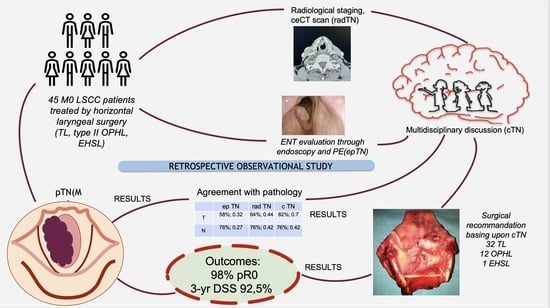
Reliability of a Multidisciplinary Multiparametric Approach in the Surgical Planning of Laryngeal Squamous Cell Carcinomas: A Retrospective Observational Study
Abstract
:1. Introduction
2. Materials and Methods
2.1. Tumor Board Discussion and Treatment Selection
- The staging according to American Joint Committee on Cancer (AJCC);
- Patient-related parameters such as age, comorbidities, and preferences.
2.2. Data Collection
- epTN (based on endoscopy and physical ENT examination);
- radTN based on CT scan;
- cTN (based on multidisciplinary discussion);
- pTN based on pathology on surgical sample.
2.3. Statistical Analysis
3. Results
4. Discussion
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Piotrowski, I.; Zhu, X.; Saccon, T.D.; Ashiqueali, S.; Schneider, A.; de Carvalho Nunes, A.D.; Noureddine, S.; Sobecka, A.; Barczak, W.; Szewczyk, M.; et al. miRNAs as Biomarkers for Diagnosing and Predicting Survival of Head and Neck Squamous Cell Carcinoma Patients. Cancers 2021, 13, 3980. [Google Scholar] [CrossRef] [PubMed]
- Bradley, P.J.; Piazza, C.; Paderno, A. A roadmap of six different pathways to improve survival in laryngeal cancer patients. Curr. Opin. Otolaryngol. Head Neck Surg. 2020, 29, 65–78. [Google Scholar] [CrossRef] [PubMed]
- Sung, H.; Ferlay, J.; Siegel, R.L.; Laversanne, M.; Soerjomataram, I.; Jemal, A.; Bray, F. Global Cancer Statistics 2020: GLOBOCAN Estimates of Incidence and Mortality Worldwide for 36 Cancers in 185 Countries. CA A Cancer J. Clin. 2021, 71, 209–249. [Google Scholar] [CrossRef] [PubMed]
- National Cancer Institute, SEER. Available online: http://seer.cancer.gov/statfacts/html/laryn.html (accessed on 23 August 2022).
- Siegel, R.L.; Miller, K.D.; Fuchs, H.E.; Jemal, A. Cancer Statistics, 2022. CA Cancer J. Clin. 2022, 72, 7–33. [Google Scholar] [CrossRef]
- Forastiere, A.A.; Goepfert, H.; Maor, M.; Pajak, T.F.; Weber, R.; Morrison, W.; Glisson, B.; Trotti, A.; Ridge, J.A.; Chao, C.; et al. Concurrent Chemotherapy and Radiotherapy for Organ Preservation in Advanced Laryngeal Cancer. N. Engl. J. Med. 2003, 349, 2091–2098. [Google Scholar] [CrossRef]
- Department of Veterans Affairs Laryngeal Cancer Study Group; Wolf, G.T.; Fisher, S.G.; Hong, W.K.; Hillman, R.; Spaulding, M.; Laramore, G.E.; Endicott, J.W.; McClatchey, K.; Henderson, W.G. Induction Chemotherapy plus Radiation Compared with Surgery plus Radiation in Patients with Advanced Laryngeal Cancer. N. Engl. J. Med. 1991, 324, 1685–1690. [Google Scholar] [CrossRef]
