Unmasking the Silent Threat: Periodontal Health’s Impact on COPD Severity and Hospitalization
Abstract
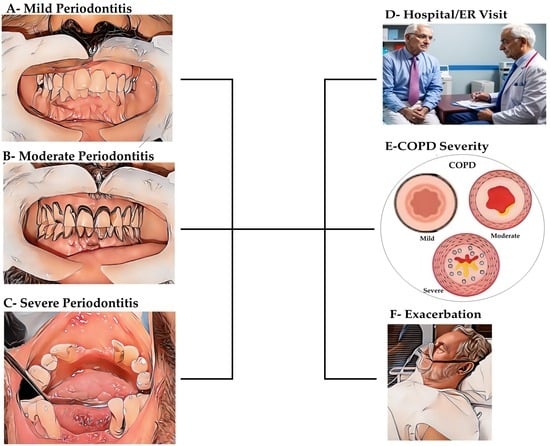
:1. Introduction
2. Materials and Methods
2.1. Study Design and Patients
2.2. Inclusion and Exclusion Criteria
2.3. Data Collection
2.4. Spirometry
2.5. Evaluation of Periodontal Status
2.6. Assessment of Probing Pocket Depth and Clinical Attachment Levels
2.7. Assessment of Plaque Index (PI)
2.8. Statistical Analysis
3. Results
3.1. Respiratory and Clinical Parameters
3.2. Periodontal Severity and COPD Exacerbations
3.3. Periodontal Indices and COPD Severity
3.4. Correlations and Regression Analyses
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Nibali, L.; Donos, N.; Henderson, B. Periodontal Infectogenomics. J. Med. Microbiol. 2009, 58, 1269–1274. [Google Scholar] [CrossRef] [PubMed]
- Laine, M.L.; Loos, B.G.; Crielaard, W. Gene Polymorphisms in Chronic Periodontitis. Int. J. Dent. 2010, 2010, 324719. [Google Scholar] [CrossRef] [PubMed]
- Lim, G.; Janu, U.; Chiou, L.-L.; Gandhi, K.K.; Palomo, L.; John, V. Periodontal Health and Systemic Conditions. Dent. J. 2020, 8, 130. [Google Scholar] [CrossRef] [PubMed]
- Knight, E.T.; Liu, J.; Seymour, G.J.; Faggion, C.M.; Cullinan, M.P. Risk Factors That May Modify the Innate and Adaptive Immune Responses in Periodontal Diseases. Periodontology 2000 2016, 71, 22–51. [Google Scholar] [CrossRef] [PubMed]
- Emrich, L.J.; Shlossman, M.; Genco, R.J. Periodontal Disease in Non-Insulin-Dependent Diabetes Mellitus. J. Periodontol. 1991, 62, 123–131. [Google Scholar] [CrossRef] [PubMed]
- Lalla, E.; Cheng, B.; Lal, S.; Kaplan, S.; Softness, B.; Greenberg, E.; Goland, R.S.; Lamster, I.B. Diabetes Mellitus Promotes Periodontal Destruction in Children. J. Clin. Periodontol. 2007, 34, 294–298. [Google Scholar] [CrossRef] [PubMed]
- Tsai, C.; Hayes, C.; Taylor, G.W. Glycemic Control of Type 2 Diabetes and Severe Periodontal Disease in the US Adult Population. Community Dent. Oral Epidemiol. 2002, 30, 182–192. [Google Scholar] [CrossRef]
- Salmen, T.; Mihai, B.M.; Iarca, R.A.; Stan, B.A.; Dima, V.; Bohiltea, R.E. Diabetes Mellitus and Periodontal Disease. Rom. J. Stomatol. 2021, 67, 244–246. [Google Scholar] [CrossRef]
- Pihlstrom, B.L.; Michalowicz, B.S.; Johnson, N.W. Periodontal Diseases. Lancet 2005, 366, 1809–1820. [Google Scholar] [CrossRef]
- Sanz, M.; Marco Del Castillo, A.; Jepsen, S.; Gonzalez-Juanatey, J.R.; D’Aiuto, F.; Bouchard, P.; Chapple, I.; Dietrich, T.; Gotsman, I.; Graziani, F.; et al. Periodontitis and Cardiovascular Diseases: Consensus Report. J. Clin. Periodontol. 2020, 47, 268–288. [Google Scholar] [CrossRef]
- Nazir, M.A. Prevalence of Periodontal Disease, Its Association with Systemic Diseases and Prevention. Int. J. Health Sci. 2017, 11, 72–80. [Google Scholar]
- Taylor, G.W. Bidirectional Interrelationships between Diabetes and Periodontal Diseases: An Epidemiologic Perspective. Ann. Periodontol. 2001, 6, 99–112. [Google Scholar] [CrossRef] [PubMed]
