Supervised Pelvic Floor Muscle Training Improves Sexual Function and Diminishes Sexual Distress in Women with Relapsing–Remitting Multiple Sclerosis: A Randomised Controlled Study
Abstract
:1. Introduction
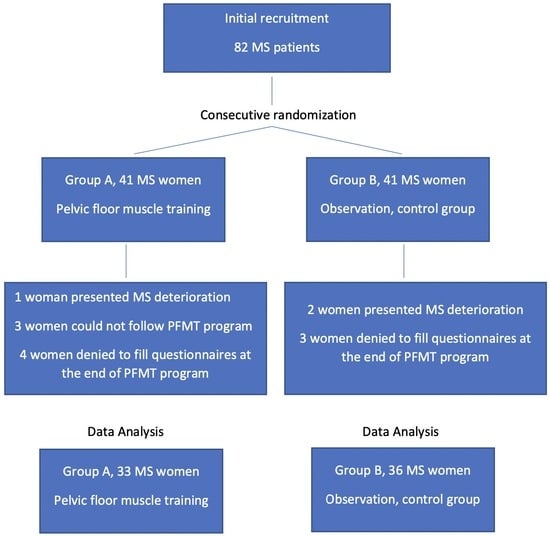
2. Materials and Methods
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Laumann, E.O.; Paik, A.; Rosen, R.C. Sexual dysfunction in the United States: Prevalence and predictors. JAMA 1999, 281, 537–544. [Google Scholar] [CrossRef]
- Stephenson, K.R.; Meston, C.M. Why is impaired sexual function distressing to women? The primacy of pleasure in female sexual dysfunction. J. Sex. Med. 2015, 12, 728–737. [Google Scholar] [CrossRef] [PubMed]
- Khajehei, M.; Doherty, M.; Tilley, P.J. An update on sexual function and dysfunction in women. Arch. Womens Ment. Health 2015, 18, 423–433. [Google Scholar] [CrossRef] [PubMed]
- Drulovic, J.; Kisic-Tepavcevic, D.; Pekmezovic, T. Epidemiology, diagnosis and management of sexual dysfunction in multiple sclerosis. Acta Neurol. Belg. 2020, 120, 791–797. [Google Scholar] [CrossRef] [PubMed]
- Schairer, L.C.; Foley, F.W.; Zemon, V.; Tyry, T.; Campagnolo, D.; Marrie, R.A.; Gromisch, E.S.; Schairer, D. The impact of sexual dysfunction on health-related quality of life in people with multiple sclerosis. Mult. Scler. 2014, 20, 610–616. [Google Scholar] [CrossRef] [PubMed]
- Yazdani, A.; Ebrahimi, N.; Mirmosayyeb, O.; Ghajarzadeh, M. Prevalence and risk of developing sexual dysfunction in women with multiple sclerosis (MS): A systematic review and meta-analysis. BMC Womens Health 2023, 23, 352. [Google Scholar] [CrossRef] [PubMed]
- Bronner, G.; Elran, E.; Golomb, J.; Korczyn, A.D. Female sexuality in multiple sclerosis: The multidimensional nature of the problem and the intervention. Acta Neurol. Scand. 2010, 121, 289–301. [Google Scholar] [CrossRef]
- Tzortzis, V.; Skriapas, K.; Hadjigeorgiou, G.; Mitsogiannis, I.; Aggelakis, K.; Gravas, S.; Poulakis, V.; Melekos, M.D. Sexual dysfunction in newly diagnosed multiple sclerosis women. Mult. Scler. 2008, 14, 561–563. [Google Scholar] [CrossRef]
- Kisic-Tepavcevic, D.; Pekmezovic, T.; Trajkovic, G.; Stojsavljevic, N.; Dujmovic, I.; Mesaros, S.; Drulovic, J. Sexual dysfunction in multiple sclerosis: A 6-year follow-up study. J. Neurol. Sci. 2015, 358, 317–323. [Google Scholar] [CrossRef]
- DasGupta, R.; Fowler, C.J. Bladder, bowel and sexual dysfunction in multiple sclerosis: Management strategies. Drugs 2003, 63, 153–166. [Google Scholar] [CrossRef]
- Dehghan-Nayeri, N.; Khakbazan, Z.; Ghafoori, F.; Nabavi, S.M. Sexual dysfunction levels in iranian women suffering from multiple sclerosis. Mult. Scler. Relat. Disord. 2017, 12, 49–53. [Google Scholar] [CrossRef] [PubMed]
