Oxidative Stress and Inflammatory Biomarkers Are Related to High Intake of Ultra-Processed Food in Old Adults with Metabolic Syndrome
Abstract
:1. Introduction
2. Methods
2.1. Study Design and Participants
2.2. Anthropometrics, Dietary Intake, and Physical Activity
2.3. Blood Collection and Analysis
2.4. Collection of Urine Samples
2.5. Enzymatic Determinations
2.6. Malondialdehyde Assay
2.7. Polyphenol Determination
2.8. Immunoassay Kits
2.9. Determination of 8-Oxo-7,8-dihydro-guanosine and 8-Oxo-7,8-dihydroguanosine
2.10. Neutrophils Reactive Oxygen Species Production
2.11. Statistical Analysis
3. Results
4. Discussion
Strengths and Limitations of the Study
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Suksatan, W.; Moradi, S.; Naeini, F.; Bagheri, R.; Mohammadi, H.; Talebi, S.; Mehrabani, S.; Ali Hojjati Kermani, M.; Suzuki, K. Ultra-processed food consumption and adult mortality risk: A systematic review and dose–response meta-analysis of 207,291 participants. Nutrients 2021, 14, 174. [Google Scholar] [CrossRef] [PubMed]
- Kearney, J. Food consumption trends and drivers. Philos. Trans. R. Soc. B Biol. Sci. 2010, 365, 2793–2807. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Beslay, M.; Srour, B.; Méjean, C.; Allès, B.; Fiolet, T.; Debras, C.; Chazelas, E.; Deschasaux, M.; Wendeu-Foyet, M.G.; Hercberg, S.; et al. Ultra-processed food intake in association with BMI change and risk of overweight and obesity: A prospective analysis of the French NutriNet-Santé cohort. PLoS Med. 2020, 17, e1003256. [Google Scholar] [CrossRef] [PubMed]
- Monteiro, C.A.; Cannon, G.; Levy, R.B.; Moubarac, J.C.; Louzada, M.L.C.; Rauber, F.; Khandpur, N.; Cediel, G.; Neri, D.; Martinez-Steele, E.; et al. Ultra-processed foods: What they are and how to identify them. Public Health Nutr. 2019, 22, 936–941. [Google Scholar] [CrossRef]
- Monteiro, C.A.; Cannon, G.; Lawrence, M.; Costa Louzada, M.L.; Pereira Machado, P. Ultra-Processed Foods, Diet Quality, and Health Using the NOVA Classification System; The Food and Agriculture Organization: Rome, Italy, 2019; pp. 1–44. [Google Scholar]
- Mertens, E.; Colizzi, C.; Peñalvo, J.L. Ultra-processed food consumption in adults across Europe. Eur. J. Nutr. 2022, 61, 1521–1539. [Google Scholar] [CrossRef]
- DeSalvo, K.B.; Olson, R.; Casavale, K.O. Dietary Guidelines for Americans. JAMA 2016, 315, 457–458. [Google Scholar] [CrossRef] [Green Version]
- Fardet, A. Minimally processed foods are more satiating and less hyperglycemic than ultra-processed foods: A preliminary study with 98 ready-to-eat foods. Food Funct. 2016, 7, 2338–2346. [Google Scholar] [CrossRef]