- DeBowes, L.J. The Effects of Dental Disease on Systemic Disease. Vet. Clin. N. Am. Small Anim. Pract. 1998, 28, 1057–1062. [Google Scholar] [CrossRef] [PubMed]
- Loos, B.G. Systemic Markers of Inflammation in Periodontitis. J. Periodontol. 2005, 76, 2106–2115. [Google Scholar] [CrossRef] [PubMed]
- Taylor, J.D. COPD and the Response of the Lung to Tobacco Smoke Exposure. Pulm. Pharmacol. Ther. 2010, 23, 376–383. [Google Scholar] [CrossRef] [PubMed]
- MacNee, W. Pathogenesis of Chronic Obstructive Pulmonary Disease. Proc. Am. Thorac. Soc. 2005, 2, 258–266. [Google Scholar] [CrossRef] [PubMed]
- Garmendia, J.; Morey, P.; Bengoechea, J.A. Impact of Cigarette Smoke Exposure on Host-Bacterial Pathogen Interactions. Eur. Respir. J. 2012, 39, 467–477. [Google Scholar] [CrossRef]
- Global Initiative for Chronic Obstructive Lung Disease (GOLD). Global Strategy for Prevention, Diagnosis and Management of Chronic Obstructive Pulmonary Disease; 2020 Report. Available online: https://www.goldcopd.org/ (accessed on 1 December 2023).
- Lokesh, K.S.; Chaya, S.K.; Jayaraj, B.S.; Praveena, A.S.; Krishna, M.; Madhivanan, P.; Mahesh, P.A. Vitamin D Deficiency Is Associated with Chronic Obstructive Pulmonary Disease and Exacerbation of COPD. Clin. Respir. J. 2021, 15, 389–399. [Google Scholar] [CrossRef]
- Bansal, M.; Khatri, M.; Taneja, V. Potential Role of Periodontal Infection in Respiratory Diseases—A Review. J. Med. Life 2013, 6, 244–248. [Google Scholar]
- Apessos, I.; Voulgaris, A.; Agrafiotis, M.; Andreadis, D.; Steiropoulos, P. Effect of Periodontal Therapy on COPD Outcomes: A Systematic Review. BMC Pulm. Med. 2021, 21, 92. [Google Scholar] [CrossRef]
- Prasanna, S. Causal Relationship between Periodontitis and Chronic Obstructive Pulmonary Disease. J. Indian Soc. Periodontol. 2011, 15, 359. [Google Scholar] [CrossRef] [PubMed]
- Mahesh, P.A.; Lokesh, K.S.; Madhivanan, P.; Chaya, S.K.; Jayaraj, B.S.; Ganguly, K.; Krishna, M. The Mysuru studies of Determinants of Health in Rural Adults (MUDHRA), India. Epidemiol. Health 2018, 40, e2018027. [Google Scholar] [CrossRef] [PubMed]
- Högman, M.; Sulku, J.; Ställberg, B.; Janson, C.; Bröms, K.; Hedenström, H.; Lisspers, K.; Malinovschi, A. 2017 Global Initiative for Chronic Obstructive Lung Disease Reclassifies Half of COPD Subjects to Lower Risk Group. Int. J. Chron. Obstruct. Pulm. Dis. 2018, 13, 165–173. [Google Scholar] [CrossRef] [PubMed]
- Page, R.C.; Eke, P.I. Case Definitions for Use in Population-Based Surveillance of Periodontitis. J. Periodontol. 2007, 78, 1387–1399. [Google Scholar] [CrossRef] [PubMed]
- Eke, P.I.; Page, R.C.; Wei, L.; Thornton-Evans, G.; Genco, R.J. Update of the Case Definitions for Population-Based Surveillance of Periodontitis. J. Periodontol. 2012, 83, 1449–1454. [Google Scholar] [CrossRef]
