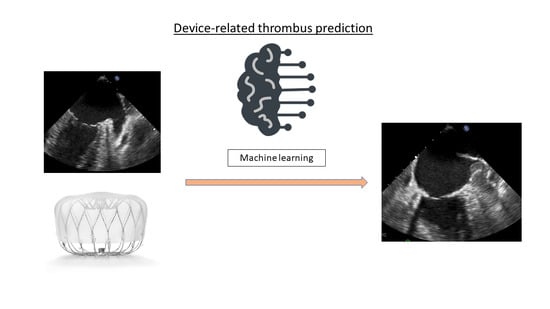
Predictive Power for Thrombus Detection after Atrial Appendage Closure: Machine Learning vs. Classical Methods
Abstract
:1. Introduction
2. Materials and Methods
2.1. Data
2.2. Multivariable Analysis
2.3. Machine Learning Feature Selection
2.4. Experiments Performed
2.4.1. No Resampling Experiments
2.4.2. Resampling Experiments
2.5. Experiments Design
2.6. Software
3. Results
3.1. Predictive Power
3.2. Predictor Variables
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Conflicts of Interest
References
- Developed with the Special Contribution of the European Heart Rhythm Association (EHRA); Endorsed by the European Association for Cardio-Thoracic Surgery (EACTS); Authors/Task Force Members; Camm, A.J.; Kirchhof, P.; Lip, G.Y.; Schotten, U.; Savelieva, I.; Ernst, S.; Van Gelder, I.C.; et al. Guidelines for the Management of Atrial Fibrillation: The Task Force for the Management of Atrial Fibrillation of the Management of Atrial Fibrillation of the European Society of Cardiology (ESC). Eur. Heart J. 2010, 31, 2369–2429. [Google Scholar] [PubMed]
- Lip, G.Y.H.; Nieuwlaat, R.; Pisters, R.; Lane, D.A.; Crijns, H.J.G.M. Refining Clinical Risk Stratification for Predicting Stroke and Thromboembolism in Atrial Fibrillation Using a Novel Risk Factor-Based Approach. Chest 2010, 137, 263–272. [Google Scholar] [CrossRef] [PubMed]
- Rivera-Caravaca, J.M.; Roldan, V.; Esteve-Pastor, M.A.; Valdes, M.; Vicente, V.; Lip, G.Y.; Marin, F. Long-Term Stroke Risk Prediction in Patients With Atrial Fibrillation: Comparison of the ABC-Stroke and CHA 2 DS 2-VAS c Scores. J. Am. Heart Assoc. 2017, 6, e006490. [Google Scholar] [PubMed]
- Glikson, M.; Wolff, R.; Hindricks, G.; Mandrola, J.; Camm, A.J.; Lip, G.Y.; Fauchier, L.; Betts, T.R.; Lewalter, T.; Saw, J. EHRA/EAPCI Expert Consensus Statement on Catheter-Based Left Atrial Appendage Occlusion—An Update. EP Eur. 2020, 22, 184. [Google Scholar] [CrossRef]
- Cruz-González, I.; Trejo-Velasco, B. Percutaneous Left Atrial Appendage Occlusion in the Current Practice. Kardiol. Pol. (Pol. Heart J.) 2021, 79, 255–268. [Google Scholar] [CrossRef]
- Reddy, V.Y.; Doshi, S.K.; Kar, S.; Gibson, D.N.; Price, M.J.; Huber, K.; Horton, R.P.; Buchbinder, M.; Neuzil, P.; Gordon, N.T. 5-Year Outcomes after Left Atrial Appendage Closure: From the PREVAIL and PROTECT AF Trials. J. Am. Coll. Cardiol. 2017, 70, 2964–2975. [Google Scholar]
- Osmancik, P.; Herman, D.; Neuzil, P.; Hala, P.; Taborsky, M.; Kala, P.; Poloczek, M.; Stasek, J.; Haman, L.; Branny, M. 4-Year Outcomes After Left Atrial Appendage Closure Versus Nonwarfarin Oral Anticoagulation for Atrial Fibrillation. J. Am. Coll. Cardiol. 2022, 79, 1–14. [Google Scholar]