- Poti, J.M.; Braga, B.; Qin, B. Ultra-processed Food Intake and Obesity: What Really Matters for Health-Processing or Nutrient Content? Curr. Obes. Rep. 2017, 6, 420–431. [Google Scholar] [CrossRef]
- Elizabeth, L.; Machado, P.; Zinöcker, M.; Baker, P.; Lawrence, M. Ultra-Processed Foods and Health Outcomes: A Narrative Review. Nutrients 2020, 12, 1955. [Google Scholar] [CrossRef]
- Levy, R.B.; Rauber, F.; Chang, K.; Louzada, M.L.d.C.; Monteiro, C.A.; Millett, C.; Vamos, E.P. Ultra-processed food consumption and type 2 diabetes incidence: A prospective cohort study. Clin. Nutr. 2021, 40, 3608–3614. [Google Scholar] [CrossRef]
- Donat-Vargas, C.; Sandoval-Insausti, H.; Rey-Garciá, J.; Moreno-Franco, B.; Åkesson, A.; Banegas, J.R.; Rodríguez-Artalejo, F.; Guallar-Castillon, P. High Consumption of Ultra-Processed Food is Associated with Incident Dyslipidemia: A Prospective Study of Older Adults. J. Nutr. 2021, 151, 2390–2398. [Google Scholar] [CrossRef] [PubMed]
- Konieczna, J.; Fiol, M.; Colom, A.; Martínez-González, M.Á.; Salas-Salvadó, J.; Corella, D.; Soria-Florido, M.T.; Martínez, J.A.; Alonso-Gómez, Á.M.; Wärnberg, J.; et al. Does Consumption of Ultra-Processed Foods Matter for Liver Health? Prospective Analysis among Older Adults with Metabolic Syndrome. Nutrients 2022, 14, 4142. [Google Scholar] [CrossRef] [PubMed]
- Martínez Leo, E.E.; Peñafiel, A.M.; Hernández Escalante, V.M.; Cabrera Araujo, Z.M. Ultra-processed diet, systemic oxidative stress, and breach of immunologic tolerance. Nutrition 2021, 91, 111419. [Google Scholar] [CrossRef] [PubMed]
- Song, Z.; Song, R.; Liu, Y.; Wu, Z.; Zhang, X. Effects of ultra-processed foods on the microbiota-gut-brain axis: The bread-and-butter issue. Food Res. Int. 2023, 167, 112730. [Google Scholar] [CrossRef] [PubMed]
- Alberti, K.G.M.M.; Eckel, R.H.; Grundy, S.M.; Zimmet, P.Z.; Cleeman, J.I.; Donato, K.A.; Fruchart, J.-C.; James, W.P.T.; Loria, C.M.; Smith, S.C., Jr.; et al. Harmonizing the metabolic syndrome: A joint interim statement of the International Diabetes Federation Task Force on Epidemiology and Prevention; National Heart, Lung, and Blood Institute; American Heart Association; World Heart Federation; International. Circulation 2009, 120, 1640–1645. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Fernández-Ballart, J.D.; Piñol, J.L.; Zazpe, I.; Corella, D.; Carrasco, P.; Toledo, E.; Perez-Bauer, M.; Martínez-González, M.Á.; Salas-Salvadó, J.; Martn-Moreno, J.M. Relative validity of a semi-quantitative food-frequency questionnaire in an elderly Mediterranean population of Spain. Br. J. Nutr. 2010, 103, 1808–1816. [Google Scholar] [CrossRef] [Green Version]
- Ares, G.; Vidal, L.; Allegue, G.; Giménez, A.; Bandeira, E.; Moratorio, X.; Molina, V.; Curutchet, M.R. Consumers’ conceptualization of ultra-processed foods. Appetite 2016, 105, 611–617. [Google Scholar] [CrossRef]