- Tonetti, M.S.; Greenwell, H.; Kornman, K.S. Staging and Grading of Periodontitis: Framework and Proposal of a New Classification and Case Definition. J. Periodontol. 2018, 89, S159–S172. [Google Scholar] [CrossRef] [PubMed]
- Silness, J.; Löe, H. Periodontal Disease in Pregnancy II. Correlation between Oral Hygiene and Periodontal Condition. Acta Odontol. Scand. 1964, 22, 121–135. [Google Scholar] [CrossRef]
- Soriano, J.B.; Rodriguez-Roisin, R. Chronic Obstructive Pulmonary Disease Overview: Epidemiology, Risk Factors, and Clinical Presentation. Proc. Am. Thorac. Soc. 2011, 8, 363–367. [Google Scholar] [CrossRef]
- Peter, K.P.; Mute, B.R.; Doiphode, S.S.; Bardapurkar, S.J.; Borkar, M.S.; Raje, D.V. Association between Periodontal Disease and Chronic Obstructive Pulmonary Disease: A Reality or Just a Dogma? J. Periodontol. 2013, 84, 1717–1723. [Google Scholar] [CrossRef]
- Nayak, R.; Spoorthi, B.; Vadiraj, S.; Choudhary, G.K.; Kudyar, N. Periodontal Pathogens and Respiratory Diseases—Evaluating Their Potential Association: A Clinical and Microbiological Study. J. Contemp. Dent. Pract. 2013, 14, 610–615. [Google Scholar] [CrossRef]
- Barros, S.P.; Suruki, R.; Loewy, Z.G.; Beck, J.D.; Offenbacher, S. A Cohort Study of the Impact of Tooth Loss and Periodontal Disease on Respiratory Events among COPD Subjects: Modulatory Role of Systemic Biomarkers of Inflammation. PLoS ONE 2013, 8, e68592. [Google Scholar] [CrossRef]
- Offenbacher, S.; Barros, S.P.; Altarawneh, S.; Beck, J.D.; Loewy, Z.G. Impact of Tooth Loss on Oral and Systemic Health. Gen. Dent. 2012, 60, 494–500. [Google Scholar] [PubMed]
- Shi, Q.; Zhang, B.; Xing, H.; Yang, S.; Xu, J.; Liu, H. Patients with Chronic Obstructive Pulmonary Disease Suffer from Worse Periodontal Health-Evidence from a Meta-Analysis. Front. Physiol. 2018, 9, 33. [Google Scholar] [CrossRef] [PubMed]
- Lopez-de-Andrés, A.; Vazquez-Vazquez, L.; Martinez-Huedo, M.A.; Hernández-Barrera, V.; Jimenez-Trujillo, I.; Tapias-Ledesma, M.A.; De Miguel-Diez, J.; Jiménez-Garcia, R. Is COPD Associated with Periodontal Disease? A Population-Based Study in Spain. Int. J. Chron. Obstruct. Pulm. Dis. 2018, 13, 3435–3445. [Google Scholar] [CrossRef]
- Zhong, Y.; Slade, G.D.; Beck, J.D.; Offenbacher, S. Gingival Crevicular Fluid Interleukin-1?, Prostaglandin E2 and Periodontal Status in a Community Population. J. Clin. Periodontol. 2007, 34, 285–293. [Google Scholar] [CrossRef]
- Engebretson, S.P.; Grbic, J.T.; Singer, R.; Lamster, I.B. GCF IL-1β Profiles in Periodontal Disease: GCF IL-1β Profiles in Periodontal Disease. J. Clin. Periodontol. 2002, 29, 48–53. [Google Scholar] [CrossRef]
- Kornman, K.S.; Page, R.C.; Tonetti, M.S. The Host Response to the Microbial Challenge in Periodontitis: Assembling the Players. Periodontology 2000 1997, 14, 33–53. [Google Scholar] [CrossRef]
- Cardoso, E.M.; Reis, C.; Manzanares-Céspedes, M.C. Chronic Periodontitis, Inflammatory Cytokines, and Interrelationship with Other Chronic Diseases. Postgrad. Med. 2018, 130, 98–104. [Google Scholar] [CrossRef]