- Freeman, J.V.; Higgins, A.Y.; Wang, Y.; Du, C.; Friedman, D.J.; Daimee, U.A.; Minges, K.E.; Pereira, L.; Goldsweig, A.M.; Price, M.J.; et al. Antithrombotic Therapy After Left Atrial Appendage Occlusion in Patients With Atrial Fibrillation. J. Am. Coll. Cardiol. 2022, 79, 1785–1798. [Google Scholar] [CrossRef]
- Fauchier, L.; Cinaud, A.; Brigadeau, F.; Lepillier, A.; Pierre, B.; Abbey, S.; Fatemi, M.; Franceschi, F.; Guedeney, P.; Jacon, P.; et al. Device-Related Thrombosis After Percutaneous Left Atrial Appendage Occlusion for Atrial Fibrillation. J. Am. Coll. Cardiol. 2018, 71, 1528–1536. [Google Scholar] [CrossRef]
- Simard, T.; Jung, R.G.; Lehenbauer, K.; Piayda, K.; Pracoń, R.; Jackson, G.G.; Flores-Umanzor, E.; Faroux, L.; Korsholm, K.; Chun, J.K.R.; et al. Predictors of Device-Related Thrombus Following Percutaneous Left Atrial Appendage Occlusion. J. Am. Coll. Cardiol. 2021, 78, 297–313. [Google Scholar] [CrossRef]
- Dukkipati, S.R.; Kar, S.; Holmes, D.R.; Doshi, S.K.; Swarup, V.; Gibson, D.N.; Maini, B.; Gordon, N.T.; Main, M.L.; Reddy, V.Y. Device-Related Thrombus After Left Atrial Appendage Closure: Incidence, Predictors, and Outcomes. Circulation 2018, 138, 874–885. [Google Scholar] [CrossRef]
- Sedaghat, A.; Vij, V.; Al-Kassou, B.; Gloekler, S.; Galea, R.; Fürholz, M.; Meier, B.; Valgimigli, M.; O’Hara, G.; Arzamendi, D.; et al. Device-Related Thrombus After Left Atrial Appendage Closure. Circ. Cardiovasc. Interv. 2021, 14, 544–553. [Google Scholar] [CrossRef] [PubMed]
- Aminian, A.; Schmidt, B.; Mazzone, P.; Berti, S.; Fischer, S.; Montorfano, M.; Lam, S.C.C.; Lund, J.; Asch, F.M.; Gage, R.; et al. Incidence, Characterization, and Clinical Impact of Device-Related Thrombus Following Left Atrial Appendage Occlusion in the Prospective Global AMPLATZER Amulet Observational Study. JACC Cardiovasc. Interv. 2019, 12, 1003–1014. [Google Scholar] [CrossRef] [PubMed]
- Saw, J.; Tzikas, A.; Shakir, S.; Gafoor, S.; Omran, H.; Nielsen-Kudsk, J.E.; Kefer, J.; Aminian, A.; Berti, S.; Santoro, G.; et al. Incidence and Clinical Impact of Device-Associated Thrombus and Peri-Device Leak Following Left Atrial Appendage Closure With the Amplatzer Cardiac Plug. JACC Cardiovasc. Interv. 2017, 10, 391–399. [Google Scholar] [CrossRef]
- Budts, W.; Laenens, D.; Van Calenbergh, F.; Vermeersch, P.; De Potter, T.; Aminian, A.; Benit, E.; Stammen, F.; Kefer, J. Left Atrial Appendage Occlusion with the Amplatzer Cardiac Plug Could Improve Survival and Prevent Thrombo-Embolic and Major Bleeding Events in Atrial Fibrillation Patients with Increased Bleeding Risk. Acta Cardiol. 2016, 71, 135–143. [Google Scholar] [CrossRef]