- Bussu, F.; Miccichè, F.; Rigante, M.; Dinapoli, N.; Parrilla, C.; Bonomo, P.; Cadoni, G.; Mantini, G.; Galli, J.; Rufini, V.; et al. Oncologic Outcomes in Advanced Laryngeal Squamous Cell Carcinomas Treated with Different Modalities in a Single Institution: A Retrospective Analysis of 65 Cases. Head Neck 2012, 34, 573–579. [Google Scholar] [CrossRef]
- De Virgilio, A.; Bussu, F.; De Vincentiis, M. Evidence-Based Review of Treatment Options for Patients with Glottic Cancer. Acta Otorhinolaryngol. Ital. 2012, 32, 256–257. [Google Scholar]
- Dinapoli, N.; Parrilla, C.; Galli, J.; Autorino, R.; Miccichè, F.; Bussu, F.; Balducci, M.; D’Alatri, L.; Marchese, R.; Rigante, M.; et al. Multidisciplinary Approach in the Treatment of T1 Glottic Cancer. The Role of Patient Preference in a Homogenous Patient Population. Strahlenther. Onkol. 2010, 186, 607–613. [Google Scholar] [CrossRef]
- Koroulakis, A.; Agarwal, M. Laryngeal Cancer. In StatPearls; StatPearls Publishing: Treasure Island, FL, USA, 2022. [Google Scholar]
- Hutcheson, K.A.; Lewin, J.S. Functional Outcomes after Chemoradiotherapy of Laryngeal and Pharyngeal Cancers. Curr. Oncol. Rep. 2012, 14, 158–165. [Google Scholar] [CrossRef]
- Cooper, J.S.; Zhang, Q.; Pajak, T.F.; Forastiere, A.A.; Jacobs, J.; Saxman, S.B.; Kish, J.A.; Kim, H.E.; Cmelak, A.J.; Rotman, M.; et al. Long-Term Follow-up of the RTOG 9501/intergroup Phase III Trial: Postoperative Concurrent Radiation Therapy and Chemotherapy in High-Risk Squamous Cell Carcinoma of the Head and Neck. Int. J. Radiat. Oncol. Biol. Phys. 2012, 84, 1198–1205. [Google Scholar] [CrossRef] [Green Version]
- Forastiere, A.A.; Zhang, Q.; Weber, R.S.; Maor, M.H.; Goepfert, H.; Pajak, T.F.; Morrison, W.; Glisson, B.; Trotti, A.; Ridge, J.A.; et al. Long-Term Results of RTOG 91-11: A Comparison of Three Nonsurgical Treatment Strategies to Preserve the Larynx in Patients with Locally Advanced Larynx Cancer. J. Clin. Oncol. 2013, 31, 845–852. [Google Scholar] [CrossRef]
- Silverman, D.A.; Puram, S.V.; Rocco, J.W.; Old, M.O.; Kang, S.Y. Salvage laryngectomy following organ-preservation therapy—An evidence-based review. Oral Oncol. 2018, 88, 137–144. [Google Scholar] [CrossRef]
- Tsetsos, N.; Poutoglidis, A.; Vlachtsis, K.; Stavrakas, M.; Nikolaou, A.; Fyrmpas, G. Twenty-Year Experience with Salvage Total Laryngectomy: Lessons Learned. J. Laryngol. Otol. 2021, 135, 729–736. [Google Scholar] [CrossRef]
- Bussu, F.; Paludetti, G.; Almadori, G.; De Virgilio, A.; Galli, J.; Miccichè, F.; Tombolini, M.; Rizzo, D.; Gallo, A.; Giglia, V.; et al. Comparison of Total Laryngectomy with Surgical (cricohyoidopexy) and Nonsurgical Organ-Preservation Modalities in Advanced Laryngeal Squamous Cell Carcinomas: A Multicenter Retrospective Analysis. Head Neck 2013, 35, 554–561. [Google Scholar] [CrossRef]
