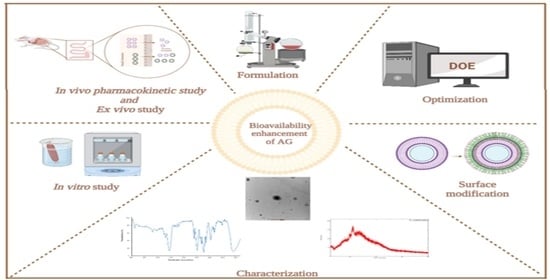
Mannosylated-Chitosan-Coated Andrographolide Nanoliposomes for the Treatment of Hepatitis: In Vitro and In Vivo Evaluations
Abstract
:1. Introduction
2. Materials and Methods
2.1. Materials
2.2. Methods
2.2.1. Preparation of Andrographolide Loaded Nanoliposomes (AGL)
2.2.2. Formulation Optimization Using DoE Software
2.2.3. Preparation of Mannosylated-Chitosan-Coated Nanoliposomes (MCS-AGL)
2.2.4. Particle Size Analysis, PDI and Zeta Potential
2.2.5. Entrapment Efficiency
2.2.6. Solid State Characterization
Fourier Transform Infrared Spectroscopy (FTIR)
Differential Scanning Calorimetry (DSC)
Powder X-Ray Diffraction (PXRD)
Transmission Electron Microscopy
2.2.7. Molecular Docking Studies
2.2.8. In Vitro Drug Release Studies
2.2.9. In Vitro Cell Viability Assay
2.2.10. Ex Vivo Permeation Study
2.2.11. In Vivo Pharmacokinetics Study
3. Results
3.1. Formulation and Optimization of AGL
- (A)
- Particle size (nm) = −48.00208 + 2.49021 * Lipid + 5.18208 * Amplitude + 5.51333 * Sonication time + 0.223000 * Lipid*Amplitude − 0.079875 * Lipid * Sonication time − 1.12725 * Amplitude*Sonication time − 0.067408 * Lipid − 0.192833 * Amplitude + 2.31667 * Sonication time
- (B)
- EE (%) = −566.84200 + 8.21825 * Lipid + 13.31600 * Amplitude + 22.95625 * Sonication time − 0.15560 * Lipid * Amplitude − 0.419750 * Lipid*Sonication time + 0.141000 * Amplitude * Sonication time
3.2. Effect of Independent Variables on Particle Size
3.2.1. Effect of Independent Variables on Entrapment Efficiency
3.2.2. Validation of BBD Model
3.3. Particle Size Analysis, PDI, Zeta Potential and Entrapment Efficiency
3.4. Solid State Characterization
3.4.1. FTIR Studies
3.4.2. DSC Studies
3.4.3. XRD Studies
3.4.4. Transmission Electron Microscopy
3.5. Molecular Docking
3.6. In Vitro Drug Release Studies
3.7. In Vitro Cell Viability
3.8. Ex Vivo Permeation Study
3.9. In Vivo Pharmacokinetics Study
4. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Deb Roy, S.; Das, S.; Shil, D.; Dutta, K. Herbal hepatoprotective agents: A review. World J. Pharm. Res. 2012, 1, 87–99. [Google Scholar]
- Das, S.; Pradhan, G.K.; Das, S.; Nath, D.; Das Saha, K. Enhanced Protective Activity of Nano Formulated Andrographolide against Arsenic Induced Liver Damage. Chem. Biol. Interact. 2015, 242, 281–289. [Google Scholar] [CrossRef] [PubMed]
- Jain, P.K.; Khurana, N.; Pounikar, Y.; Gajbhiye, A.; Kharya, M.D. Enhancement of Absorption and Hepatoprotective Potential through Soya-Phosphatidylcholine-Andrographolide Vesicular System. J. Liposome Res. 2013, 23, 110–118. [Google Scholar] [CrossRef]
- Okhuarobo, A.; Falodun, J.E.; Erharuyi, O.; Imieje, V.; Falodun, A.; Langer, P. Harnessing the Medicinal Properties of Andrographis Paniculata for Diseases and beyond: A Review of Its Phytochemistry and Pharmacology. Asian Pac. J. Trop. Dis. 2014, 4, 213–222. [Google Scholar] [CrossRef]
- Jiang, Y.; Wang, F.; Xu, H.; Liu, H.; Meng, Q.; Liu, W. Development of Andrographolide Loaded PLGA Microspheres: Optimization, Characterization and in Vitro–in Vivo Correlation. Int. J. Pharm. 2014, 475, 475–484. [Google Scholar] [CrossRef]