- Bouzas, C.; Bibiloni, M.d.M.; Julibert, A.; Ruiz-Canela, M.; Salas-Salvadó, J.; Corella, D.; Zomeño, M.D.; Romaguera, D.; Vioque, J.; Alonso-Gómez, Á.M.; et al. Adherence to the Mediterranean Lifestyle and Desired Body Weight Loss in a Mediterranean Adult Population with Overweight: A PREDIMED-Plus Study. Nutrients 2020, 12, 2114. [Google Scholar] [CrossRef]
- Moreiras, O.; Cabrera, L.C.C. Tablas de Composición de Alimentos (Spanish Food Composition Tables), 17th ed.; Pirámide: Madrid, Spain, 2015. [Google Scholar]
- Mataix-Verdú, J.; García-Diz, L.; Mañas-Almendros, M.; Martinez de Victoria, E.; Llopis González, J. Tablas de Composición de Alimentos, 5th ed.; University of Granada: Granada, Spain, 2013. [Google Scholar]
- Quetglas-Llabrés, M.M.; Monserrat-Mesquida, M.; Bouzas, C.; Gómez, C.; Mateos, D.; Ripoll-Vera, T.; Tur, J.A.; Sureda, A. Inflammatory and Oxidative Stress Markers Related to Adherence to the Mediterranean Diet in Patients with Metabolic Syndrome. Antioxidants 2022, 11, 901. [Google Scholar] [CrossRef]
- Ainsworth, B.E.; Haskell, W.L.; Leon, A.S.; Jacobs, D.R., Jr.; Montoye, H.J.; Sallis, J.F.; Paffenbarger, R.S., Jr. Compendium of physical activities: Classification of energy costs of human physical activities. Med. Sci. Sports Exerc. 1993, 25, 71–74. [Google Scholar] [CrossRef]
- Aebi, H. Catalase in Vitro. In Methods in Enzymology; Academic Press: Cambridge, CA, USA, 1984; Volume 105, pp. 121–126. [Google Scholar]
- McCord, J.M.; Fridovich, I. Superoxide dismutase. An enzymic function for erythrocuprein (hemocuprein). J. Biol. Chem. 1969, 244, 6049–6055. [Google Scholar] [CrossRef]
- Capeillère-Blandin, C. Oxidation of guaiacol by myeloperoxidase: A two-electron-oxidized guaiacol transient species as a mediator of NADPH oxidation. Biochem. J. 1998, 336, 395–404. [Google Scholar] [CrossRef] [Green Version]
- Kubiliene, L.; Laugaliene, V.; Pavilonis, A.; Maruska, A.; Majiene, D.; Barcauskaite, K.; Kubilius, R.; Kasparaviciene, G.; Savickas, A. Alternative preparation of propolis extracts: Comparison of their composition and biological activities. BMC Complement. Altern. Med. 2015, 15, 156. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Poulsen, H.E.; Weimann, A.; Henriksen, T.; Kjær, L.K.; Larsen, E.L.; Carlsson, E.R.; Christensen, C.K.; Brandslund, I.; Fenger, M. Oxidatively generated modifications to nucleic acids in vivo: Measurement in urine and plasma. Free Radic. Biol. Med. 2019, 145, 336–341. [Google Scholar] [CrossRef] [PubMed]
- Barbosa, L.B.; Vasconcelos, N.B.R.; Dos Santos, E.A.; Dos Santos, T.R.; Ataide-Silva, T.; Ferreira, H.D.S. Ultra-processed food consumption and metabolic syndrome: A cross-sectional study in Quilombola communities of Alagoas, Brazil. Int. J. Equity Health 2023, 22, 14. [Google Scholar] [CrossRef]