- Hobbins, S.; Chapple, I.; Sapey, E.; Stockley, R. Is Periodontitis a Comorbidity of COPD or Can Associations Be Explained by Shared Risk Factors/Behaviors? Int. J. Chron. Obstruct. Pulm. Dis. 2017, 12, 1339–1349. [Google Scholar] [CrossRef]
- Takeuchi, K.; Matsumoto, K.; Furuta, M.; Fukuyama, S.; Takeshita, T.; Ogata, H.; Suma, S.; Shibata, Y.; Shimazaki, Y.; Hata, J.; et al. Periodontitis Is Associated with Chronic Obstructive Pulmonary Disease. J. Dent. Res. 2019, 98, 534–540. [Google Scholar] [CrossRef]
- Kaleem Ullah, M.; Parthasarathi, A.; Biligere Siddaiah, J.; Vishwanath, P.; Upadhyay, S.; Ganguly, K.; Anand Mahesh, P. Impact of Acute Exacerbation and Its Phenotypes on the Clinical Outcomes of Chronic Obstructive Pulmonary Disease in Hospitalized Patients: A Cross-Sectional Study. Toxics 2022, 10, 667. [Google Scholar] [CrossRef] [PubMed]
- Shen, T.-C.; Chang, P.-Y.; Lin, C.-L.; Chen, C.-H.; Tu, C.-Y.; Hsia, T.-C.; Shih, C.-M.; Hsu, W.-H.; Sung, F.-C.; Kao, C.-H. Risk of Periodontal Diseases in Patients with Chronic Obstructive Pulmonary Disease: A Nationwide Population-Based Cohort Study. Medicine 2015, 94, e2047. [Google Scholar] [CrossRef] [PubMed]
- Jung, E.S.; Lee, K.H.; Choi, Y.Y. Association between Oral Health Status and Chronic Obstructive Pulmonary Disease in Korean Adults. Int. Dent. J. 2020, 70, 208–213. [Google Scholar] [CrossRef]
- Tamiya, H.; Mitani, A.; Abe, M.; Nagase, T. Putative Bidirectionality of Chronic Obstructive Pulmonary Disease and Periodontal Disease: A Review of the Literature. J. Clin. Med. 2023, 12, 5935. [Google Scholar] [CrossRef] [PubMed]
- Javaheri, N.; Matin, S.; Naghizadeh-Baghi, A.; Bagheri, A.; Andreasian, A.; Ghobadi, H. Periodontal Status, Its Treatment Needs, and Its Relationship with Airflow Limitation and Quality of Life in COPD Patients. Eurasian J. Med. 2020, 52, 259–264. [Google Scholar] [CrossRef] [PubMed]
- Tan, L.; Tang, X.; Pan, C.; Wang, H.; Pan, Y. Relationship among Clinical Periodontal, Microbiologic Parameters and Lung Function in Participants with Chronic Obstructive Pulmonary Disease. J. Periodontol. 2019, 90, 134–140. [Google Scholar] [CrossRef] [PubMed]
- Si, Y.; Fan, H.; Song, Y.; Zhou, X.; Zhang, J.; Wang, Z. Association Between Periodontitis and Chronic Obstructive Pulmonary Disease in a Chinese Population. J. Periodontol. 2012, 83, 1288–1296. [Google Scholar] [CrossRef]
- Zhou, X.; Han, J.; Liu, Z.; Song, Y.; Wang, Z.; Sun, Z. Effects of Periodontal Treatment on Lung Function and Exacerbation Frequency in Patients with Chronic Obstructive Pulmonary Disease and Chronic Periodontitis: A 2-Year Pilot Randomized Controlled Trial. J. Clin. Periodontol. 2014, 41, 564–572. [Google Scholar] [CrossRef]
- Scannapieco, F.A.; Wang, B.; Shiau, H.J. Oral Bacteria and Respiratory Infection: Effects on Respiratory Pathogen Adhesion and Epithelial Cell Proinflammatory Cytokine Production. Ann. Periodontol. 2001, 6, 78–86. [Google Scholar] [CrossRef]