- Zamani, M.; Tavoli, A.; Yazd Khasti, B.; Sedighimornani, N.; Zafar, M. Sexual Therapy for Women with Multiple Sclerosis and Its Impact on Quality of Life. Iran. J. Psychiatry 2017, 12, 58–65. [Google Scholar] [PubMed]
- Mahajan, S.T.; James, R.; Frasure, H. Pelvic floor disorders and multiple sclerosis: Are patients satisfied with their care? Int. J. MS Care 2014, 16, 20–25. [Google Scholar] [CrossRef]
- Omodei, M.S.; Marques Gomes Delmanto, L.R.; Carvalho-Pessoa, E.; Schmitt, E.B.; Nahas, G.P.; Petri Nahas, E.A. Association Between Pelvic Floor Muscle Strength and Sexual Function in Postmenopausal Women. J. Sex. Med. 2019, 16, 1938–1946. [Google Scholar] [CrossRef] [PubMed]
- Sapouna, V.; Thanopoulou, S.; Papriakas, D.; Papakosta, S.; Sakopoulou, M.; Zachariou, D.; Zikopoulos, A.; Kaltsas, A.; Vrachnis, N.; Vrachnis, D.; et al. Pelvic Floor Muscle Training and Its Benefits for Multiple Sclerosis Patients Suffering From Urinary Incontinence and Sexual Dysfunction. Cureus 2023, 15, e47086. [Google Scholar] [CrossRef] [PubMed]
- Mosalanejad, F.; Afrasiabifar, A.; Zoladl, M. Investigating the combined effect of pelvic floor muscle exercise and mindfulness on sexual function in women with multiple sclerosis: A randomized controlled trial. Clin. Rehabil. 2018, 32, 1340–1347. [Google Scholar] [CrossRef] [PubMed]
- Giannopapas, V.; Kitsos, D.; Tsogka, A.; Tzartos, J.S.; Paraskevas, G.; Tsivgoulis, G.; Voumvourakis, K.; Giannopoulos, S.; Bakalidou, D. Sexual dysfunction therapeutic approaches in patients with multiple sclerosis: A systematic review. Neurol. Sci. 2023, 44, 873–880. [Google Scholar] [CrossRef]
- Rosen, R.; Brown, C.; Heiman, J.; Leiblum, S.; Meston, C.; Shabsigh, R.; Ferguson, D.; D’Agostino, R., Jr. The Female Sexual Function Index (FSFI): A multidimensional self-report instrument for the assessment of female sexual function. J. Sex Marital Ther. 2000, 26, 191–208. [Google Scholar] [CrossRef]
- Zachariou, A.; Filiponi, M.; Kirana, P.S. Translation and validation of the Greek version of the female sexual function index questionnaire. Int. J. Impot. Res. 2017, 29, 171–174. [Google Scholar] [CrossRef]
- Derogatis, L.; Clayton, A.; Lewis-D’Agostino, D.; Wunderlich, G.; Fu, Y. Validation of the female sexual distress scale-revised for assessing distress in women with hypoactive sexual desire disorder. J. Sex. Med. 2008, 5, 357–364. [Google Scholar] [CrossRef]
- Aguilar-Zafra, S.; Del Corral, T.; Vidal-Quevedo, C.; Rodriguez-Duran, P.; Lopez-de-Uralde-Villanueva, I. Pelvic floor dysfunction negatively impacts general functional performance in patients with multiple sclerosis. Neurourol. Urodyn. 2020, 39, 978–986. [Google Scholar] [CrossRef] [PubMed]
- Dasgupta, R.; Wiseman, O.J.; Kanabar, G.; Fowler, C.J.; Mikol, D. Efficacy of sildenafil in the treatment of female sexual dysfunction due to multiple sclerosis. J. Urol. 2004, 171, 1189–1193; discussion 1193. [Google Scholar] [CrossRef] [PubMed]