- Kaneko, H.; Neuss, M.; Weissenborn, J.; Butter, C. Predictors of Thrombus Formation after Percutaneous Left Atrial Appendage Closure Using the WATCHMAN Device. Heart Vessel. 2017, 32, 1137–1143. [Google Scholar] [CrossRef] [PubMed]
- Vij, V.; Piayda, K.; Nelles, D.; Gloekler, S.; Galea, R.; Fürholz, M.; Meier, B.; Valgimigli, M.; O’Hara, G.; Arzamendi, D.; et al. Clinical and Echocardiographic Risk Factors for Device-Related Thrombus after Left Atrial Appendage Closure: An Analysis from the Multicenter EUROC-DRT Registry. Clin. Res. Cardiol. 2022, 1–10. [CrossRef]
- Sobh, M.; Cleophas, T.J.; Hadj-Chaib, A.; Zwinderman, A.H. Clinical Trials: Odds Ratios and Multiple Regression Models--Why and How to Assess Them. Am. J. Ther. 2008, 15, 44–52. [Google Scholar] [CrossRef]
- Hidalgo, B.; Goodman, M. Multivariate or Multivariable Regression? Am. J. Public Health 2013, 103, 39–40. [Google Scholar] [CrossRef] [PubMed]
- Ranganathan, P.; Pramesh, C.S.; Aggarwal, R. Common Pitfalls in Statistical Analysis: Logistic Regression. Perspect. Clin. Res. 2017, 8, 148–151. [Google Scholar] [CrossRef]
- De Bin, R.; Janitza, S.; Sauerbrei, W.; Boulesteix, A.-L. Subsampling versus Bootstrapping in Resampling-Based Model Selection for Multivariable Regression. Biometrics 2016, 72, 272–280. [Google Scholar] [CrossRef] [PubMed]
- Kahlert, J.; Gribsholt, S.B.; Gammelager, H.; Dekkers, O.M.; Luta, G. Control of Confounding in the Analysis Phase—an Overview for Clinicians. Clin. Epidemiol. 2017, 9, 195–204. [Google Scholar] [CrossRef] [Green Version]
- Pearl, J. Remarks on the Method of Propensity Score. Stat. Med. 2009, 28, 1415–1416. [Google Scholar] [CrossRef]
- Dorado-Díaz, P.I.; Sampedro-Gómez, J.; Vicente-Palacios, V.; Sánchez, P.L. Applications of Artificial Intelligence in Cardiology. The Future Is Already Here. Rev. Española de Cardiol. (Engl. Ed.) 2019, 72, 1065–1075. [Google Scholar] [CrossRef]
- Pérez-Sánchez, P.; Vicente-Palacios, V.; Barreiro, M.; Díaz-Peláez, E.; Sanchez Puente, A.; Sampedro-Gómez, J.; García-Galindo, A.; Dorado-Díaz, P.; Sanchez, P. Automatic Classification of Valve Diseases Through Natural Language Processing in Spanish and Active Learning. In International Conference on Bioengineering and Biomedical Signal and Image Processing, Proceedings of the First International Conference, BIOMESIP 2021, Meloneras, Gran Canaria, Spain, 19–21 July 2021; Springer: Cham, Switzerland, 2021; pp. 39–50. ISBN 978-3-030-88162-7. [Google Scholar]
- Chen, C.; Qin, C.; Qiu, H.; Tarroni, G.; Duan, J.; Bai, W.; Rueckert, D. Deep Learning for Cardiac Image Segmentation: A Review. Front. Cardiovasc. Med. 2020, 7, 25. [Google Scholar] [CrossRef] [PubMed]