- Pan, F.; Wang, Z.; Wang, H.; Zhang, J.; Su, C.; Jia, X.; Du, W.; Jiang, H.; Li, W.; Wang, L.; et al. Association between Ultra-Processed Food Consumption and Metabolic Syndrome among Adults in China-Results from the China Health and Nutrition Survey. Nutrients 2023, 15, 752. [Google Scholar] [CrossRef]
- Díaz, M.C.; Glaves, A. Relación entre consumo de alimentos procesados, ultraprocesados y riesgo de cáncer: Una revisión sistemática. Rev. Chil. Nutr. 2020, 47, 808–821. [Google Scholar] [CrossRef]
- Talens, P.; Cámara, M.; Daschner, Á.; López, E.; Marín, S.; Martínez, J.A.; Morales, F.J. Informe del Comité Científico de la Agencia Española de SeguridadAlimentaria y Nutrición (AESAN) sobre el impacto del consumo dealimentos “ultra-procesados” en la salud de los consumidores. Rev. Com. Científico AESAN 2020, 31, 49–76. [Google Scholar]
- Dinu, M.; Asensi, M.T.; Pagliai, G.; Lotti, S.; Martini, D.; Colombini, B.; Sofi, F. Consumption of Ultra-Processed Foods Is Inversely Associated with Adherence to the Mediterranean Diet: A Cross-Sectional Study. Nutrients 2022, 14, 2073. [Google Scholar] [CrossRef] [PubMed]
- Da Silva, A.; Felício, M.B.; Caldas, A.P.S.; Miranda Hermsdorff, H.H.; Bersch-Ferreira, Â.C.; Torreglosa, C.R.; Shivappa, N.; Hébert, J.R.; Weber, B.; Bressan, J. Pro-inflammatory diet is associated with a high number of cardiovascular events and ultra-processed foods consumption in patients in secondary care. Public Health Nutr. 2021, 24, 3331. [Google Scholar] [CrossRef]
- Juul, F.; Vaidean, G.; Parekh, N. Ultra-processed Foods and Cardiovascular Diseases: Potential Mechanisms of Action. Adv. Nutr. 2021, 12, 1673–1680. [Google Scholar] [CrossRef] [PubMed]
- Contreras-Rodriguez, O.; Solanas, M.; Escorihuela, R.M. Dissecting ultra-processed foods and drinks: Do they have a potential to impact the brain? Rev. Endocr. Metab. Disord. 2022, 23, 697–717. [Google Scholar] [CrossRef] [PubMed]
- Menezes, C.A.; Magalhães, L.B.; da Silva, J.T.; da Silva Lago, R.M.R.; Gomes, A.N.; Ladeia, A.M.T.; Vianna, N.A.; Oliveira, R.R. Ultra-Processed Food Consumption Is Related to Higher Trans Fatty Acids, Sugar Intake, and Micronutrient-Impaired Status in Schoolchildren of Bahia, Brazil. Nutrients 2023, 15, 381. [Google Scholar] [CrossRef]
- Fraga, C.G.; Celep, G.S.; Galleano, M. Biochemical actions of plant phenolics compounds: Thermodynamic and kinetic aspects. Plant Phenolics Hum. Health Biochem. Nutr. Pharmacol. 2009, 3, 91–106. [Google Scholar]