- Kaleem Ullah, M.; Malamardi, S.; Siddaiah, J.B.; A, T.; Prashant, A.; Vishwanath, P.; Riley, L.W.; Madhivanan, P.; Mahesh, P.A. Trends in the Bacterial Prevalence and Antibiotic Resistance Patterns in the Acute Exacerbation of Chronic Obstructive Pulmonary Disease in Hospitalized Patients in South India. Antibiotics 2022, 11, 1577. [Google Scholar] [CrossRef]
- Usher, A.K.; Stockley, R.A. The Link between Chronic Periodontitis and COPD: A Common Role for the Neutrophil? BMC Med. 2013, 11, 241. [Google Scholar] [CrossRef] [PubMed]
- Tan, L.; Wang, H.; Li, C.; Pan, Y. 16S rDNA-Based Metagenomic Analysis of Dental Plaque and Lung Bacteria in Patients with Severe Acute Exacerbations of Chronic Obstructive Pulmonary Disease. J. Periodontal Res. 2014, 49, 760–769. [Google Scholar] [CrossRef] [PubMed]
- Madalli, R.; Kheur, S.; Reddy, M.G.; Kheur, M.; Mahalle, A. Assessment of Role of Porphyromonas Gingivalis as an Aggravating Factor for Chronic Obstructive Pulmonary Disease Patients with Periodontitis. Dent. Hypotheses 2016, 7, 100. [Google Scholar] [CrossRef]
- Agado, B.; Bowen, D. Does the Link Between COPD and Periodontitis Affect Dental Hygiene Treatment? Access 2009, 23, 19–21. [Google Scholar]
- Deo, V.; Bhongade, M.; Ansari, S.; Chavan, R. Periodontitis as a Potential Risk Factor for Chronic Obstructive Pulmonary Disease: A Retrospective Study. Indian J. Dent. Res. 2009, 20, 466. [Google Scholar] [CrossRef] [PubMed]
- Mannino, D.M.; Homa, D.M.; Akinbami, L.J.; Ford, E.S.; Redd, S.C. Chronic Obstructive Pulmonary Disease Surveillance—United States, 1971–2000. Morb. Mortal. Wkly. Rep. Surveill. Summ. 2002, 51, 1–16. [Google Scholar]
- Wagner, E.H. Chronic Disease Care. BMJ 2004, 328, 177–178. [Google Scholar] [CrossRef] [PubMed]
- Chowdhury, M.Z.I.; Turin, T.C. Variable Selection Strategies and Its Importance in Clinical Prediction Modelling. Fam. Med. Community Health 2020, 8, e000262. [Google Scholar] [CrossRef]
- Hyman, J.J.; Reid, B.C. Cigarette Smoking, Periodontal Disease: And Chronic Obstructive Pulmonary Disease. J. Periodontol. 2004, 75, 9–15. [Google Scholar] [CrossRef]
- Scannapieco, F.A.; Ho, A.W. Potential Associations Between Chronic Respiratory Disease and Periodontal Disease: Analysis of National Health and Nutrition Examination Survey III. J. Periodontol. 2001, 72, 50–56. [Google Scholar] [CrossRef]
- Harland, J.; Furuta, M.; Takeuchi, K.; Tanaka, S.; Yamashita, Y. Periodontitis Modifies the Association between Smoking and Chronic Obstructive Pulmonary Disease in Japanese Men. J. Oral Sci. 2018, 60, 226–231. [Google Scholar] [CrossRef]
- Kim, S.W.; Han, K.; Kim, S.Y.; Park, C.K.; Rhee, C.K.; Yoon, H.K. The Relationship between the Number of Natural Teeth and Airflow Obstruction: A Cross-Sectional Study Using Data from the Korean National Health and Nutrition Examination Survey. Int. J. Chron. Obstruct. Pulm. Dis. 2015, 13, 13–21. [Google Scholar] [CrossRef] [PubMed]
