the application was installed and tested on the tablet, a trained psychologist adapted the number of questions for all of the three levels (seven questions), the highest amount of time per question (12 s), and the emotions needed for the FER evaluation (happiness, sadness, anger, fear, and surprise) (Figure 2).
2.7. Statistical Analysis
3. Results
3.1. Convergent Validity of the ‘Feeling Master’
3.2. Acceptability and Usability
3.3. Accuracy
3.4. Response Time
3.5. Relationship between the Emotion Recognition Performance and IPSAQ and ToM
4. Discussion
4.1. Tool Design
4.2. Impairment in Emotional Recognition
4.3. Relation between Emotional Recognition, Attribution Style, and ToM
4.4. Future Work
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Green, M.F.; Penn, D.L.; Bentall, R.; Carpenter, W.T.; Gaebel, W.; Gur, R.C.; Kring, A.M.; Park, S.; Silverstein, S.M.; Heinssen, R.; et al. Social Cognition in Schizophrenia: An NIMH Workshop on Definitions, Assessment, and Research Opportunities. Schizophr. Bull. 2008, 34, 1211–1220. [Google Scholar] [CrossRef] [Green Version]
- Tan, B.-L.; Lee, S.-A.; Lee, J. Social cognitive interventions for people with schizophrenia: A systematic review. Asian J. Psychiatry 2018, 35, 115–131. [Google Scholar] [CrossRef] [Green Version]
- Buck, B.E.; Healey, K.M.; Gagen, E.C.; Roberts, D.L.; Penn, D.L. Social cognition in schizophrenia: Factor structure, clinical and functional correlates. J. Ment. Heal. 2016, 25, 330–337. [Google Scholar] [CrossRef]
- Harvey, P.D.; Penn, D. Social cognition: The key factor predicting social outcome in people with schizophrenia? Psychiatry 2010, 7, 41–44. Available online: http://www.ncbi.nlm.nih.gov/pubmed/20376275 (accessed on 16 March 2021). [PubMed]
- Kurtz, M.M.; Richardson, C.L. Social Cognitive Training for Schizophrenia: A Meta-Analytic Investigation of Controlled Research. Schizophr. Bull. 2011, 38, 1092–1104. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Green, M.F.; Horan, W.P.; Lee, J. Social cognition in schizophrenia. Nat. Rev. Neurosci. 2015, 16, 620–631. Available online: http://www.ncbi.nlm.nih.gov/pubmed/26373471 (accessed on 16 March 2021). [CrossRef] [PubMed]
- Kirkpatrick, B.; Buchanan, R.W.; McKenny, P.D.; Alphs, L.D.; Carpenter, W.T. The schedule for the deficit syndrome: An instrument for research in schizophrenia. Psychiatry Res. 1989, 30, 119–123. [Google Scholar] [CrossRef]
- Mueser, K.T.; Doonan, R.; Penn, D.L.; Blanchard, J.J.; Bellack, A.S.; Nishith, P.; de Leon, J. Emotion recognition and social competence in chronic schizophrenia. J. Abnorm. Psychol. 1996, 105, 271–275. Available online: http://www.ncbi.nlm.nih.gov/pubmed/8723008 (accessed on 16 March 2021). [CrossRef]
- Addington, J.; Addington, D. Facial affect recognition and information processing in schizophrenia and bipolar disorder. Schizophr. Res. 1998, 32, 171–181. [Google Scholar] [CrossRef]
- Bryson, G.; Bell, M.; Kaplan, E.; Greig, T.; Lysaker, P. Affect recognition in deficit syndrome schizophrenia. Psychiatry Res. 1998, 77, 113–120. [Google Scholar] [CrossRef]
- Davis, P.J.; Gibson, M.G. Recognition of posed and genuine facial expressions of emotion in paranoid and nonparanoid schizophrenia. J. Abnorm. Psychol. 2000, 109, 445–450. Available online: http://www.ncbi.nlm.nih.gov/pubmed/11016114 (accessed on 16 March 2021). [CrossRef] [PubMed]
