The Efficacy of an Ultrasound-Guided Improved Puncture Path Technique of Nerve Block/Pulsed Radiofrequency for Pudendal Neuralgia: A Retrospective Study
Abstract
:1. Introduction
2. Patients and Methods
2.1. Data Sources
2.2. Data Collocation
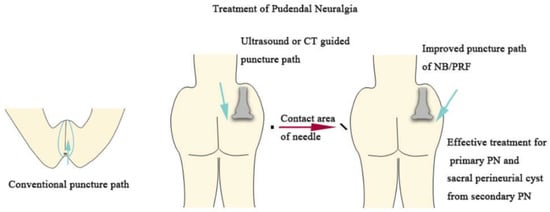
2.3. Conventional Pudendal NB and Ultrasound-Guided Improved Pudendal NB
2.3.1. Conventional Pudendal NB Technique
2.3.2. Ultrasound-Guided Improved Pudendal NB Puncture Path Technique
2.3.3. Ultrasound-Guided Improved Pudendal NB and PRF Puncture Path Technique Group
2.4. Statistical Analysis
3. Results
3.1. Subject Characteristics
3.2. Comparison between Conventional and Improved Pudendal NB
3.3. Comparison between NB and PRF
3.4. Comparison between Secondary and Primary Pudendal Neuralgia Treated with PRF
3.5. Efficacy for Various Etiologies of Secondary Pudendal Neuralgia with PRF
3.6. Degree of Pain Relief (>50%) in Pudendal Neuralgia
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Chiarioni, G.; Asteria, C.; Whitehead, W.E. Chronic proctalgia and chronic pelvic pain syndromes: New etiologic insights and treatment options. World J. Gastroenterol. 2011, 17, 4447–4455. [Google Scholar] [CrossRef] [PubMed]
- Cvetanovich, G.L.; Saltzman, B.M.; Ukwuani, G.; Frank, R.M.; Verma, N.N.; Bush-Joseph, C.A.; Nho, S.J. Anatomy of the Pudendal Nerve and Other Neural Structures Around the Proximal Hamstring Origin in Males. Arthroscopy 2018, 34, 2105–2110. [Google Scholar] [CrossRef] [PubMed]
- Bornstein, J.; Goldstein, A.T.; Stockdale, C.K.; Bergeron, S.; Pukall, C.; Zolnoun, D.; Coady, D. 2015 ISSVD, ISSWSH and IPPS Consensus Terminology and Classification of Persistent Vulvar Pain and Vulvodynia. Obstet. Gynecol. 2016, 127, 745–751. [Google Scholar] [CrossRef] [PubMed]
- Dellon, A.L.; Coady, D. Vulvar and pelvic pain terminology review: Implications for microsurgeons. Microsurgery 2015, 35, 85–90. [Google Scholar] [CrossRef]
- Hibner, M.; Desai, N.; Robertson, L.J.; Nour, M. Pudendal neuralgia. J. Minim. Invasive Gynecol. 2010, 17, 148–153. [Google Scholar] [CrossRef]
- Jones, S.; Chhabra, A.; Vadim, P.-K. Pulsed radiofrequency ablation of pudendal nerve for treatment of a case of refractory pelvic pain. Pain Physician 2017, 20, E451–E454. [Google Scholar] [CrossRef]
- Frank, C.E.; Flaxman, T.; Goddard, Y. The Use of Pulsed Radiofrequency for the Treatment of Pudendal Neuralgia: A Case Series. J. Obstet. Gynaecol. Can. 2019, 41, 1558–1663. [Google Scholar] [CrossRef]
- Bellingham, G.A.; Bhatia, A.; Chan, C.W.; Peng, P.W. Randomized controlled trial comparing pudendal nerve block under ultrasound and fluoroscopic guidance. Reg. Anesth. Pain Med. 2012, 37, 262–266. [Google Scholar] [CrossRef]