- Mullen, W.; Edwards, C.A.; Crozier, A. Absorption, excretion, and metabolite profiling of methyl-, glucuronyl-, glucosyl- and sulpho-conjugates of quercetin in human plasma and urine after ingestion of onions. Br. J. Nutr. 2006, 96, 107–116. [Google Scholar] [CrossRef] [Green Version]
- Coletro, H.N.; Bressan, J.; Diniz, A.P.; Hermsdorff, H.H.M.; Pimenta, A.M.; Meireles, A.L.; Mendonça, R.d.D.; Carraro, J.C.C. Habitual polyphenol intake of foods according to NOVA classification: Implications of ultra-processed foods intake (CUME study). Int. J. Food Sci. Nutr. 2023, 3, 1–12. [Google Scholar] [CrossRef]
- Wassmann, S.; Wassmann, K.; Nickenig, G. Modulation of Oxidant and Antioxidant Enzyme Expression and Function in Vascular Cells. Hypertension 2004, 44, 381–386. [Google Scholar] [CrossRef]
- Vadillo, E.; Pelayo, R. Toll-like receptors in development and function of the hematopoietic system. Rev. Investig. Clin. 2012, 64, 461–476. [Google Scholar]
- Makni-Maalej, K.; Chiandotto, M.; Hurtado-Nedelec, M.; Bedouhene, S.; Gougerot-Pocidalo, M.A.; Dang, P.M.C.; El-Benna, J. Zymosan induces NADPH oxidase activation in human neutrophils by inducing the phosphorylation of p47phox and the activation of Rac2: Involvement of protein tyrosine kinases, PI3Kinase, PKC, ERK1/2 and p38MAPkinase. Biochem. Pharmacol. 2013, 85, 92–100. [Google Scholar] [CrossRef]
- Anandan, A.; Vrielink, A. Structure and function of lipid A–modifying enzymes. Ann. N. Y. Acad. Sci. 2020, 1459, 19–37. [Google Scholar] [CrossRef]
- Stocker, R.; Keaney, J.F., Jr. Role of oxidative modifications in atherosclerosis. Physiol. Rev. 2004, 84, 1381–1478. [Google Scholar] [CrossRef] [PubMed]
- Millar, S.R.; Navarro, P.; Harrington, J.M.; Shivappa, N.; Hébert, J.R.; Perry, I.J.; Phillips, C.M. Dietary score associations with markers of chronic low-grade inflammation: A cross-sectional comparative analysis of a middle-to older-aged population. Eur. J. Nutr. 2022, 61, 3377–3390. [Google Scholar] [CrossRef]
- Hwang, D.H.; Kim, J.A.; Lee, J.Y. Mechanisms for the activation of Toll-like receptor 2/4 by saturated fatty acids and inhibition by docosahexaenoic acid. Eur. J. Pharmacol. 2016, 785, 24–35. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Anatoliotakis, N.; Deftereos, S.; Bouras, G.; Giannopoulos, G.; Tsounis, D.; Angelidis, C.; Kaoukis, A.; Stefanadis, C. Myeloperoxidase: Expressing inflammation and oxidative stress in cardiovascular disease. Curr. Top. Med. Chem. 2013, 13, 115–138. [Google Scholar] [CrossRef]
- Montero-Salazar, H.; Donat-Vargas, C.; Moreno-Franco, B.; Sandoval-Insausti, H.; Civeira, F.; Laclaustra, M.; Guallar-Castillón, P. High consumption of ultra-processed food may double the risk of subclinical coronary atherosclerosis: The Aragon Workers’ Health Study (AWHS). BMC Med. 2020, 18, 235. [Google Scholar] [CrossRef] [PubMed]