- de Vincentiis, M.; De Virgilio, A.; Bussu, F.; Gallus, R.; Gallo, A.; Bastanza, G.; Parrilla, C.; Greco, A.; Galli, J.; Turchetta, R.; et al. Oncologic Results of the Surgical Salvage of Recurrent Laryngeal Squamous Cell Carcinoma in a Multicentric Retrospective Series: Emerging Role of Supracricoid Partial Laryngectomy. Head Neck 2015, 37, 84–91. [Google Scholar] [CrossRef]
- Forastiere, A.A.; Ismaila, N.; Lewin, J.S.; Nathan, C.A.; Adelstein, D.J.; Eisbruch, A.; Fass, G.; Fisher, S.G.; Laurie, S.A.; Le, Q.-T.; et al. Use of Larynx-Preservation Strategies in the Treatment of Laryngeal Cancer: American Society of Clinical Oncology Clinical Practice Guideline Update. J. Clin. Oncol. 2018, 36, 1143–1169. [Google Scholar] [CrossRef]
- Bussu, F.; Almadori, G.; De Corso, E.; Rizzo, D.; Rigante, M.; Parrilla, C.; Valentini, V.; Paludetti, G. Endoscopic Horizontal Partial Laryngectomy by CO(2) Laser in the Management of Supraglottic Squamous Cell Carcinoma. Head Neck 2009, 31, 1196–1206. [Google Scholar] [CrossRef]
- Banko, B.; Dukić, V.; Milovanović, J.; Kovač, J.D.; Artiko, V.; Maksimović, R. Diagnostic Significance of Magnetic Resonance Imaging in Preoperative Evaluation of Patients with Laryngeal Tumors. Eur. Arch. Otorhinolaryngol. 2011, 268, 1617–1623. [Google Scholar] [CrossRef]
- Ryu, I.S.; Lee, J.H.; Roh, J.-L.; Choi, S.-H.; Nam, S.Y.; Kim, S.Y.; Cho, K.-J. Clinical Implication of Computed Tomography Findings in Patients with Locally Advanced Squamous Cell Carcinoma of the Larynx and Hypopharynx. Eur. Arch. Otorhinolaryngol. 2015, 272, 2939–2945. [Google Scholar] [CrossRef]
- Friedland, P.L.; Bozic, B.; Dewar, J.; Kuan, R.; Meyer, C.; Phillips, M. Impact of Multidisciplinary Team Management in Head and Neck Cancer Patients. Br. J. Cancer 2011, 104, 1246–1248. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Liu, J.C.; Kaplon, A.; Blackman, E.; Miyamoto, C.; Savior, D.; Ragin, C. The Impact of the Multidisciplinary Tumor Board on Head and Neck Cancer Outcomes. Laryngoscope 2020, 130, 946–950. [Google Scholar] [CrossRef] [PubMed]
- Caudell, J.J.; Gillison, M.L.; Maghami, E.; Spencer, S.; Pfister, D.G.; Adkins, D.; Birkeland, A.C.; Brizel, D.M.; Busse, P.M.; Cmelak, A.J.; et al. NCCN Guidelines® Insights: Head and Neck Cancers, Version 1.2022: Featured Updates to the NCCN Guidelines. J. Natl. Compr. Cancer Netw. 2022, 20, 224–234. [Google Scholar] [CrossRef] [PubMed]
- Li, H.Y.; Chen, X.H. Diagnostic value of enhanced CT/MRI for thyroid cartilage invasion by malignant tumor. Zhonghua Er Bi Yan Hou Tou Jing Wai Ke Za Zhi 2017, 52, 372–376. [Google Scholar] [CrossRef]