- Kohler, C.G.; Bilker, W.; Hagendoorn, M.; Gur, R.E.; Gur, R.C. Emotion recognition deficit in schizophrenia: Association with symptomatology and cognition. Biol. Psychiatry 2000, 48, 127–136. [Google Scholar] [CrossRef]
- Penn, D.L.; Combs, D.R.; Ritchie, M.; Francis, J.; Cassisi, J.; Morris, S.; Townsend, M. Emotion recognition in schizophrenia: Further investigation of generalized versus specific deficit models. J. Abnorm. Psychol. 2000, 109, 512–516. Available online: http://www.ncbi.nlm.nih.gov/pubmed/11016120 (accessed on 16 March 2021). [CrossRef] [PubMed]
- Edwards, J.; Jackson, H.J.; Pattison, P.E. Erratum to “Emotion recognition via facial expression and affective prosody in schizophrenia: A methodological review.” [Clinical Psychology Review 22 (2002) 789–832]. Clin. Psychol. Rev. 2002, 22, 1267–1285. [Google Scholar] [CrossRef]
- Van’t Wout, M.; van Dijke, A.; Aleman, A.; Kessels, R.P.C.; Pijpers, W.; Kahn, R.S. Fearful faces in schizophrenia: The relationship between patient characteristics and facial affect recognition. J. Nerv. Ment. Dis. 2007, 195, 758–764. Available online: https://pubmed.ncbi.nlm.nih.gov/17984776/ (accessed on 16 March 2021). [CrossRef]
- Leppänen, J.; Niehaus, D.; Koen, L.; du Toit, E.; Schoeman, R.; Emsley, R. Emotional face processing deficit in schizophrenia: A replication study in a South African Xhosa population. Schizophr. Res. 2006, 84, 323–330. [Google Scholar] [CrossRef]
- Song, Y.; Xiang, Y.-T.; Huang, Y.; Wang, X.; Wang, X.; Zhang, F.; Kwan, J.S.H.; Chan, O.C.; Wang, Z.; Ungvari, G.S.; et al. Impairments in Negative Facial Emotion Recognition in Chinese Schizophrenia Patients Detected with a Newly Designed Task. J. Nerv. Ment. Dis. 2015, 203, 718–724. [Google Scholar] [CrossRef]
- Weniger, G.; Lange, C.; Rüther, E.; Irle, E. Differential impairments of facial affect recognition in schizophrenia subtypes and major depression. Psychiatry Res. 2004, 128, 135–146. [Google Scholar] [CrossRef]
- Schneider, F.; Gur, R.C.; Gur, R.E.; Shtasel, D.L. Emotional processing in schizophrenia: Neurobehavioral probes in relation to psychopathology. Schizophr. Res. 1995, 17, 67–75. [Google Scholar] [CrossRef]
- Hall, J.; Harris, J.M.; Sprengelmeyer, R.; Sprengelmeyer, A.; Young, A.W.; Santos, I.M.; Johnstone, E.C.; Lawrie, S.M. Social cognition and face processing in schizophrenia. Br. J. Psychiatry 2004, 185, 169–170. [Google Scholar] [CrossRef] [Green Version]
- Couture, S.M.; Penn, D.L.; Roberts, D.L. The Functional Significance of Social Cognition in Schizophrenia: A Review. Schizophr. Bull. 2006, 32, S44–S63. [Google Scholar] [CrossRef] [Green Version]
- Mayer, J.D.; Salovey, P.; Caruso, D.R.; Sitarenios, G. Measuring emotional intelligence with the MSCEIT V2.0. Emotion 2003, 3, 97–105. [Google Scholar] [CrossRef] [Green Version]
- Cassé-Perrot, C.; Fakra, E.; Jouve, E.; Blin, O. Conceptualisation and validation of the “Emotional State Questionnaire (ESQ)”: Evaluation of an emotional profile. L’Encéphale 2007, 33, 169–178. [Google Scholar] [CrossRef]
- Scherer, K.R.; Scherer, U. Assessing the ability to recognize facial and vocal expressions of emotion. Construction and validation of the Emotion Recognition Index (ERI). J. Nonverbal. Behav. 2011, 35, 305–326. [Google Scholar] [CrossRef] [Green Version]