- Rhame, E.E.; Levey, K.A.; Gharibo, C.G. Successful Treatment of Refractory Pudendal Neuralgia with Pulsed Radiofrequency. Pain Physician 2009, 12, 633–638. [Google Scholar] [CrossRef]
- Fang, H.; Zhang, J.; Yang, Y.; Ye, L.; Wang, X. Clinical effect and safety of pulsed radiofrequency treatment for pudendal neuralgia: A prospective, randomized controlled clinical trial. J. Pain Res. 2018, 11, 2367–2374. [Google Scholar] [CrossRef] [Green Version]
- Chang, M.C. Efficacy of Pulsed Radiofrequency Stimulation in Patients with Peripheral Neuropathic Pain: A Narrative Review. Pain Physician 2018, 21, E225–E234. [Google Scholar] [CrossRef] [PubMed]
- Vallejo, R.; Benyamin, R.M.; Kramer, J.; Stanton, G.; Joseph, N.J. Pulsed Radiofrequency Denervation for the Treatment of Sacroiliac Joint Syndrome. Pain Med. 2006, 7, 429–434. [Google Scholar] [CrossRef] [PubMed]
- Khoder, W.; Hale, D. Pudendal neuralgia. Obstet. Gynecol. Clin. N. Am. 2014, 41, 443–452. [Google Scholar] [CrossRef] [PubMed]
- Labat, J.-J.; Riant, T.; Robert, R.; Amarenco, G.; Lefaucheur, J.-P.; Rigaud, J. Diagnostic criteria for pudendal neuralgia by pudendal nerve entrapment (Nantes criteria). Neurourol. Urodyn. 2008, 27, 306–310. [Google Scholar] [CrossRef] [PubMed]
- Abdi, S.; Shenouda, P.; Patel, N.; Saini, B.; Bharat, Y.; Calvillo, O. A Novel Technique for Pudendal Nerve Block. Pain Physician 2004, 7, 3. [Google Scholar]
- Wiffen, P.J.; Derry, S.; Bell, R.F.; Rice, A.S.; Tolle, T.R.; Phillips, T.; Moore, R.A. Gabapentin for chronic neuropathic pain in adults. Cochrane Database Syst. Rev. 2017, 6, CD007938. [Google Scholar] [CrossRef] [Green Version]
- Derry, S.; Wiffen, P.J.; Kalso, E.A.; Bell, R.F.; Aldington, D.; Phillips, T.; Gaskell, H.; Moore, R.A. Topical analgesics for acute and chronic pain in adults—An overview of Cochrane Reviews. Cochrane Database Syst. Rev. 2017, 5, CD008609. [Google Scholar] [CrossRef]
- Konschake, M.; Brenner, E.; Moriggl, B.; Hörmann, R.; Bauer, S.; Foditsch, E.; Janetschek, G.; Künzel, K.-H.; Sievert, K.-D.; Zimmermann, R. New laparoscopic approach to the pudendal nerve for neuromodulation based on an anatomic study. Neurourol. Urodyn. 2017, 36, 1069–1075. [Google Scholar] [CrossRef]
- Tricard, T.; Munier, P.; Story, F.; Lang, H.; Saussine, C. The drug-resistant pudendal neuralgia management: A systematic review. Neurourol. Urodyn. 2019, 38, 13–21. [Google Scholar] [CrossRef]
- Hong, M.-J.; Kim, Y.-D.; Park, J.-K.; Hong, H.-J. Management of pudendal neuralgia using ultrasound-guided pulsed radiofrequency: A report of two cases and discussion of pudendal nerve block techniques. J. Anesth. 2016, 30, 356–359. [Google Scholar] [CrossRef]
- Matejčík, V. Surgical location and anatomical variations of pudendal nerve. ANZ J. Surg. 2012, 82, 935–938. [Google Scholar] [CrossRef] [PubMed]