- Silva Dos Santos, F.; Costa Mintem, G.; De Oliveira, I.O.; Horta, B.L.; Ramos, E.; Lopes, C.; Gigante, D.P. Consumption of ultra-processed foods and IL-6 in two cohorts from high- and middle-income countries. Br. J. Nutr. 2023, 129, 1552–1562. [Google Scholar] [CrossRef]
- Lopez-Garcia, E.; Schulze, M.B.; Fung, T.T.; Meigs, J.B.; Rifai, N.; Manson, J.A.E.; Hu, F.B. Major dietary patterns are related to plasma concentrations of markers of inflammation and endothelial dysfunction. Am. J. Clin. Nutr. 2004, 80, 1029–1035. [Google Scholar] [CrossRef] [Green Version]
- Galland, L. Diet and inflammation. Nutr. Clin. Pract. 2010, 25, 634–640. [Google Scholar] [CrossRef]
- Fernandes, A.E.; Rosa, P.W.L.; Melo, M.E.; Martins, R.C.R.; Santin, F.G.O.; Moura, A.M.S.H.; Coelho, G.S.M.A.; Sabino, E.C.; Cercato, C.; Mancini, M.C. Differences in the gut microbiota of women according to ultra-processed food consumption. Nutr. Metab. Cardiovasc. Dis. 2023, 33, 84–89. [Google Scholar] [CrossRef]
- Guo, L.; Liu, M.F.; Huang, J.N.; Li, J.M.; Jiang, J.; Wang, J. Role of interleukin-15 in cardiovascular diseases. J. Cell. Mol. Med. 2020, 24, 7094. [Google Scholar] [CrossRef]
- Martins, G.M.D.S.; França, A.K.T.D.C.; Viola, P.C.D.A.F.; De Carvalho, C.A.; Marques, K.D.S.; Dos Santos, A.M.; Batalha, M.A.; Alves, J.D.D.A.; Ribeiro, C.C.C. Intake of ultra-processed foods is associated with inflammatory markers in Brazilian adolescents. Public Health Nutr. 2022, 25, 591. [Google Scholar] [CrossRef] [PubMed]
- Wuttge, D.M.; Eriksson, P.; Sirsjö, A.; Hansson, G.K.; Stemme, S. Expression of Interleukin-15 in Mouse and Human Atherosclerotic Lesions. Am. J. Pathol. 2001, 159, 417. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Bahrampour, N.; Shiraseb, F.; Noori, S.; Clark, C.C.T.; Mirzaei, K. Is there any putative mediatory role of inflammatory markers on the association between ultra-processed foods and resting metabolic rate? Front. Nutr. 2022, 9, 932225. [Google Scholar] [CrossRef] [PubMed]




| Low UPF Intake (n = 46) | High UPF Intake (n = 46) | p-Value | |
|---|---|---|---|
| Age (years) | 65.1 ± 4.5 | 64.6 ± 4.4 | 0.612 |
| Female [n (%)] | 25 (54.3) | 13 (28.3) | 0.011 |
| Male [n (%)] | 21 (45.7) | 33 (71.7) | |
| Anthropometrical parameters | |||
| Weight (kg) | 84.6 ± 12.0 | 90.6 ± 12.9 | 0.205 |
| Height (cm) | 161 ± 9 | 166 ± 8 | 0.068 |
| BMI (kg/m2) | 32.7 ± 3.3 | 32.8 ± 3.9 | 0.739 |
| WHtR | 0.687 ± 0.056 | 0.678 ± 0.061 | 0.586 |
| Abdominal obesity (cm) | 110.3 ± 9.6 | 112.5 ± 10.0 | 0.808 |
| Systolic blood pressure (mmHg) | 144 ± 19 | 141 ± 18 | 0.210 |
| Diastolic blood pressure (mmHg) | 81.6 ± 11.6 | 82.0 ± 10.4 | 0.884 |
| Clinical parameters | |||
| Glucose (mg/dL) | 115 ± 24 | 121 ± 50 | 0.945 |