- Delaney, K.E.; Donovan, J. Multiple sclerosis and sexual dysfunction: A need for further education and interdisciplinary care. NeuroRehabilitation 2017, 41, 317–329. [Google Scholar] [CrossRef] [PubMed]
- Orasanu, B.; Frasure, H.; Wyman, A.; Mahajan, S.T. Sexual dysfunction in patients with multiple sclerosis. Mult. Scler. Relat. Disord. 2013, 2, 117–123. [Google Scholar] [CrossRef]
- Polat Dunya, C.; Tulek, Z.; Kurtuncu, M.; Gunduz, T.; Panicker, J.N.; Eraksoy, M. Evaluating the effects of transcutaneous tibial nerve stimulation or pelvic floor muscle training on sexual dysfunction in female multiple sclerosis patients reporting overactive bladder. Neurourol. Urodyn. 2021, 40, 1661–1669. [Google Scholar] [CrossRef] [PubMed]
- Drulovic, J.; Pekmezovic, T.; Matejic, B.; Mesaros, S.; Manigoda, M.; Dujmovic, I.; Stojsavljevic, N.; Kocev, N.; Gavric-Kezic, M.; Nikic, P.; et al. Quality of life in patients with multiple sclerosis in Serbia. Acta Neurol. Scand. 2007, 115, 147–152. [Google Scholar] [CrossRef]
- Lucio, A.C.; D’Ancona, C.A.; Lopes, M.H.; Perissinotto, M.C.; Damasceno, B.P. The effect of pelvic floor muscle training alone or in combination with electrostimulation in the treatment of sexual dysfunction in women with multiple sclerosis. Mult. Scler. 2014, 20, 1761–1768. [Google Scholar] [CrossRef]
- Zahariou, A.G.; Karamouti, M.V.; Papaioannou, P.D. Pelvic floor muscle training improves sexual function of women with stress urinary incontinence. Int. Urogynecol. J. Pelvic Floor Dysfunct. 2008, 19, 401–406. [Google Scholar] [CrossRef]
- Sparaco, M.; Bonavita, S. Pelvic Floor Dysfunctions and Their Rehabilitation in Multiple Sclerosis. J. Clin. Med. 2022, 11, 1941. [Google Scholar] [CrossRef]
- Altunan, B.; Gundogdu, A.A.; Ozcaglayan, T.I.K.; Unal, A.; Turgut, N. The effect of pelvic floor exercise program on incontinence and sexual dysfunction in multiple sclerosis patients. Int. Urol. Nephrol. 2021, 53, 1059–1065. [Google Scholar] [CrossRef]
- Lowenstein, L.; Gruenwald, I.; Gartman, I.; Vardi, Y. Can stronger pelvic muscle floor improve sexual function? Int. Urogynecol. J. 2010, 21, 553–556. [Google Scholar] [CrossRef] [PubMed]
- Gopal, A.; Sydow, R.; Block, V.; Allen, D.D. Effectiveness of Physical Therapy in Addressing Sexual Dysfunction in Individuals with Multiple Sclerosis: A Systematic Review and Meta-analysis. Int. J. MS Care 2021, 23, 213–222. [Google Scholar] [CrossRef] [PubMed]
- Hwang, U.J.; Lee, M.S.; Jung, S.H.; Ahn, S.H.; Kwon, O.Y. Pelvic Floor Muscle Parameters Affect Sexual Function After 8 Weeks of Transcutaneous Electrical Stimulation in Women with Stress Urinary Incontinence. Sex. Med. 2019, 7, 505–513. [Google Scholar] [CrossRef]