- Bussu, F.; Galli, J.; Valenza, V.; D’Alatri, L.; Pizzuto, D.A.; Almadori, G.; Giordano, A.; Paludetti, G. Evaluation of Swallowing Function after Supracricoid Laryngectomy as a Primary or Salvage Procedure. Dysphagia 2015, 30, 686–694. [Google Scholar] [CrossRef]
- Acevedo Ortiz, L.; Aguilera Aguilera, G.A.; Lasierra Concellón, M.; Carboni Muñoz, M.A.; Andreu Mencia, L.; Soteras Olle, J.; Garcia Gonzalez, B.; Galindo Ortego, F.J. Comparison of Patients with Total and Salvage Laryngectomy. Acta Otorrinolaringol. Esp. 2021, 72, 352–358. [Google Scholar] [CrossRef]
- Soudry, E.; Hadar, T.; Shvero, J.; Segal, K.; Shpitzer, T.; Nageris, B.I.; Feinmesser, R. The Impact of Positive Resection Margins in Partial Laryngectomy for Advanced Laryngeal Carcinomas and Radiation Failures. Clin. Otolaryngol. 2010, 35, 402–408. [Google Scholar] [CrossRef]
- León, X.; Montoro, V.; Rovira, C.; Neumann, E.; López, M.; García, J.; Quer, M. Oncological Results of Salvage Laryngectomy in Patients with Laryngeal Carcinoma. Acta Otorrinolaringol. Esp. 2020, 71, 70–77. [Google Scholar] [CrossRef]
- Rizzotto, G.; Crosetti, E.; Lucioni, M.; Bertolin, A.; Monticone, V.; Sprio, A.E.; Berta, G.N.; Succo, G. Oncologic Outcomes of Supratracheal Laryngectomy: Critical Analysis. Head Neck 2015, 37, 1417–1424. [Google Scholar] [CrossRef]
- Succo, G.; Crosetti, E.; Bertolin, A.; Piazza, C.; Molteni, G.; Cirillo, S.; Petracchini, M.; Tascone, M.; Sprio, A.E.; Berta, G.N.; et al. Treatment for T3 to T4a Laryngeal Cancer by Open Partial Horizontal Laryngectomies: Prognostic Impact of Different Pathologic Tumor Subcategories. Head Neck 2018, 40, 1897–1908. [Google Scholar] [CrossRef]
- American Society of Clinical Oncology; Pfister, D.G.; Laurie, S.A.; Weinstein, G.S.; Mendenhall, W.M.; Adelstein, D.J.; Ang, K.K.; Clayman, G.L.; Fisher, S.G.; Forastiere, A.A.; et al. American Society of Clinical Oncology Clinical Practice Guideline for the Use of Larynx-Preservation Strategies in the Treatment of Laryngeal Cancer. J. Clin. Oncol. 2006, 24, 3693–3704. [Google Scholar] [CrossRef]
- Alicandri-Ciufelli, M.; Piccinini, A.; Grammatica, A.; Chiesi, A.; Bergamini, G.; Luppi, M.P.; Nizzoli, F.; Ghidini, A.; Tassi, S.; Presutti, L. Voice and Swallowing after Partial Laryngectomy: Factors Influencing Outcome. Head Neck 2013, 35, 214–219. [Google Scholar] [CrossRef]
- Laccourreye, O.; Hans, S.; Borzog-Grayeli, A.; Maulard-Durdux, C.; Brasnu, D.; Housset, M. Complications of Postoperative Radiation Therapy after Partial Laryngectomy in Supraglottic Cancer: A Long-Term Evaluation. Otolaryngol. Head Neck Surg. 2000, 122, 752–757. [Google Scholar] [CrossRef]