| HbA1c (%) | 6.14 ± 0.72 | 6.28 ± 1.50 | 0.951 |
| Triglycerides (mg/dL) | 153 ± 68 | 162 ± 83 | 0.802 |
| HDL-Cholesterol (mg/dL) | 45.5 ± 11.5 | 44.0 ± 11.8 | 0.963 |
| LDL-Cholesterol (mg/dL) | 116 ± 36 | 109 ± 30 | 0.605 |
| Cholesterol total (mg/dL) | 191 ± 40 | 184 ± 33 | 0.712 |
| Uric acid (mg/dL) | 6.12 ± 1.50 | 6.23 ± 1.37 | 0.611 |
| Lifestyle parameters | |||
| Physical activity (METs·min/week) | 3734 ± 3600 | 2960 ± 2623 | 0.055 |
| Mediterranean diet adherence (score) | 8.15 ± 2.4 | 6.80 ± 2.03 | 0.015 |
| Basal metabolism rate (kcal) | 1628 ± 278 | 1772 ± 280 | 0.310 |
| Ingested calories (Kcal/day) | 2385 ± 809 | 2575 ± 658 | 0.857 |
| DII | −0.029 ± 1.73 | 0.721 ± 1.89 | 0.038 |
| Drug intake | |||
| Antidiabetic [n (%)] | 17 (37%) | 14 (30%) | 0.508 |
| Antihypertensive [n (%)] | 38 (83%) | 37 (80%) | 0.788 |
| Lipid-lowering [n (%)] | 24 (52%) | 30 (65%) | 0.204 |
| Low UPF Intake (n = 46) | High UPF Intake (n = 46) | p-Value | |
|---|---|---|---|
| Macronutrients | |||
| Carbohydrates (g/day) | 246.6 ± 98.1 | 265.3 ± 74.9 | 0.768 |
| Proteins (g/day) | 94.0 ± 28.0 | 97.0 ± 24.4 | 0.722 |
| Lipids (g/day) | 101.3 ± 37.0 | 113.8 ± 37.7 | 0.475 |
| Micronutrients | |||
| MUFAs (g/day) | 51.2 ± 20.3 | 56.7 ± 20.1 | 0.609 |
| PUFAs (g/day) | 17.2 ± 7.5 | 19.1 ± 16.8 | 0.567 |
| SFA (g/day) | 25.9 ± 9.9 | 30.9 ± 11.3 | 0.014 |
| Trans FA (g/day) | 0.570 ± 0.307 | 0.759 ± 0.472 | 0.013 |
| w-6 FA (g/day) | 13.4 ± 6.2 | 15.0 ± 7.1 | 0.522 |
| w-3 FA (g/day) | 0.795 ± 0.464 | 0.755 ± 0.369 | 0.524 |
| Cholesterol (mg/day) | 390.0 ± 178.6 | 424.5 ± 120.3 | 0.620 |
| Folic acid (µg/day) | 357.7 ± 119.7 | 328.9 ± 107.9 | 0.154 |
| Fiber (g/day) | 28.5 ± 10.3 | 25.2 ± 8.9 | 0.048 |
| Vitamins | |||
| Vitamin A (µg/day) | 1163 ± 613 | 1331 ± 757 | 0.339 |
| Vitamin C (mg/day) | 217 ± 88 | 213 ± 95 | 0.783 |
| Vitamin D (µg/day) | 5.57 ± 3.74 | 5.13 ± 2.43 | 0.492 |
| Vitamin E (mg/day) | 10.3 ± 3.9 | 11.2 ± 3.5 | 0.529 |
| Minerals | |||
| Phosphor (mg/day) | 1645 ± 463 | 1730 ± 425 | 0.890 |
| Magnesium (mg/day) | 424 ± 130 | 421 ± 122 | 0.437 |
| Iron (mg/day) | 16.9 ± 5.6 | 17.2 ± 4.7 | 0.672 |
| Iodine (mg/day) | 234.1 ± 119.5 | 228.1 ± 148.7 | 0.432 |
| Potassium (mg/day) | 4555 ± 1299 | 4416 ± 1251 | 0.324 |
| Calcium (mg/day) | 941.8 ± 287.6 | 988.7 ± 344.7 | 0.958 |
| Sodium (mg/day) | 2524 ± 1188 | 2662 ± 934 | 0.751 |
| Selenium (mg/day) | 115.0 ± 40.1 | 112 ± 32.8 | 0.306 |
| Zinc (mg/day) | 12.2 ± 3.9 | 12.6 ± 3.3 | 0.778 |
| Glycaemic load | 140.1 ± 64.0 | 151.4 ± 49.1 | 0.806 |
| Glycaemic index | 55.8 ± 5.4 | 56.5 ± 4.6 | 0.772 |
| Alcohol (g/day) | 15.8 ± 20.9 | 15.3 ± 18.0 | 0.167 |
| Low UPF Intake (n = 46) | High UPF Intake (n = 46) | p-Value | |