- Dantzer, R. Cytokine, sickness behavior, and depression. Immunol. Allergy Clin. N. Am. 2009, 29, 247–264. [Google Scholar] [CrossRef] [PubMed]
- Alba Pale, L.; Leon Caballero, J.; Samso Buxareu, B.; Salgado Serrano, P.; Perez Sola, V. Systematic review of depression in patients with multiple sclerosis and its relationship to interferonbeta treatment. Mult. Scler. Relat. Disord. 2017, 17, 138–143. [Google Scholar] [CrossRef] [PubMed]
- Persson, R.; Lee, S.; Yood, M.U.; Wagner, M.R.; Minton, N.; Niemcryk, S.; Lindholm, A.; Evans, A.M.; Jick, S. Incident depression in patients diagnosed with multiple sclerosis: A multi-database study. Eur. J. Neurol. 2020, 27, 1556–1560. [Google Scholar] [CrossRef]
- Ferreira, A.P.; Pegorare, A.B.; Salgado, P.R.; Casafus, F.S.; Christofoletti, G. Impact of a Pelvic Floor Training Program Among Women with Multiple Sclerosis: A Controlled Clinical Trial. Am. J. Phys. Med. Rehabil. 2016, 95, 1–8. [Google Scholar] [CrossRef] [PubMed]
- Sadeghi Bahmani, D.; Motl, R.W. Rate, burden, and treatment of sexual dysfunction in multiple sclerosis: The case for exercise training as a new treatment approach. Mult. Scler. Relat. Disord. 2021, 51, 102878. [Google Scholar] [CrossRef]
- Lensch, E.; Jost, W.H. Autonomic disorders in multiple sclerosis. Autoimmune Dis. 2011, 2011, 803841. [Google Scholar] [CrossRef]
- Gott, M.; Galena, E.; Hinchliff, S.; Elford, H. “Opening a can of worms”: GP and practice nurse barriers to talking about sexual health in primary care. Fam. Pract. 2004, 21, 528–536. [Google Scholar] [CrossRef]
- Proietti, S.; Giannantoni, A.; Sahai, A.; Khan, M.S.; Dasgupta, P. Overactive bladder and sexual function: A nightmare couple. BJU Int. 2012, 110, 921–924. [Google Scholar] [CrossRef] [PubMed]
| Inclusion Criteria | Exclusion Criteria |
|---|---|
| 18 years of age or older | Previous pelvic floor muscle training program |
| Diagnosis of relapsing–remitting MS | Ongoing pregnancy |
| Stable condition for a minimum period of six months | Child delivery within the previous six months |
| Kurtzke’s Expanded Disability Status Scale (EDSS) score < 4 | Urinary or faecal incontinence |
| Women sexually active for at least four weeks | Pelvic organ prolapses greater than stage I |
| Cognitive ability to complete the questionnaires and study protocol | Perimenopause or menopause period |
| Ability to contract PFM evaluated by the primary investigator |
| Variables | Groups | p Value | |
|---|---|---|---|
| PFMT Group A, 33 pts | Control Group B, 36 pts | ||
| Mean Age (years) ± SD | 38.1 ± 3.2 | 39.3 ± 5.1 | p > 0.05 |
| Mean Duration of MS (years) ± SD | 8.1 ± 2.6 | 7.5 ± 2.3 | p > 0.05 |
| Mean Age of MS Diagnosis (years) ± SD | 32.0 ± 2.5 | 30.8 ± 2.9 | p > 0.05 |
| Mean EDSS ± SD | 2.3 ± 0.9 | 2.1 ± 1.0 | p > 0.05 |
| Domain | Group A | Group B | p Value |