- Petrone, G.; Rossi, E.D.; Gallus, R.; Petrelli, L.; Marrone, S.; Rizzo, D.; Piras, A.; Garofalo, G.; Rindi, G.; Galli, J.; et al. Utility of Ultrasound-Guided Fine Needle Aspiration Cytology in Assessing Malignancy in Head and Neck Pathology. Cytopathology 2021, 32, 407–415. [Google Scholar] [CrossRef]
- Castaldi, P.; Rufini, V.; Bussu, F.; Miccichè, F.; Dinapoli, N.; Autorino, R.; Lago, M.; De Corso, E.; Almadori, G.; Galli, J.; et al. Can “Early” and “late”18F-FDG PET-CT Be Used as Prognostic Factors for the Clinical Outcome of Patients with Locally Advanced Head and Neck Cancer Treated with Radio-Chemotherapy? Radiother. Oncol. 2012, 103, 63–68. [Google Scholar] [CrossRef]
- Castaldi, P.; Leccisotti, L.; Bussu, F.; Miccichè, F.; Rufini, V. Role of (18)F-FDG PET-CT in Head and Neck Squamous Cell Carcinoma. Acta Otorhinolaryngol. Ital. 2013, 33, 1–8. [Google Scholar]
- Tsetsos, N.; Poutoglidis, A.; Arsos, G.; Tsentemeidou, A.; Kilmpasanis, A.; Katsampoukas, D.; Fyrmpas, G. 18F-FDG-PET/CT Interpretation Pitfalls in Patients with Head and Neck Cancer. Am. J. Otolaryngol. 2022, 43, 103209. [Google Scholar] [CrossRef]
- Locatello, L.G.; Pietragalla, M.; Taverna, C.; Bonasera, L.; Massi, D.; Mannelli, G. A Critical Reappraisal of Primary and Recurrent Advanced Laryngeal Cancer Staging. Ann. Otol. Rhinol. Laryngol. 2019, 128, 36–43. [Google Scholar] [CrossRef]
- Pietragalla, M.; Nardi, C.; Bonasera, L.; Mungai, F.; Verrone, G.B.; Calistri, L.; Taverna, C.; Novelli, L.; Locatello, L.G.; Mannelli, G.; et al. Current Role of Computed Tomography Imaging in the Evaluation of Cartilage Invasion by Laryngeal Carcinoma. Radiol. Med. 2020, 125, 1301–1310. [Google Scholar] [CrossRef]
- Kuno, H.; Sakamaki, K.; Fujii, S.; Sekiya, K.; Otani, K.; Hayashi, R.; Yamanaka, T.; Sakai, O.; Kusumoto, M. Comparison of MR Imaging and Dual-Energy CT for the Evaluation of Cartilage Invasion by Laryngeal and Hypopharyngeal Squamous Cell Carcinoma. AJNR Am. J. Neuroradiol. 2018, 39, 524–531. [Google Scholar] [CrossRef]
- Agnello, F.; Cupido, F.; Sparacia, G.; Midiri, F.; Miroddi, M.; Grassedonio, E.; Galia, M. Computerised Tomography and Magnetic Resonance Imaging of Laryngeal Squamous Cell Carcinoma: A Practical Approach. Neuroradiol. J. 2017, 30, 197–204. [Google Scholar] [CrossRef] [PubMed]
- Havsteen, I.; Ohlhues, A.; Madsen, K.H.; Nybing, J.D.; Christensen, H.; Christensen, A. Are Movement Artifacts in Magnetic Resonance Imaging a Real Problem?-A Narrative Review. Front. Neurol. 2017, 8, 232. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Wu, J.-H.; Zhao, J.; Li, Z.-H.; Yang, W.-Q.; Liu, Q.-H.; Yang, Z.-Y.; Liao, B.; Li, X.-L.; Wang, B.; Qin, H.; et al. Comparison of CT and MRI in Diagnosis of Laryngeal Carcinoma with Anterior Vocal Commissure Involvement. Sci. Rep. 2016, 6, 30353. [Google Scholar] [CrossRef] [PubMed]