- Pombo, M.; Bradley, J.B. Proximal Hamstring Avulsion Injuries: A Technique Note on Surgical Repairs. Sports Health 2009, 1, 261–264. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Woodley, S.J.; Mercer, S.R. Hamstring muscles: Architecture and innervation. Cells Tissues Organs 2005, 179, 125–141. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Miller, S.L.; Gill, J.; Webb, G.R. The proximal origin of the hamstrings and surrounding anatomy encountered during repair: A cadaveric study. J. Bone Joint Surg. Am. 2007, 89, 44–48. [Google Scholar] [CrossRef] [PubMed]
- Fredrickson, M.J.; Wolstencroft, P.J.; Chinchanwala, S.; Boland, M.R. Does motor block related to long-acting brachial plexus block cause patient dissatisfaction after minor wrist and hand surgery? A randomized observer-blinded trial. Br. J. Anaesth. 2012, 109, 809–815. [Google Scholar] [CrossRef] [Green Version]
- Cheng, L.; Banker, A.S.; Martin, M.; Kozak, I.; Freeman, W.R. Triamcinolone acetonide concentration of aqueous humor after decanted 20-mg intravitreal injection. Ophthalmology 2009, 116, 1356–1359. [Google Scholar] [CrossRef]
- Chua, N.H.L.; Vissers, K.C.; Sluijter, M.E. Pulsed radiofrequency treatment in interventional pain management: Mechanisms and potential indications-a review. Acta Neurochir. 2011, 153, 763–771. [Google Scholar] [CrossRef] [Green Version]
- Elsawaf, A.; Awad, T.E.; Fesal, S.S. Surgical excision of symptomatic sacral perineurial Tarlov cyst: Case series and review of the literature. Eur. Spine J. 2016, 25, 3385–3392. [Google Scholar] [CrossRef]
- Tarlov, I.M. Spinal perineurial and meningeal cysts. J. Neurol. Neurosurg. Psychiatry 1970, 33, 10. [Google Scholar] [CrossRef] [Green Version]



| NB (n = 40) | PRF (n = 48) | p Value | ||
|---|---|---|---|---|
| Gender (%) | Female | 30 (75%) | 32 (66.7%) | 0.546 |
| male | 10 (25%) | 16 (33.3%) | - | |
| Age (Mean ± SD) | 51.9 ± 13.0 | 59.4 ± 14.1 | 0.073 | |
| Side (%) | Unilateral | 16 (40%) | 14 (29.2%) | 0.450 |
| bilateral | 24 (60%) | 34 (70.8%) | - | |
| Etiology (%) | secondary | 18 (45%) | 28 (58.3%) | 0.316 |
| primary | 22 (55%) | 20 (41.7%) | - | |
| Conventional Pudendal NB (n = 22) | Improved Pudendal NB (n = 18) | p Value (Conventional vs. Improved) | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| VAS | Pain Severity | p Value (BS vs. Point-In-Time) | VAS | Pain Severity | p Value (BS vs. Point-In-Time) | ||||||
| Mean | SD | Mean (%) | SD | Mean | SD | Mean(%) | SD | ||||
| baseline | 6.6 | 0.7 | 100% | 0.11 | - | 6.6 | 0.83 | 100% | 0.12 | - | 1.0 |
| 1d | 1.7 | 0.5 | 25.9% | 0.07 | p < 0.001 | 1.6 | 0.21 | 24.0% | 0.05 | p < 0.001 | 0.739 |
| 3d | 1.9 | 0.6 | 29.6% | 0.08 | p < 0.001 | 1.7 | 0.35 | 29.0% | 0.07 | p < 0.001 | 0.977 |