|---|---|---|---|
| Plasma markers | |||
| CAT activity (k/L) | 56.4 ± 29.0 | 46.5 ± 17.4 | 0.047 |
| SOD activity (pkat/L) | 180.1 ± 88.4 | 136.6 ± 71.4 | 0.018 |
| MPO activity (µkat/mL) | 53.3 ± 28.9 | 67.6 ± 31.2 | 0.016 |
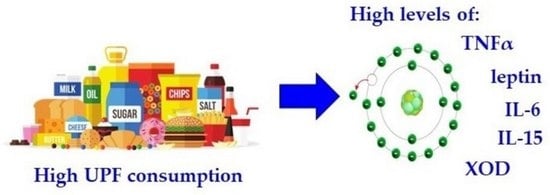
| XO levels (µg/L) | 0.395 ± 0.211 | 0.535 ± 0.449 | 0.030 |
| MDA levels (nM) | 1.06 ± 0.63 | 1.15 ± 0.69 | 0.253 |
| TNFα levels (pg/mL) | 3.17 ± 1.83 | 4.37 ± 1.71 | 0.003 |
| IL-1ß levels (pg/mL) | 19.1 ± 42.2 | 22.5 ± 48.9 | 0.366 |
| IL-6 levels (pg/mL) | 4.23 ± 3.11 | 5.78 ± 3.75 | 0.022 |
| IL-15 levels (pg/mL) | 7.39 ± 3.24 | 10.2 ± 5.82 | 0.048 |
| INF-γ levels (pg/mL) | 5.92 ± 1.75 | 6.22 ± 1.85 | 0.330 |
| MCP-1 levels (pg/mL) | 234.5 ± 89.0 | 232.8 ± 78.9 | 0.462 |
| Resistin levels (ng/mL) | 5.60 ± 6.43 | 6.40 ± 8.39 | 0.385 |
| Ghrelin levels (pg/mL) | 302.1 ± 53.9 | 313.0 ± 57.2 | 0.298 |
| Leptin levels (ng/mL) | 10.3 ± 7.6 | 15.1 ± 16.3 | 0.044 |
| Polyphenol levels (nM) | 0.058 ± 0.020 | 0.057 ± 0.016 | 0.389 |
| Urine markers corrected by creatinine | |||
| MDA levels (mM/mM) | 85.0 ± 53.1 | 108.9 ± 94.4 | 0.133 |
| Polyphenol levels (mM/mM) | 13.0 ± 3.97 | 10.9 ± 3.17 | 0.027 |
| OxoGuo levels (nM/mM) | 1.84 ± 0.39 | 1.91 ± 0.47 | 0.279 |
| OxodG levels (nM/mM) | 1.31 ± 0.43 | 1.43 ± 0.55 | 0.189 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Quetglas-Llabrés, M.M.; Monserrat-Mesquida, M.; Bouzas, C.; Mateos, D.; Ugarriza, L.; Gómez, C.; Tur, J.A.; Sureda, A. Oxidative Stress and Inflammatory Biomarkers Are Related to High Intake of Ultra-Processed Food in Old Adults with Metabolic Syndrome. Antioxidants 2023, 12, 1532. https://doi.org/10.3390/antiox12081532
Quetglas-Llabrés MM, Monserrat-Mesquida M, Bouzas C, Mateos D, Ugarriza L, Gómez C, Tur JA, Sureda A. Oxidative Stress and Inflammatory Biomarkers Are Related to High Intake of Ultra-Processed Food in Old Adults with Metabolic Syndrome. Antioxidants. 2023; 12(8):1532. https://doi.org/10.3390/antiox12081532
Chicago/Turabian StyleQuetglas-Llabrés, Maria Magdalena, Margalida Monserrat-Mesquida, Cristina Bouzas, David Mateos, Lucía Ugarriza, Cristina Gómez, Josep A. Tur, and Antoni Sureda. 2023. "Oxidative Stress and Inflammatory Biomarkers Are Related to High Intake of Ultra-Processed Food in Old Adults with Metabolic Syndrome" Antioxidants 12, no. 8: 1532. https://doi.org/10.3390/antiox12081532
APA StyleQuetglas-Llabrés, M. M., Monserrat-Mesquida, M., Bouzas, C., Mateos, D., Ugarriza, L., Gómez, C., Tur, J. A., & Sureda, A. (2023). Oxidative Stress and Inflammatory Biomarkers Are Related to High Intake of Ultra-Processed Food in Old Adults with Metabolic Syndrome. Antioxidants, 12(8), 1532. https://doi.org/10.3390/antiox12081532