- Gupta, I.; Patel, S.A.; Kondal, D.; Goodman, M.; Mohan, S.; Ali, M.K.; Tandon, N.; Narayan, K.M.V.; Prabhakaran, D.; Shridhar, K. Epidemiological Pattern of COVID-19 and Its Association with Periodontal Health in an Urban Indian Cohort. Front. Public Health 2023, 11, 1108465. [Google Scholar] [CrossRef] [PubMed]
- Costa, C.A.; Vilela, A.C.S.; Oliveira, S.A.; Gomes, T.D.; Andrade, A.A.C.; Leles, C.R.; Costa, N.L. Poor Oral Health Status and Adverse COVID-19 Outcomes: A Preliminary Study in Hospitalized Patients. J. Periodontol. 2022, 93, 1889–1901. [Google Scholar] [CrossRef] [PubMed]
- Gupta, S.; Sorsa, T.; Brandt, E.; Räisänen, I.T.; Mohindra, R.; Goyal, K. Poor Oral Health May Prolong COVID-19 Illness. J. Transl. Med. 2022, 20, 113. [Google Scholar] [CrossRef]
- Baima, G.; Marruganti, C.; Sanz, M.; Aimetti, M.; Romandini, M. Periodontitis and COVID-19: Biological Mechanisms and Meta-Analyses of Epidemiological Evidence. J. Dent. Res. 2022, 101, 1430–1440. [Google Scholar] [CrossRef]
- Tamimi, F.; Altigani, S.; Sanz, M. Periodontitis and Coronavirus Disease 2019. Periodontology 2000 2022, 89, 207–214. [Google Scholar] [CrossRef]
- Wang, Y.; Deng, H.; Pan, Y.; Jin, L.; Hu, R.; Lu, Y.; Deng, W.; Sun, W.; Chen, C.; Shen, X.; et al. Periodontal Disease Increases the Host Susceptibility to COVID-19 and Its Severity: A Mendelian Randomization Study. J. Transl. Med. 2021, 19, 528. [Google Scholar] [CrossRef]






| Total (N = 199) | GOLD Grade | |||||
|---|---|---|---|---|---|---|
| 1 (N = 22) | 2 (N = 75) | 3 (N = 88) | 4 (N = 14) | p-Value | ||
| Age | 64.5 ± 8.8 | 59.2 ± 11.2 | 66.8 ± 8.5 | 64.3 ± 8.1 | 61.4 ± 4.6 | 0.001 1 |
| Occupation | <0.001 2 | |||||
| Farmer | 72 (36.2) | 11 (50.0) | 30 (40.0) | 22 (25.0) | 9 (64.3) | |
| Retired farmer | 104 (52.3) | 9 (40.9) | 37 (49.3) | 57 (64.8) | 1 (7.1) | |
| Others | 23 (11.6) | 2 (9.1) | 8 (10.7) | 9 (10.2) | 4 (28.6) | |
| Smoking Type | 0.037 2 | |||||
| Beedi | 151 (75.9) | 21 (95.5) | 53 (70.7) | 67 (76.1) | 10 (71.4) | |
| Cigarette | 32 (16.1) | 0 (0.0) | 19 (25.3) | 11 (12.5) | 2 (14.3) | |
| Both | 16 (8.0) | 1 (4.5) | 3 (4.0) | 10 (11.4) | 2 (14.3) | |
| Smoking Pack-Years | 39.9 ± 35 | 27.5 ± 19 | 33.3 ± 24 | 47.4 ± 45 | 48.1 ± 25 | 0.016 1 |
| FVC % Pred # | 73.8 ± 20 | 105.2 ± 7 | 83.6 ± 11 | 61.8 ± 12 | 46.9 ± 18 | <0.001 1 |
| FEV1 % Pred # | 53.3 ± 19 | 88.5 ± 6 | 64.1 ± 8 | 39.8 ± 6 | 25.4 ± 3 | <0.001 1 |
| FEV1/FVC Ratio # | 56.3 ± 10 | 66.3 ± 3 | 60.5 ± 7 | 50.7 ± 9 | 53.3 ± 8 | <0.001 1 |
| SGRQ-C Total % | 34.6 ± 15 | 27.6 ± 16 | 32.3 ± 15 | 38.8 ± 13 | 32.1 ± 13 | 0.002 1 |
| 6MWD % | 79.6 ± 13 | 82.8 ± 11 | 81.0 ± 13 | 78.8 ± 13 | 72.1 ± 16 | 0.064 1 |
| Tooth loss | 5.6 ± 1.1 | 4.0 ± 0.7 | 5.0 ± 0.1 | 6.2 ± 0.6 | 7.8 ± 1.1 | <0.001 1 |
| Tooth present | 23.0 ± 2.1 | 27.1 ± 1.5 | 23.6 ± 1.1 | 21.9 ± 0.9 | 20.2 ± 1.1 | <0.001 1 |
| Periodontal Severity | <0.001 2 | |||||