| 7d | 6.0 | 1.0 | 90.9% | 0.13 | 0.091 | 5.8 | 1.25 | 87.8% | 0.11 | p < 0.05 | 0.573 |
| 14d | 6.1 | 1.1 | 91.8% | 0.12 | 0.105 | 6.1 | 1.27 | 91.1% | 0.12 | 0.140 | 0.894 |
| 1M | 6.2 | 1.1 | 92.7% | 0.10 | 0.120 | 6.1 | 1.18 | 92.2% | 0.10 | 0.162 | 0.911 |
| 3M | 6.4 | 0.9 | 95.5% | 0.07 | 0.255 | 6.2 | 1.03 | 94.4% | 0.07 | 0.269 | 0.754 |
| NB (n = 40) | PRF (n = 48) | p Value (NB vs. PRF) | |||||||
|---|---|---|---|---|---|---|---|---|---|
| VAS | Pain Severity | VAS | Pain Severity | ||||||
| Mean | SD | Mean (%) | SD | Mean | SD | Mean (%) | SD | ||
| baseline | 6.61 | 0.75 | 100% | 0.11 | 6.8 | 0.68 | 100% | 0.10 | 1.0 |
| 1d | 1.63 | 0.42 | 25% | 0.06 | 1.8 | 0.32 | 26% | 0.05 | 0.739 |
| 3d | 1.84 | 0.51 | 29.5% | 0.07 | 2.01 | 0.90 | 29.6% | 0.14 | 0.981 |
| 7d | 5.95 | 1.21 | 89.5% | 0.12 | 1.97 | 0.87 | 31.0% | 0.14 | p < 0.001 |
| 14d | 6.08 | 1.17 | 91.5% | 0.11 | 2.23 | 0.91 | 32.3% | 0.13 | p < 0.001 |
| 1M | 6.18 | 1.09 | 92.5% | 0.10 | 2.71 | 1.48 | 40.8% | 0.22 | p < 0.001 |
| 3M | 6.31 | 0.92 | 95.0% | 0.07 | 4.01 | 2.30 | 59.8% | 0.35 | p < 0.001 |
| Improved Pudendal PRF | |||||||||
|---|---|---|---|---|---|---|---|---|---|
| Secondary Pudendal Neuralgia (n = 28) | Primary Pudendal Neuralgia (n = 20) | p Value (Secondary vs. Primary) | |||||||
| VAS | Pain Severity | VAS | Pain Severity | ||||||
| Mean | SD | Mean (%) | SD | Mean | SD | Mean (%) | SD | ||
| baseline | 6.64 | 0.68 | 100% | 0.10 | 7.1 | 0.63 | 100% | 0.93 | 0.153 |
| 1d | 2.8 | 0.9 | 27% | 0.04 | 1.71 | 0.46 | 23% | 0.05 | 0.059 |
| 3d | 2.19 | 1.05 | 31.8% | 0.16 | 1.76 | 0.61 | 26.5% | 0.10 | 0.367 |
| 7d | 1.93 | 1.1 | 32.5% | 0.17 | 2.03 | 0.43 | 29.0% | 0.08 | 0.546 |
| 14d | 2.4 | 1.1 | 35.0% | 0.15 | 1.98 | 0.45 | 28.5% | 0.09 | 0.236 |
| 1M | 3.25 | 1.7 | 49.6% | 0.25 | 1.96 | 0.47 | 28.5% | 0.07 | p < 0.05 |
| 3M | 4.99 | 2.2 | 75.4% | 0.33 | 2.65 | 1.70 | 38.0% | 0.27 | p < 0.01 |
| Secondary Pudendal Neuralgia of PRF (n = 28) | ||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Surgery (n = 6) | Trauma (n = 12, Occured After Urinary Tract Infection, after Sexual Life) | Sacral Perineurial Cyst (n = 6) | Diabetes (n = 4) | |||||||||||||
| VAS | Pain Severity | VAS | Pain Severity | VAS | Pain Severity | VAS | Pain Severity | |||||||||
| mean | SD | Mean (%) | SD | mean | SD | Mean (%) | SD | mean | SD | Mean (%) | SD | mean | SD | Mean (%) | SD | |
| baseline | 6.53 | 0.58 | 96% | 0.08 | 6.4 | 0.84 | 94.1% | 0.12 | 6.73 | 0.40 | 99% | 0.06 | 7.35 | 0.21 | 108% | 0.03 |
| 1d | 2.4 | 0.17 | 30.0% | 0 | 2.95 | 1.11 | 28.3% | 0.04 | 2.5 | 1.06 | 26.7% | 0.15 | 3.4 | 0.85 | 25.0% | 0.07 |
| 3d | 1.67 | 0.23 | 26.7% | 0.06 | 2.32 | 1.31 | 35.8% | 0.20 | 1.87 | 0.64 | 23.3% | 0.15 | 3.1 | 1.27 | 40.0% | 0.14 |