- Maadi, M.; Akbarzadeh Khorshidi, H.; Aickelin, U. A Review on Human–AI Interaction in Machine Learning and Insights for Medical Applications. Int. J. Environ. Res. Public Health 2021, 18, 2121. [Google Scholar] [CrossRef]
- Wilkinson, J.; Arnold, K.F.; Murray, E.J.; van Smeden, M.; Carr, K.; Sippy, R.; de Kamps, M.; Beam, A.; Konigorski, S.; Lippert, C.; et al. Time to Reality Check the Promises of Machine Learning-Powered Precision Medicine. Lancet. Digit. Health 2020, 2, e677–e680. [Google Scholar] [CrossRef]
- Roberts, M.; Driggs, D.; Thorpe, M.; Gilbey, J.; Yeung, M.; Ursprung, S.; Aviles-Rivero, A.I.; Etmann, C.; McCague, C.; Beer, L.; et al. Common Pitfalls and Recommendations for Using Machine Learning to Detect and Prognosticate for COVID-19 Using Chest Radiographs and CT Scans. Nat. Mach. Intell. 2021, 3, 199–217. [Google Scholar] [CrossRef]
- Kraiem, M.S.; Sánchez-Hernández, F.; Moreno-García, M.N. Selecting the Suitable Resampling Strategy for Imbalanced Data Classification Regarding Dataset Properties. An Approach Based on Association Models. Appl. Sci. 2021, 11, 8546. [Google Scholar] [CrossRef]
- Yaman, E.; Subasi, A. Comparison of Bagging and Boosting Ensemble Machine Learning Methods for Automated EMG Signal Classification. Biomed. Res. Int. 2019, 2019, 9152506. [Google Scholar] [CrossRef]
- Avram, R.; Olgin, J.E.; Tison, G.H. The Rise of Open-Sourced Machine Learning in Small and Imbalanced Datasets: Predicting In-Stent Restenosis. Can. J. Cardiol. 2020, 36, 1574–1576. [Google Scholar] [CrossRef] [PubMed]
- Sampedro-Gómez, J.; Dorado-Díaz, P.I.; Vicente-Palacios, V.; Sánchez-Puente, A.; Jiménez-Navarro, M.; Roman, J.A.S.; Galindo-Villardón, P.; Sanchez, P.L.; Fernández-Avilés, F. Machine Learning to Predict Stent Restenosis Based on Daily Demographic, Clinical, and Angiographic Characteristics. Can. J. Cardiol. 2020, 36, 1624–1632. [Google Scholar] [CrossRef] [PubMed]
- Faroux, L.; Cruz-González, I.; Arzamendi, D.; Freixa, X.; Nombela-Franco, L.; Peral, V.; Caneiro-Queija, B.; Mangieri, A.; Trejo-Velasco, B.; Asmarats, L.; et al. Effect of Glomerular Filtration Rates on Outcomes Following Percutaneous Left Atrial Appendage Closure. Am. J. Cardiol. 2021, 145, 77–84. [Google Scholar] [CrossRef] [PubMed]
- Faroux, L.; Cruz-González, I.; Arzamendi, D.; Freixa, X.; Nombela-Franco, L.; Peral, V.; Caneiro-Queija, B.; Mangieri, A.; Trejo-Velasco, B.; Asmarats, L.; et al. Short-Term Direct Oral Anticoagulation or Dual Antiplatelet Therapy Following Left Atrial Appendage Closure in Patients with Relative Contraindications to Chronic Anticoagulation Therapy. Int. J. Cardiol. 2021, 333, 77–82. [Google Scholar] [CrossRef]