| None | 14 (7.0) | 14 (63.6) | 0 (0) | 0 (0) | 0 (0) | |
| Mild | 28 (14.1) | 8 (36.4) | 20 (26.7) | 0 (0) | 0 (0) | |
| Moderate | 50 (25.1) | 0 (0) | 48 (64.0) | 2 (2.3) | 0 (0) | |
| Severe | 107 (53.8) | 0 (0) | 7 (9.3) | 86 (97.7) | 14 (100) | |
| Presence of Exacerbation in Last Year | <0.001 2 | |||||
| No | 6 (3.0) | 6 (27.3) | 0 (0.0) | 0 (0.0) | 0 (0.0) | |
| Yes | 193 (97.0) | 16 (72.7) | 75 (100.0) | 88 (100.0) | 14 (100.0) | |
| Number of Exacerbations | ||||||
| Mean ± SD | 2.3 ± 1 | 0.9 ± 0.6 | 1.3 ± 0.5 | 3.1 ± 0.6 | 4.8 ± 0.7 | <0.001 1 |
| Median (IQR) | 2 (1–3) | 1 (0–1) | 1 (1–2) | 3 (3–3) | 5 (4–5) | <0.001 1 |
| Presence of Hospitalization in Last Year | 0.027 2 | |||||
| No | 132 (66.3) | 16 (72.7) | 56 (74.7) | 55 (62.5) | 5 (35.7) | |
| Yes | 67 (33.7) | 6 (27.3) | 19 (25.3) | 33 (37.5) | 9 (64.3) | |
| Model 1 | Model 2 | |
|---|---|---|
| Age | 0.002 (−0.003–0.007) | −0.007 (−0.017–0.003) |
| Smoking Pack-Years | −0.000 (−0.001–0.001) | 0.003 (0.0002–0.005) * |
| SGRQ_C Total Percentage | −0.002 (−0.005–0.001) | 0.006 (−0.000–0.012) * |
| Periodontal Severity: | ||
| Severe | 1.273 (1.043–1.502) *** | 0.130 (−0.436–0.696) |
| Mild | 0.556 (0.355–0.757) *** | −0.344 (−0.761–0.072) |
| Moderate | 0.808 (0.618–0.998) *** | −0.474 (−0.899-−0.048) * |
| Exacerbation | 0.309 (0.250–0.368) *** | - |
| GOLD Stage | - | 1.159 (0.938–1.381) *** |
| Total (N = 199) | GOLD Grade | p-Value | ||||
|---|---|---|---|---|---|---|
| 1 (N = 22) | 2 (N = 75) | 3 (N = 88) | 4 (N = 14) | |||
| PPD | ||||||
| Mean ± SD | 5.4 ± 1.5 | 2.3 ± 0.9 | 4.9 ± 0.3 | 6.2 ± 0.7 | 7.7 ± 0.7 | <0.001 1 |
| Median (IQR) | 5 (5–6) | 3 (1–3) | 5 (5–5) | 6 (6–7) | 8 (7–8) | <0.001 2 |
| PI | ||||||
| Mean ± SD | 2.3 ± 0.5 | 1.3 ± 0.5 | 2.2 ± 0.1 | 2.5 ± 0.2 | 2.9 ± 0.1 | <0.001 1 |
| Median (IQR) | 2.3 (2.2–2.5) | 1 (0.9–1.7) | 2.2 (2.2–2.3) | 2.4 (2.4–2.8) | 2.9 (2.8–2.9) | <0.001 2 |
| CAL | ||||||
| Mean ± SD | 4.8 ± 2.1 | 0.6 ± 0.8 | 4.0 ± 1.3 | 6.2 ± 0.5 | 7.5 ± 0.5 | <0.001 1 |
| Median (IQR) | 6 (4–6) | 0(0–1) | 4 (3–5) | 6 (6–6) | 7.5 (7–8) | <0.001 2 |
| Risk Factors for Severity of Airflow Limitation | Model 1 | Model 2 | Model 3 | Model 4 |
|---|---|---|---|---|
| Age | 0.0002 (−0.005–0.005) | 0.0003 (−0.0050–0.0056) | 0.0006 (−0.0045–0.0057) | −0.001 (−0.005–0.004) |
| Smoking Pack-Years | 0.00003 (−0.001–0.001) | 0.0001 (−0.0013–0.0014) | 0.0001 (−0.0012–0.0014) | 0.000 (−0.001–0.001) |
| SGRQ-C Total Percentage | −0.0004 (−0.003–0.003) | 0.0001 (−0.0031–0.0032) | −0.002 (−0.0051–0.0011) | −0.002 (−0.004–0.001) |
| Number of Exacerbations in last year | 0.263 (0.207–0.319) *** | 0.351 (0.298–0.403) *** | 0.281 (0.221–0.340) *** | 0.177 (0.119–0.236) *** |
| PPD | 0.288 (0.241–0.334) *** | - | - | 0.280 (0.196–0.364) *** |
| PI | - | 0.718 (0.574–0.861) *** | - | −0.319 (−0.584–−0.054) ** |
| CAL | - | - | 0.193 (0.157–0.228) *** | 0.132 (0.091–0.174) *** |