| 7d | 2.63 | 1.44 | 41.7% | 0.25 | 2 | 1.02 | 32.5% | 0.17 | 0.9 | 0.35 | 21.7% | 0.13 | 2.2 | 1.13 | 35.0% | 0.07 |
| 14d | 3.3 | 0.92 | 50.0% | 0.15 | 2.65 | 1.01 | 37.5% | 0.13 | 1 | 0.52 | 18.3% | 0.07 | 2.5 | 0.42 | 30.0% | 0.05 |
| 1M | 3.47 | 1.96 | 56.7% | 0.3 | 3.51 | 1.70 | 55.0% | 0.23 | 1.47 | 0.80 | 21.7% * | 0.13 | 4.75 | 0..64 | 65.0% | 0.07 |
| 3M | 5.4 | 2.31 | 81.7% | 0.32 | 5.4 | 1.55 | 77.9% | 0.23 | 2.87 | 3.17 | 43.3% | 0.49 | 6.25 | 1.77 | 85.0% | 0.21 |
| Degree of Pain Relief > 50% (n, %) | ||||||||
|---|---|---|---|---|---|---|---|---|
| Conventional Pudendal NB (n = 22) | Improved Pudendal NB (n = 18) | Improved Pudendal PRF(n = 48) | ||||||
| Primary Pudendal Neuralgia (n = 20) | Secondary Pudendal Neuralgia (n = 28) | |||||||
| Surgery (n = 6) | Trauma (n = 12) | Sacral perineurial cyst (n = 6) | Diabetes (n = 4) | Total (n = 28) | ||||
| baseline | 0 (0%) | 0 (0%) | 0 (0%) | 0 (0%) | 0 (0%) | 0 (0%) | 0 (0%) | 0 (0%) |
| 1d | 22 (100%) | 18 (100%) | 20 (100%) | 6 (100%) | 12 (100%) | 6 (100%) | 4 (100%) | 28 (100%) |
| 3d | 22 (100%) | 18 (100%) | 20 (100%) | 6 (100%) | 11 (91.7%) | 6 (100%) | 4 (100%) | 26 (92.8%) |
| 7d | 0 (0%) | 0 (0%) | 20 (100%) | 4 (67%) | 11 (91.7%) | 6 (100%) | 4 (100%) | 24 (85.7%) |
| 14d | 0 (0%) | 0 (0%) | 20 (100%) | 4 (67%) | 10 (83.3% | 6 (100%) | 4 (100%) | 24 (85.7%) |
| 1M | 0 (0%) | 0 (0%) | 20 (100%) | 0 (0%) | 6 (50%) | 6 (100%) | 0 (0%) | 14 (50%) |
| 3M | 0 (0%) | 0 (0%) | 17 (85%) | 1 (16.7%) | 2 (16.7%) | 6 (100%) | 0 (0%) | 8 (28.6%) |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Zhu, D.; Fan, Z.; Cheng, F.; Li, Y.; Huo, X.; Cui, J. The Efficacy of an Ultrasound-Guided Improved Puncture Path Technique of Nerve Block/Pulsed Radiofrequency for Pudendal Neuralgia: A Retrospective Study. Brain Sci. 2022, 12, 510. https://doi.org/10.3390/brainsci12040510
Zhu D, Fan Z, Cheng F, Li Y, Huo X, Cui J. The Efficacy of an Ultrasound-Guided Improved Puncture Path Technique of Nerve Block/Pulsed Radiofrequency for Pudendal Neuralgia: A Retrospective Study. Brain Sciences. 2022; 12(4):510. https://doi.org/10.3390/brainsci12040510
Chicago/Turabian StyleZhu, Dan, Zhenzhen Fan, Fujun Cheng, Yuping Li, Xingyue Huo, and Jian Cui. 2022. "The Efficacy of an Ultrasound-Guided Improved Puncture Path Technique of Nerve Block/Pulsed Radiofrequency for Pudendal Neuralgia: A Retrospective Study" Brain Sciences 12, no. 4: 510. https://doi.org/10.3390/brainsci12040510
APA StyleZhu, D., Fan, Z., Cheng, F., Li, Y., Huo, X., & Cui, J. (2022). The Efficacy of an Ultrasound-Guided Improved Puncture Path Technique of Nerve Block/Pulsed Radiofrequency for Pudendal Neuralgia: A Retrospective Study. Brain Sciences, 12(4), 510. https://doi.org/10.3390/brainsci12040510