- Kaltenthaler, E.; Cavanagh, K. Computerised cognitive behavioural therapy and its uses. Prog. Neurol. Psychiatry 2010, 14, 22–29. [Google Scholar] [CrossRef]
- Kaltenthaler, E.; Parry, G.; Beverley, C. Computerized Cognitive Behaviour Therapy: A Systematic Review. Behav. Cogn. Psychother. 2004, 32, 31–55. [Google Scholar] [CrossRef]
- Newman, M.G.; Szkodny, L.E.; Llera, S.J.; Przeworski, A. A review of technology-assisted self-help and minimal contact therapies for drug and alcohol abuse and smoking addiction: Is human contact necessary for therapeutic efficacy? Clin. Psychol. Rev. 2011, 31, 178–186. [Google Scholar] [CrossRef] [PubMed]
- Taylor, C.B.; Luce, K.H. Computer- and Internet-Based Psychotherapy Interventions. Curr. Dir. Psychol. Sci. 2003, 12, 18–22. [Google Scholar] [CrossRef]
- Miller, B.J.; Stewart, A.; Schrimsher, J.; Peeples, D.; Buckley, P.F. How connected are people with schizophrenia? Cell phone, computer, email, and social media use. Psychiatry Res. 2015, 225, 458–463. [Google Scholar] [CrossRef]
- Goh, D.H.; Ang, R.P.; Tan, H.C. Strategies for designing effective psychotherapeutic gaming interventions for children and adolescents. Comput. Hum. Behav. 2008, 24, 2217–2235. [Google Scholar] [CrossRef]
- Van der Geest, J.N.; Kemner, C.; Camfferman, G.; Verbaten, M.N.; van Engeland, H. Looking at images with human figures: Comparison between autistic and normal children. J. Autism. Dev. Disord. 2002, 32, 69–75. Available online: http://www.ncbi.nlm.nih.gov/pubmed/12058845 (accessed on 16 March 2021). [CrossRef] [PubMed]
- Miyahara, M.; Bray, A.; Tsujii, M.; Fujita, C.; Sugiyama, T. Reaction Time of Facial Affect Recognition in Asperger’s Disorder for Cartoon and Real, Static and Moving Faces. Child Psychiatry Hum. Dev. 2007, 38, 121–134. [Google Scholar] [CrossRef] [PubMed]
- Grelotti, D.J.; Klin, A.J.; Gauthier, I.; Skudlarski, P.; Cohen, D.J.; Gore, J.C.; Volkmar, F.R.; Schultz, R.T. fMRI activation of the fusiform gyrus and amygdala to cartoon characters but not to faces in a boy with autism. Neuropsychologia 2005, 43, 373–385. [Google Scholar] [CrossRef]
- Silver, M.; Oakes, P. Evaluation of a new computer intervention to teach people with autism or Asperger syndrome to recognize and predict emotions in others. Autism 2001, 5, 299–316. [Google Scholar] [CrossRef]
- Xu, Z.; John, D.; Boucouvalas, A. Expressive image generation: Towards expressive Internet communications. J. Vis. Lang. Comput. 2006, 17, 445–465. [Google Scholar] [CrossRef]
- Tsalakanidou, F.; Malassiotis, S. Real-time 2D+3D facial action and expression recognition. Pattern Recognit. 2010, 43, 1763–1775. [Google Scholar] [CrossRef]
- Ekman, P.; Friedsen, W.V. Consulting Psychologists; Consulting Psychologists Press: Palo Alto, CA, USA, 1976. [Google Scholar]
- Parke, F.I.; Waters, K. Computer Facial Animation; CRC Press: Boca Raton, CA, USA, 1996. [Google Scholar]
- Wechsler, D. WAIS-IV, Escala de Inteligencia de Wechsler para Adultos-IV. Manual Técnico y de Interpretación; Pearson: Madrid, Spain, 2012. [Google Scholar]
- Kinderman, P.; Bentall, R.P. Self-discrepancies and persecutory delusions: Evidence for a model of paranoid ideation. J. Abnorm. Psychol. 1996, 105, 106–113. Available online: http://www.ncbi.nlm.nih.gov/pubmed/8666699 (accessed on 16 March 2021). [CrossRef]