- Maroldi, R.; Ravanelli, M.; Farina, D. Magnetic Resonance for Laryngeal Cancer. Curr. Opin. Otolaryngol. Head Neck Surg. 2014, 22, 131–139. [Google Scholar] [CrossRef]


| Surgical Treatment (n,%) | |||||||
|---|---|---|---|---|---|---|---|
| Parameters | Whole Series | Total laryngectomy 32 (71.1%) | Partial laryngeal surgery 13 (28.8%) | ||||
| OPHL II 12 (26.6%) | EHSL 1 (2.2%) | ||||||
| Age (mean +/− SD) | 65.7 +/− 10.6 | 65.9 +/− 10.6 | 64.3 +/− 8.3 | 75 | |||
| Gender (n, %) | |||||||
| Male | 41 (91.1%) | 29 (90.6%) | 12 (100%) | 0 | |||
| Female | 4 (8.9%) | 3 (9.4%) | 0 | 1 (100%) | |||
| Smoking status (n, %) | |||||||
| Current | 21 (46.7%) | 16 (50%) | 4 (34%) | 0 | |||
| Former | 22 (48.9%) | 16 (50%) | 6 (50%) | 1 (100%) | |||
| Never | 2 (4.4%) | 0 | 2 (16%) | 0 | |||
| Drinking status (n, %) | |||||||
| Current | 29 (64.5%) | 19 (59.4%) | 10 (84%) | 0 | |||
| Former | 5 (11.1%) | 5 (15.6%) | 0 | 0 | |||
| Never | 11 (24.4%) | 8 (25%) | 2 (16%) | 1 (100%) | |||
| Relevant comorbidities (n, %) | |||||||
| yes | 38 (84.4%) | 25 (78.1%) | 12 (100%) | 1 (100%) | |||
| no | 7 (15.6%) | 7 (21.9%) | 0 | 0 | |||
| Renal failure 2 (5.2%) | |||||||
| Liver failure 2 (5.2%) | |||||||
| Diabetes 8 (21%) | |||||||
| CPDO 4 (10.5%) | |||||||
| Cardiovascular disease 11 (28.9%) | |||||||
| Addiction 1 (2.6%) | |||||||
| Other 10 (26.3%) | |||||||
| Tumor site (n, %) | |||||||
| Glottic larynx | 29 (64.5%) | 18 (56.3%) | 11 (91.7%) | 0 | |||
| Supraglottic larynx | 10 (22.2%) | 8 (25%) | 1 (8.3%) | 1 (100%) | |||
| Hypopharynx | 5 (11.1%) | 5 (15.6%) | 0 | 0 | |||
| Subglottic larynx | 1 (2.2%) | 1 (3.1%) | 0 | 0 | |||
| Histology (n, %) SCC | 45 (100%) | 32 (100%) | 12 (100%) | 1 (100%) | |||
| Primary/Recurrence (n, %) | |||||||
| Primary | 41 (91.1%) | 28 (87.5%) | 12 (100%) | 1 (100%) | |||
| Recurrence | 4 (8.9%) | 4 (12.5%) | 0 | 0 | |||
| Margins (n, %) | |||||||
| R0 | 38 (84.4%) | 26 (81.3%) | 11 (91.7%) | 1 (100%) | |||
| R1 | 1 (2.2%) | 1 (3.1%) | 0 | 0 | |||
| Close | 6 (13.4%) | 5 (15.6%) | 1 (8.3%) | 0 | |||
| Voice prosthesis (n, %) | |||||||
| Yes | 15 (33.3%) | 15 (46.9%) | 0 | 0 | |||
| no | 30 (66.7%) | 17 (53.1%) | 12 (100%) | 1 (100%) | |||
| Pectoralis major flap (n, %) | |||||||
| Yes | 3 (6.7%) | 3 (9.4%) | 0 | 0 | |||
| no | 42 (93.3%) | 29 (90.6%) | 12 (100%) | 1 (100%) | |||
| follow up +/− SD (months) | 24.24 +/− 14.82 | 24.24 +/− 14.82 | 27.29 +/− 13.96 | 45.07 | |||