- Mesnier, J.; Cruz-González, I.; Arzamendi, D.; Freixa, X.; Nombela-Franco, L.; Peral, V.; Caneiro-Queija, B.; Mangieri, A.; Trejo-Velasco, B.; Asmarats, L.; et al. Early Discontinuation of Antithrombotic Treatment Following Left Atrial Appendage Closure. Am. J. Cardiol. 2022, 171, 91–98. [Google Scholar] [CrossRef]
- Regueiro, A.; Cruz-Gonzalez, I.; Bethencourt, A.; Nombela-Franco, L.; Champagne, J.; Asmarats, L.; Jiménez-Quevedo, P.; Rodriguez-Gabella, T.; Rama-Merchan, J.C.; Puri, R.; et al. Long-Term Outcomes Following Percutaneous Left Atrial Appendage Closure in Patients with Atrial Fibrillation and Contraindications to Anticoagulation. J. Interv. Card. Electrophysiol. 2018, 52, 53–59. [Google Scholar] [CrossRef]
- Saeys, Y.; Inza, I.; Larrañaga, P. A Review of Feature Selection Techniques in Bioinformatics. Bioinformatics 2007, 23, 2507–2517. [Google Scholar] [CrossRef]
- Kamalov, F.; Thabtah, F.; Leung, H.H. Feature Selection in Imbalanced Data. Ann. Data. Sci. 2022. [Google Scholar] [CrossRef]
- Pedregosa, F.; Varoquaux, G.; Gramfort, A.; Michel, V.; Thirion, B.; Grisel, O.; Blondel, M.; Prettenhofer, P.; Weiss, R.; Dubourg, V.; et al. Scikit-Learn: Machine Learning in Python. J. Mach. Learn. Res. 2011, 12, 2825–2830. [Google Scholar]
- Goodfellow, I.; Bengio, Y.; Courville, A. Machine Learning Basics. In Deep Learning; MIT Press: Cambridge, MA, USA, 2016; pp. 216–218. [Google Scholar]
- Breiman, L. Random Forests. Mach. Learn. 2001, 45, 5–32. [Google Scholar] [CrossRef]
- Friedman, J.H. Greedy Function Approximation: A Gradient Boosting Machine. Ann. Stat. 2001, 29, 1189–1232. [Google Scholar] [CrossRef]
- Grinsztajn, L.; Oyallon, E.; Varoquaux, G. Why Do Tree-Based Models Still Outperform Deep Learning on Tabular Data? arXiv 2022, arXiv:2207.08815. [Google Scholar]
- Seabold, S.; Perktold, J. Statsmodels: Econometric and Statistical Modeling with Python. Available online: https://pdfs.semanticscholar.org/3a27/6417e5350e29cb6bf04ea5a4785601d5a215.pdf (accessed on 20 June 2022).
- Virtanen, P.; Gommers, R.; Oliphant, T.E.; Haberland, M.; Reddy, T.; Cournapeau, D.; Burovski, E.; Peterson, P.; Weckesser, W.; Bright, J.; et al. SciPy 1.0: Fundamental Algorithms for Scientific Computing in Python. Nat. Methods 2020, 17, 261–272. [Google Scholar] [CrossRef] [PubMed]
- Pérez-Sánchez, P.; Vicente-Palacios, V.; Sampedro-Gómez, J. IA-Cardiologia-Husa/LAAC_Thrombus_detection_MLvsClassical: Update 2022. Available online: https://github.com/IA-Cardiologia-husa/LAAC_Thrombus_detection_MLvsClassical (accessed on 20 June 2022).