- Frith, C.D.; Corcoran, R. Exploring “theory of mind” in people with schizophrenia. Psychol. Med. 1996, 26, 521–530. Available online: http://www.ncbi.nlm.nih.gov/pubmed/8733211 (accessed on 16 March 2021). [CrossRef] [PubMed]
- Kring, A.M.; Kerr, S.L.; Earnst, K.S. Schizophrenic patients show facial reactions to emotional facial expressions. Psychophysiology 1999, 36, 186–192. Available online: http://www.ncbi.nlm.nih.gov/pubmed/10194965 (accessed on 16 March 2021). [CrossRef] [PubMed]
- Gabay, A.S.; Kempton, M.J.; Mehta, M.A. Facial affect processing deficits in schizophrenia: A meta-analysis of antipsychotic treatment effects. J. Psychopharmacol. 2014, 29, 224–229. [Google Scholar] [CrossRef] [Green Version]
- Lally, J.; MacCabe, J.H. Antipsychotic medication in schizophrenia: A review. Br. Med Bull. 2015, 114, 169–179. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Romero-Ferreiro, M.V.; Aguado, L.; Rodriguez-Torresano, J.; Palomo, T.; Rodriguez-Jimenez, R.; Pedreira-Massa, J.L. Facial affect recognition in early and late-stage schizophrenia patients. Schizophr. Res. 2016, 172, 177–183. [Google Scholar] [CrossRef] [PubMed]
- Kohler, C.G.; Turner, T.H.; Bilker, W.B.; Brensinger, C.M.; Siegel, S.J.; Kanes, S.J.; Gur, R.E.; Gur, R.C. Facial Emotion Recognition in Schizophrenia: Intensity Effects and Error Pattern. Am. J. Psychiatry 2003, 160, 1768–1774. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Adolphs, R. Recognizing Emotion from Facial Expressions: Psychological and Neurological Mechanisms. Behav. Cogn. Neurosci. Rev. 2002, 1, 21–62. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Trémeau, F.; Antonius, D.; Todorov, A.; Rebani, Y.; Ferrari, K.; Lee, S.H.; Calderone, D.; Nolan, K.A.; Butler, P.D.; Malaspina, D.; et al. Implicit emotion perception in schizophrenia. J. Psychiatr. Res. 2015, 71, 112–119. [Google Scholar] [CrossRef] [PubMed]
- Healey, K.M.; Bartholomeusz, C.F.; Penn, D.L. Deficits in social cognition in first episode psychosis: A review of the literature. Clin. Psychol. Rev. 2016, 50, 108–137. [Google Scholar] [CrossRef]
- Langdon, R.; Coltheart, M.; Ward, P.B. Empathetic perspective-taking is impaired in schizophrenia: Evidence from a study of emotion attribution and theory of mind. Cogn. Neuropsychiatry 2006, 11, 133–155. [Google Scholar] [CrossRef]
- Maat, A.; van Haren, N.E.M.; Bartholomeusz, C.F.; Kahn, R.S.; Cahn, W. Emotion recognition and theory of mind are related to gray matter volume of the prefrontal cortex in schizophrenia. Eur. Neuropsychopharmacol. 2016, 26, 255–264. Available online: http://linkinghub.elsevier.com/retrieve/pii/S0924977X1500396X (accessed on 16 March 2021). [CrossRef] [PubMed]
- Edwards, J.; Pattison, P.E.; Jackson, H.J.; Wales, R.J. Facial affect and affective prosody recognition in first-episode schizophrenia. Schizophr. Res. 2001, 48, 235–253. [Google Scholar] [CrossRef]
- Lewis, S.F.; Garver, D.L. Treatment and diagnostic subtype in facial affect recognition in schizophrenia. J. Psychiatr. Res. 1995, 29, 5–11. [Google Scholar] [CrossRef]
- Gessler, S.; Cutting, J.; Frith, C.D.; Weinman, J. Schizophrenic inability to judge facial emotion: A controlled study. Br. J. Clin. Psychol. 1989, 28, 19–29. [Google Scholar] [CrossRef]