|---|---|---|---|
| Patients’ evaluation at the beginning of this study | |||
| Desire | 2.97 ± 0.2 | 2.85 ± 0.29 | p > 0.05 |
| Arousal | 3.91 ± 0.49 | 3.81 ± 0.41 | p > 0.05 |
| Lubrication | 3.67 ± 0.40 | 3.78 ± 0.48 | p > 0.05 |
| Orgasm | 3.79 ± 0.39 | 3.90 ± 0.35 | p > 0.05 |
| Satisfaction | 3.76 ± 0.35 | 3.92 ± 0.37 | p > 0.05 |
| Pain | 4.07 ± 0.44 | 4.26 ± 0.42 | p > 0.05 |
| Total FSFI score | 22.17 ± 1.74 | 22.52 ± 1.93 | p > 0.05 |
| FSDS-R | 9.62 ± 4.37 | 9.44 ± 4.01 | p > 0.05 |
| Patients’ evaluation at the end of this study | |||
| Desire | 3.54 ± 0.28 | 2.94 ± 0.25 | p = 0.02 |
| Arousal | 4.33 ± 0.49 | 3.92 ± 0.47 | p = 0.03 |
| Lubrication | 4.81 ± 0.46 | 3.82 ± 0.44 | p = 0.04 |
| Orgasm | 4.91 ± 0.57 | 3.93 ± 0.38 | p = 0.03 |
| Satisfaction | 5.01 ± 0.56 | 3.96 ± 0.39 | p = 0.01 |
| Pain | 4.42 ± 0.42 | 4.31 ± 0.41 | p > 0.05 |
| Total FSFI score | 27.02 ± 1.87 | 22.88 ± 1.81 | p = 0.04 |
| FSDS-R | 7.23 ± 3.72 | 9.35 ± 4.51 | p = 0.03 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Zachariou, A.; Zikopoulos, A.; Sapouna, V.; Skentou, C.; Kaltsas, A.; Giannakis, I.; Zachariou, D.; Dimitriadis, F.; Mamoulakis, C.; Mai, D.B.T.; et al. Supervised Pelvic Floor Muscle Training Improves Sexual Function and Diminishes Sexual Distress in Women with Relapsing–Remitting Multiple Sclerosis: A Randomised Controlled Study. J. Pers. Med. 2024, 14, 88. https://doi.org/10.3390/jpm14010088
Zachariou A, Zikopoulos A, Sapouna V, Skentou C, Kaltsas A, Giannakis I, Zachariou D, Dimitriadis F, Mamoulakis C, Mai DBT, et al. Supervised Pelvic Floor Muscle Training Improves Sexual Function and Diminishes Sexual Distress in Women with Relapsing–Remitting Multiple Sclerosis: A Randomised Controlled Study. Journal of Personalized Medicine. 2024; 14(1):88. https://doi.org/10.3390/jpm14010088
Chicago/Turabian StyleZachariou, Athanasios, Athanasios Zikopoulos, Vaia Sapouna, Chara Skentou, Aris Kaltsas, Ioannis Giannakis, Dimitrios Zachariou, Fotios Dimitriadis, Charalampos Mamoulakis, Dung Ba Tien Mai, and et al. 2024. "Supervised Pelvic Floor Muscle Training Improves Sexual Function and Diminishes Sexual Distress in Women with Relapsing–Remitting Multiple Sclerosis: A Randomised Controlled Study" Journal of Personalized Medicine 14, no. 1: 88. https://doi.org/10.3390/jpm14010088
APA StyleZachariou, A., Zikopoulos, A., Sapouna, V., Skentou, C., Kaltsas, A., Giannakis, I., Zachariou, D., Dimitriadis, F., Mamoulakis, C., Mai, D. B. T., Phuoc, N. H. V., Takenaka, A., & Sofikitis, N. (2024). Supervised Pelvic Floor Muscle Training Improves Sexual Function and Diminishes Sexual Distress in Women with Relapsing–Remitting Multiple Sclerosis: A Randomised Controlled Study. Journal of Personalized Medicine, 14(1), 88. https://doi.org/10.3390/jpm14010088