| Recurrence (n, %) | |||||||
| local | 1 (2.2%) | 1 (3.1%) | 0 | 0 | |||
| regional | 2 (4.4%) | 1 (3.1%) | 1 (8.3%) | 0 | |||
| distant | 2 (4.4%) | 2 (6.3%) | 0 | 0 | |||
| no | 40 (89%) | 28 (87.5%) | 11 (91.7%) | 1 (100%) | |||
| Status (n, %) | |||||||
| alive | 35 (77.8%) | 22 (68.7%) | 12 (100%) | 1 (100%) | |||
| dead | 10 (22.2%) | 10 (31.3%) | 0 | 0 | |||
| Cause of dead (n, %) | |||||||
| tumor | 3 (6.7%) | 3 (9.4%) | 0 | 0 | |||
| other causes | 7 (15.6%) | 7 (21.9%) | 0 | 0 | |||
| cT | |||||||
| T1 | 1 (2.2%) | 0 | 0 | 1 (100%) | |||
| T1a | 0 | 0 | 0 | 0 | |||
| T1b | 0 | 0 | 0 | 0 | |||
| T2 | 14 (31.1%) | 7 (21.9%) | 7 (58.3%) | 0 | |||
| T3 | 25 (55.6%) | 20 (62.5%) | 5 (41.7%) | 0 | |||
| T4a | 5 (11.1%) | 5 (15.6%) | 0 | 0 | |||
| T4b | 0 | 0 | 0 | 0 | |||
| cN | |||||||
| N0 | 34 (75.5%) | 21 (65.6%) | 12 (100%) | 0 | |||
| N1 | 8 (17.8%) | 8 (25%) | 0 | 0 | |||
| N2a | 0 | 0 | 0 | 0 | |||
| N2b | 3 (6.7%) | 3 (9.4%) | 0 | 0 | |||
| N2c | 0 | 0 | 0 | 0 | |||
| N3a | 0 | 0 | 0 | 0 | |||
| N3b | 0 | 0 | 0 | 0 | |||
| pT | |||||||
| T1 | 1 (2.2%) | 0 | 0 | 1 (100%) | |||
| T2 | 13 (28.9%) | 6 (18.7%) | 7 (58.3%) | 0 | |||
| T3 | 21 (46.7%) | 16 (50%) | 5 (41.7%) | 0 | |||
| T4a | 10 (22.2%) | 10 (31.3%) | 0 | 0 | |||
| pN | |||||||
| N0 | 33 (73.3%) | 20 (62.5%) | 12 (100%) | 1 (100%) | |||
| N1 | 5 (11.1%) | 5 (15.6%) | 0 | 0 | |||
| N2a | 1 (2.2%) | 1 (3.1%) | 0 | 0 | |||
| N2b | 3 (6.7%) | 3 (9.4%) | 0 | 0 | |||
| N2c | 0 | 0 | 0 | 0 | |||
| N3b | 3 (6.7%) | 3 (9.4%) | 0 | 0 | |||
| Clinical stage | |||||||
| I | 0 | 0 | 0 | 0 | |||
| II | 21 (46.7%) | 8 (25%) | 12 (100%) | 1 (100%) | |||
| III | 22 (48.9%) | 22 (68.7%) | 0 | 0 | |||
| IVa | 2 (4.4%) | 2 (6.3%) | 0 | 0 | |||
| IVb | 0 | 0 | 0 | 0 | |||
| IVc | 0 | 0 | 0 | 0 | |||
| Comparison of T and N classifications | |||||||
| ep TN | rad TN | c TN | p TN | ||||
| T n% | N n% | T n% | N n% | T n% | N n% | T n% | N n% |
| T1 1 (2.2%) | N0 40 (88.9%) | T1 1 (2.2%) | N0 34 (75.5%) | T1 1 (2.2%) | N0 34 (75.5%) | T1 1 (2.2%) | N0 33 (73.3%) |
| T2 22 (48.9%) | N1 4 (8.9%) | T1a 5 (11.1%) | N1 8 (17.8%) | T2 14 (31.1%) | N1 8 (17.8%) | T2 13 (28.9%) | N1 5 (11.1%) |
| T3 22 (48.9%) | N2b 1 (2.2%) | T1b 2 (4.5%) | N2b 3 (6.7%) | T3 25 (55.6%) | N2b 3 (6.7%) | T3 21 (46.7%) | N2a 1 (2.2%) |
| T2 6 (13.3%) | T4a 5 (11.1%) | T4a 10 (22.2%) | N2b 3 (6.7%) | ||||
| T3 26 (57.8%) | N3b 3 (6.7%) | ||||||
| T4a 5 (11.1%) | |||||||
| ep TN | rad TN | c TN | |
|---|---|---|---|
| T classification (agreement rate % with pT; kappa coefficient) | 58%; 0.32 | 64%; 0.44 | 82%; 0.7 |
| N classification (agreement rate % with pN; kappa coefficient) | 76%; 0.27 | 76%; 0.42 | 76%; 0.42 |