- Della Rocca, D.G.; Magnocavallo, M.; Di Biase, L.; Mohanty, S.; Trivedi, C.; Tarantino, N.; Gianni, C.; Lavalle, C.; Van Niekerk, C.J.; Romero, J. Half-Dose Direct Oral Anticoagulation versus Standard Antithrombotic Therapy after Left Atrial Appendage Occlusion. Cardiovasc. Interv. 2021, 14, 2353–2364. [Google Scholar] [CrossRef] [PubMed]
- Belkin, M.; Hsu, D.; Ma, S.; Mandal, S. Reconciling Modern Machine-Learning Practice and the Classical Bias-Variance Trade-Off. Proc. Natl. Acad. Sci. USA 2019, 116, 15849–15854. [Google Scholar] [CrossRef]
- Akbilgic, O.; Davis, R.L. The Promise of Machine Learning: When Will It Be Delivered? J. Card. Fail. 2019, 25, 484–485. [Google Scholar] [CrossRef]




| Variables | All Patients (N = 813) |
|---|---|
| Age (Years) | 75.62 ± 8.43 (813) |
| Gender (Male) | 61.01 (496/813) |
| Weight (Kg) | 74.96 ± 15.55 (806) |
| Height (cm) | 164.73 ± 9.41 (804) |
| BMI * | 27.55 ± 4.94 (804) |
| BSA * | 1.81 ± 0.21 (804) |
| HTA * (Yes) | 87.33 (710/813) |
| Diabetes (Yes) | 33.7 (274/813) |
| Smoking (Yes) | 14.37 (127/696) |
| Prior stroke (Yes) | 35.36 (279/789) |
| Prior hemorrhagic stroke (Yes) | 24.8 (185/746) |
| Prior systemic embolization (Yes) | 9.85 (78/792) |
| Prior vascular disease (Yes) | 20.54 (167/813) |
| Previous CAD * (Yes) | 31.89 (258/809) |
| Previous MI * (Yes) | 20.08 (154/767) |
| Prior mitral valvular surgery | 2.70 (22/813) |
| CHADS2 | 2.96 ± 1.24 (768) |
| CHA2DS2VASc | 4.44 ± 1.54 (813) |
| HAS-BLED | 3.71 ± 1.05 (811) |
| Prior bleeding episodes | 1.57 ± 1.15 (768) |
| Labile INR * (Yes) | 11.07 (90/813) |
| Previously on ASA * (Yes) | 30.26 (246/813) |
| Previously on ADP inhibitor * (Yes) | 11.07 (90/813) |
| Previous antiVitK treatment (Yes) | 23.37 (190/813) |
| Previous severe mitral regurgitation (Yes) | 15.23 (122/801) |
| Previous severe mitral stenosis (Yes) | 0.26 (2/765) |
| Procedural device reposition (If available) | 0.59 ± 1 (570) |
| Procedure contrast volume | 134.03 ± 88.09 (695) |
| periprocedural pericardial effusion (Yes) | 5.9 (48/813) |
| ADP inhibitor at discharge * (Yes) | 62.64 (508/811) |
| Experiment | Resample | Feature Selection | Model | ROC AUC | Sensitivity | Specificity |
|---|---|---|---|---|---|---|
| I | - | Multivariable analysis | LR * | 0.5456 | 0.8857 | 0.2198 |
| II | - | Select from model | LR | 0.7974 | 0.6857 | 0.7776 |
| RF | 1.0 | 1.0 | 1.0 | |||
| GB | 1.0 | 1.0 | 1.0 | |||
| III | Shuffle split | Multivariable analysis | LR * | 0.4387 ± 0.0904 | 0.1811 ± 0.1143 | 0.6544 ± 0.2263 |
| k-fold | Multivariable analysis | LR * | 0.5174 ± 0.0531 | 0.4318 ± 0.3255 | 0.5504 ± 0.3173 | |
| IV | Shuffle split | Select from model | LR | 0.4838 ± 0.0118 | 0.1697 ± 0.0724 | 0.6960 ± 0.0109 |
| RF | 0.3989 ± 0.0240 | 0.0 ± 0.0 | 0.9014 ± 0.0639 | |||
| GB | 0.4614 ± 0.0437 | 0.0444 ± 0.0459 | 0.9217 ± 0.0073 | |||
| k-fold | Select from model | LR | 0.5325 ± 0.0349 | 0.2804 ± 0.0771 | 0.7634 ± 0.0518 | |
| RF | 0.4250 ± 0.354 | 0.0418 ± 0.0462 | 0.7049 ± 0.0193 | |||