- Mandal, M.K.; Rai, A. Responses to facial emotion and psychopathology. Psychiatry Res. 1987, 20, 317–323. [Google Scholar] [CrossRef]
- Mandal, M.K.; Palchoudhury, S. Identifying the Components of Facial Emotion and Schizophrenia. Psychopathology 1989, 22, 295–300. [Google Scholar] [CrossRef] [PubMed]
- Kirouac, G.; Doré, F.Y. Judgment of Facial Expressions of Emotion as a Function of Exposure Time. Percept. Mot. Ski. 1984, 59, 147–150. [Google Scholar] [CrossRef] [PubMed]
- Ogawa, T.; Suzuki, N. Response differentiation to facial expression of emotion as increasing exposure duration. Percept. Mot. Ski. 1999, 89, 557–563. [Google Scholar]
- Addington, J.; Saeedi, H.; Addington, D. Facial affect recognition: A mediator between cognitive and social functioning in psychosis? Schizophr. Res. 2006, 85, 142–150. [Google Scholar] [CrossRef]
- Proudfoot, J.; Goldberg, D.; Mann, A.; Everitt, B.; Marks, I.; Gray, J.A. Computerized, interactive, multimedia cognitive-behavioural program for anxiety and depression in general practice. Psychol. Med. 2003, 33, 217–227. [Google Scholar] [CrossRef]




| IPSAQ_PB | IPSAQ EB | ToM | |
|---|---|---|---|
| Happy Correlation coefficient Sig. (2-tailed) | −0.076 | 0.061 | 0.106 |
| 0.730 | 0.776 | 0.630 | |
| Angry Correlation coefficient Sig. (2-tailed) | 0.354 | 0.196 | 0.139 |
| 0.115 | 0.383 | 0.547 | |
| Fear Correlation coefficient Sig. (2-tailed) | 0.085 | 0.088 | 0.350 |
| 0.700 | 0.676 | 0.102 | |
| Sad Correlation coefficient Sig. (2-tailed) | 0.252 | −0.162 | 0.261 |
| 0.247 | 0.449 | 0.229 | |
| Surprise Correlation coefficient Sig. (2-tailed) | −0.028 | 0.182 | 0.430 |
| 0.900 | 0.406 | 0.046 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
González, R.P.; Tortadès, I.; Alpiste, F.; Fernandez, J.; Torner, J.; Garcia-Franco, M.; Martin-Martínez, J.R.; Vilamala, S.; Escandell, M.J.; Casas-Anguera, E.; et al. Usability of a Psychotherapeutic Interactive Gaming Tool Used in Facial Emotion Recognition for People with Schizophrenia. J. Pers. Med. 2021, 11, 214. https://doi.org/10.3390/jpm11030214
González RP, Tortadès I, Alpiste F, Fernandez J, Torner J, Garcia-Franco M, Martin-Martínez JR, Vilamala S, Escandell MJ, Casas-Anguera E, et al. Usability of a Psychotherapeutic Interactive Gaming Tool Used in Facial Emotion Recognition for People with Schizophrenia. Journal of Personalized Medicine. 2021; 11(3):214. https://doi.org/10.3390/jpm11030214
Chicago/Turabian StyleGonzález, Roberto Pablo, Ingrid Tortadès, Francesc Alpiste, Joaquín Fernandez, Jordi Torner, Mar Garcia-Franco, José Ramón Martin-Martínez, Sònia Vilamala, Maria Jose Escandell, Emma Casas-Anguera, and et al. 2021. "Usability of a Psychotherapeutic Interactive Gaming Tool Used in Facial Emotion Recognition for People with Schizophrenia" Journal of Personalized Medicine 11, no. 3: 214. https://doi.org/10.3390/jpm11030214
APA StyleGonzález, R. P., Tortadès, I., Alpiste, F., Fernandez, J., Torner, J., Garcia-Franco, M., Martin-Martínez, J. R., Vilamala, S., Escandell, M. J., Casas-Anguera, E., Prat, G., & Ochoa, S. (2021). Usability of a Psychotherapeutic Interactive Gaming Tool Used in Facial Emotion Recognition for People with Schizophrenia. Journal of Personalized Medicine, 11(3), 214. https://doi.org/10.3390/jpm11030214