| N0 vs. N+ (agreement rate % with pN; kappa coefficient) | 80%; 0.37 | 80%; 0.47 | 80%; 0.47 |
| Single parameter (rate %) | |||
| Endoscopy/Physical exam | Radiology | Pathology | |
| Laryngeal vestibule/Piriform sinus inlet (Arytenoid/Aryepiglottic fold/suprahyoid epiglottis) involvement | 35% | 42% | 37% |
| Lateral wall/apex of piriform sinus involvement | 16% | 20% | 15% |
| Infrahyoid epiglottis involvement | 26% | 24% | 23% |
| True vocal fold involvement | 85% | 80% | 84% |
| Anterior commissure | 77% | 47% | 60% |
| False vocal fold involvement | 59% | 62% | 53% |
| Laryngeal mobility | Hypomobility 36% True vocal fold/arytenoid fixation 51% | - | - |
| Anterior paraglottic space involvement | 8% | 60% | 58% |
| Posterior paraglottic space involvement | 10% | 27% | 12% |
| Cricoid cartilage involvement | - | 11% | 11% |
| Thyroid cartilage involvement | - | 24% * | 21% |
| Subglottic extension | 31% | 18% | 26% |
| Base of tongue involvement | 8% | 10% | 10% |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Rizzo, D.; Crescio, C.; Tramaloni, P.; De Luca, L.M.; Turra, N.; Manca, A.; Crivelli, P.; Tiana, C.R.; Fara, A.; Cossu, A.; et al. Reliability of a Multidisciplinary Multiparametric Approach in the Surgical Planning of Laryngeal Squamous Cell Carcinomas: A Retrospective Observational Study. J. Pers. Med. 2022, 12, 1585. https://doi.org/10.3390/jpm12101585
Rizzo D, Crescio C, Tramaloni P, De Luca LM, Turra N, Manca A, Crivelli P, Tiana CR, Fara A, Cossu A, et al. Reliability of a Multidisciplinary Multiparametric Approach in the Surgical Planning of Laryngeal Squamous Cell Carcinomas: A Retrospective Observational Study. Journal of Personalized Medicine. 2022; 12(10):1585. https://doi.org/10.3390/jpm12101585
Chicago/Turabian StyleRizzo, Davide, Claudia Crescio, Pierangela Tramaloni, Laura M. De Luca, Nicola Turra, Alessandra Manca, Paola Crivelli, Chiara R. Tiana, Alberto Fara, Antonio Cossu, and et al. 2022. "Reliability of a Multidisciplinary Multiparametric Approach in the Surgical Planning of Laryngeal Squamous Cell Carcinomas: A Retrospective Observational Study" Journal of Personalized Medicine 12, no. 10: 1585. https://doi.org/10.3390/jpm12101585
APA StyleRizzo, D., Crescio, C., Tramaloni, P., De Luca, L. M., Turra, N., Manca, A., Crivelli, P., Tiana, C. R., Fara, A., Cossu, A., Profili, S., Scaglione, M., & Bussu, F. (2022). Reliability of a Multidisciplinary Multiparametric Approach in the Surgical Planning of Laryngeal Squamous Cell Carcinomas: A Retrospective Observational Study. Journal of Personalized Medicine, 12(10), 1585. https://doi.org/10.3390/jpm12101585