| GB | 0.4893 ± 0.0668 | 0.0754 ± 0.0501 | 0.9005 ± 0.0176 |
| Var | Univariate p-Value | Multivariable p-Value |
|---|---|---|
| CHADS2 | <0.01 | 0.852 |
| CHA2DS2-VASC | <0.01 | 0.414 |
| HAS-BLED | <0.01 | <0.01 |
| Variable | Experiment III | Experiment IV | |
|---|---|---|---|
| Univariate | Multivariable | ||
| Previous CAD * | - | - | 10 |
| HAS-BLED | 10 | 8 | 10 |
| Previous antiVitK treatment | - | - | 10 |
| CHADS2 | 10 | - | 6 |
| CHA2DS2VASc | 10 | - | 6 |
| Chicken-wing LAA morphology | - | - | 9 |
| Previous severe mitral regurgitation | 1 | 1 | 9 |
| Prior bleeding episodes | - | - | 9 |
| Labile INR * | - | - | 9 |
| ADP inhibitor at discharge | - | - | 8 |
| Procedural device reposition | - | - | 8 |
| Severe CKD * | - | - | 8 |
| Periprocedural pericardial effusion | 1 | - | 8 |
| Diabetes | - | - | 7 |
| Prior stroke | - | - | 7 |
| Previously on ADP inhibitor * | - | - | 7 |
| Previously on ASA * | - | - | 7 |
| Prior systemic embolization | - | - | 7 |
| Prior vascular disease | - | - | 6 |
| Previous MI * | - | - | 6 |
| Prior hemorrhagic stroke | - | - | 6 |
| Procedure contrast volume | 1 | 1 | - |
| Prior valve surgery (mitral) | 1 | 1 | 5 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Antúnez-Muiños, P.; Vicente-Palacios, V.; Pérez-Sánchez, P.; Sampedro-Gómez, J.; Sánchez-Puente, A.; Dorado-Díaz, P.I.; Nombela-Franco, L.; Salinas, P.; Gutiérrez-García, H.; Amat-Santos, I.; et al. Predictive Power for Thrombus Detection after Atrial Appendage Closure: Machine Learning vs. Classical Methods. J. Pers. Med. 2022, 12, 1413. https://doi.org/10.3390/jpm12091413
Antúnez-Muiños P, Vicente-Palacios V, Pérez-Sánchez P, Sampedro-Gómez J, Sánchez-Puente A, Dorado-Díaz PI, Nombela-Franco L, Salinas P, Gutiérrez-García H, Amat-Santos I, et al. Predictive Power for Thrombus Detection after Atrial Appendage Closure: Machine Learning vs. Classical Methods. Journal of Personalized Medicine. 2022; 12(9):1413. https://doi.org/10.3390/jpm12091413
Chicago/Turabian StyleAntúnez-Muiños, Pablo, Víctor Vicente-Palacios, Pablo Pérez-Sánchez, Jesús Sampedro-Gómez, Antonio Sánchez-Puente, Pedro Ignacio Dorado-Díaz, Luis Nombela-Franco, Pablo Salinas, Hipólito Gutiérrez-García, Ignacio Amat-Santos, and et al. 2022. "Predictive Power for Thrombus Detection after Atrial Appendage Closure: Machine Learning vs. Classical Methods" Journal of Personalized Medicine 12, no. 9: 1413. https://doi.org/10.3390/jpm12091413
APA StyleAntúnez-Muiños, P., Vicente-Palacios, V., Pérez-Sánchez, P., Sampedro-Gómez, J., Sánchez-Puente, A., Dorado-Díaz, P. I., Nombela-Franco, L., Salinas, P., Gutiérrez-García, H., Amat-Santos, I., Peral, V., Morcuende, A., Asmarats, L., Freixa, X., Regueiro, A., Caneiro-Queija, B., Estevez-Loureiro, R., Rodés-Cabau, J., Sánchez, P. L., & Cruz-González, I. (2022). Predictive Power for Thrombus Detection after Atrial Appendage Closure: Machine Learning vs. Classical Methods. Journal of Personalized Medicine, 12(9), 1413. https://doi.org/10.3390/jpm12091413