| Risk Factors for Number of Exacerbations during Last Year | Model 1 | Model 2 | Model 3 | Model 4 |
| Age | −0.012 (−0.022–−0.001) * | −0.011 (−0.021–−0.001) * | −0.012 (−0.022–−0.002) * | −0.011 (−0.021–−0.001) * |
| Smoking Pack-Years | 0.003 (0.000–0.005) * | 0.003 (0.000–0.005) * | 0.003 (0.000–0.005) * | 0.003 (0.000–0.005) * |
| SGRQ-C Total Percentage | 0.007 (0.001–0.013) * | 0.007 (0.001–0.013) * | 0.006 (−0.000–0.012) | 0.004 (−0.002–0.010) |
| GOLD Stage | 1.173 (0.924–1.422) | 1.349 (1.146–1.551) *** | 1.114 (0.879–1.348) *** | 0.892 (0.598–1.186) *** |
| PPD | 0.115 (−0.015–0.244) *** | - | - | 0.316 (0.112–0.519) ** |
| PI | - | 0.041 (−0.304–0.385) | - | −0.911 (−1.500–−0.323) ** |
| CAL | - | - | 0.109 (0.021–0.196) * | 0.161 (0.062–0.260) ** |
| Model | Model 1 | Model 2 | Model 3 |
|---|---|---|---|
| Variable | OR (CI) | OR (CI) | OR (CI) |
| Age | 0.98 (0.94–1.01) | 0.97 (0.94–1.01) | 0.98 (0.95–1.02) |
| Smoking Pack-Years | 1.0 (0.99–1.02) | 1.0 (0.99–1.02) | 1.0 (0.99–1.02) |
| SGRQ-C Total % | 1.0 (0.98–1.02) | 1.0 (0.97–1.02) | 0.99 (0.97–1.02) |
| PPD | 1.29 (1.03–1.62) * | - | - |
| PI | - | 3.04 (1.28–7.2) * | - |
| CAL | - | - | 1.26 (1.06–1.49) ** |
| Variable | Model 1 | Model 2 | Model 3 |
|---|---|---|---|
| Age | −0.002 (−0.013–0.008) | −0.001 (−0.005–0.002) | 0 (−0.016–0.016) |
| Smoking Pack-Years | 0 (−0.002–0.003) | 0 (−0.001–0.001) | −0.001 (−0.004–0.003) |
| GOLD Stage | |||
| 2–1 | 2.678 (2.375–2.981) *** | 0.969 (0.866–1.072) *** | 3.339 (2.875–3.802) *** |
| 3–1 | 3.984 (3.688–4.279) *** | 1.251 (1.15–1.352) *** | 5.589 (5.137–6.042) *** |
| 4–1 | 5.44 (5.024–5.857) *** | 1.578 (1.436–1.72) *** | 6.874 (6.237–7.511) *** |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Subbappa, A.; Lokesh, K.S.; Chaya, S.K.; Kaleem Ullah, M.; Siddaiah, J.B.; Bhojraj, N.; Mahesh, P.A. Unmasking the Silent Threat: Periodontal Health’s Impact on COPD Severity and Hospitalization. J. Pers. Med. 2023, 13, 1714. https://doi.org/10.3390/jpm13121714
Subbappa A, Lokesh KS, Chaya SK, Kaleem Ullah M, Siddaiah JB, Bhojraj N, Mahesh PA. Unmasking the Silent Threat: Periodontal Health’s Impact on COPD Severity and Hospitalization. Journal of Personalized Medicine. 2023; 13(12):1714. https://doi.org/10.3390/jpm13121714
Chicago/Turabian StyleSubbappa, Anitha, Komarla Sundararaja Lokesh, Sindaghatta Krishnarao Chaya, Mohammed Kaleem Ullah, Jayaraj Biligere Siddaiah, Nandlal Bhojraj, and Padukudru Anand Mahesh. 2023. "Unmasking the Silent Threat: Periodontal Health’s Impact on COPD Severity and Hospitalization" Journal of Personalized Medicine 13, no. 12: 1714. https://doi.org/10.3390/jpm13121714
APA StyleSubbappa, A., Lokesh, K. S., Chaya, S. K., Kaleem Ullah, M., Siddaiah, J. B., Bhojraj, N., & Mahesh, P. A. (2023). Unmasking the Silent Threat: Periodontal Health’s Impact on COPD Severity and Hospitalization. Journal of Personalized Medicine, 13(12), 1714. https://doi.org/10.3390/jpm13121714