- Tu, Y.S.; Sun, D.M.; Zhang, J.J.; Jiang, Z.Q.; Chen, Y.X.; Zeng, X.H.; Huang, D.E.; Yao, N. Preparation and Characterisation of Andrographolide Niosomes and Its Anti-Hepatocellular Carcinoma Activity. J. Microencapsul. 2014, 31, 307–316. [Google Scholar] [CrossRef]
- Cao, Y.; Dong, X.; Chen, X. Polymer-Modified Liposomes for Drug Delivery: From Fundamentals to Applications. Pharmaceutics 2022, 14, 778. [Google Scholar] [CrossRef]
- Roy, P.; Das, S.; Auddy, R.G.; Mukherjee, A. Engineered Andrographolide Nanosystems for Smart Recovery in Hepatotoxic Conditions. Int. J. Nanomed. 2014, 9, 4723–4735. [Google Scholar] [CrossRef]
- Maiti, K.; Mukherjee, K.; Murugan, V.; Saha, B.P.; Mukherjee, P.K. Enhancing Bioavailability and Hepatoprotective Activity of Andrographolide from Andrographis Paniculata, a Well-Known Medicinal Food, through Its Herbosome. J. Sci. Food Agric. 2010, 90, 43–51. [Google Scholar] [CrossRef] [PubMed]
- Imam, S.S.; Alshehri, S.; Altamimi, M.A.; Hussain, A.; Qamar, W.; Gilani, S.J.; Zafar, A.; Alruwaili, N.K.; Alanazi, S.; Almutairy, B.K. Formulation of Piperine-Chitosan-Coated Liposomes: Characterization and In Vitro Cytotoxic Evaluation. Molecules 2021, 26, 3281. [Google Scholar] [CrossRef]
- Ejaz, S.; Hogg, B.; Hristov, D.R.; Brayden, D.J.; Imran, M.; Bhattacharjee, S. Add Sugar to Chitosan: Mucoadhesion and In Vitro Intestinal Permeability of Mannosylated Chitosan Nanocarriers. Pharmaceutics 2022, 14, 830. [Google Scholar] [CrossRef]
- Sinha, J.; Mukhopadhyay, S.; Das, N.; Basu, M.K. Targeting of Liposomal Andrographolide to L. Donovani-Infected Macrophages In Vivo. Drug Deliv. 2000, 7, 209–213. [Google Scholar] [CrossRef]
- Narayan, R.; Singh, M.; Ranjan, O.; Nayak, Y.; Garg, S.; Shavi, G.V.; Nayak, U.Y. Development of Risperidone Liposomes for Brain Targeting through Intranasal Route. Life Sci. 2016, 163, 38–45. [Google Scholar] [CrossRef] [PubMed]
- Esfandiari, F.; Motazedian, M.H.; Asgari, Q.; Morowvat, M.H.; Molaei, M.; Heli, H. Erratum to “Paromomycin-Loaded Mannosylated Chitosan Nanoparticles: Synthesis, Characterization and Targeted Drug Delivery against Leishmaniasis”. Acta Trop. 2019, 197, 105073. [Google Scholar] [CrossRef] [PubMed]
- Abdellatif, M.M.; Khalil, I.A.; Khalil, M.A.F. Sertaconazole Nitrate Loaded Nanovesicular Systems for Targeting Skin Fungal Infection: In-Vitro, Ex-Vivo and in-Vivo Evaluation. Int. J. Pharm. 2017, 527, 1–11. [Google Scholar] [CrossRef]
- Elsayad, M.K.; Mowafy, H.A.; Zaky, A.A.; Samy, A.M. Chitosan Caged Liposomes for Improving Oral Bioavailability of Rivaroxaban: In Vitro and In Vivo Evaluation. Pharm. Dev. Technol. 2021, 26, 316–327. [Google Scholar] [CrossRef]
- Chi, C.; Zhang, C.; Liu, Y.; Nie, H.; Zhou, J.; Ding, Y. Phytosome-Nanosuspensions for Silybin-Phospholipid Complex with Increased Bioavailability and Hepatoprotection Efficacy. Eur. J. Pharm. Sci. Off. J. Eur. Fed. Pharm. Sci. 2020, 144, 105212. [Google Scholar] [CrossRef]
- Arif, M.; Ahmad, R.; Sharaf, M.; Samreen; Muhammad, J.; Abdalla, M.; Eltayb, W.A.; Liu, C.-G. Antibacterial and Antibiofilm Activity of Mannose-Modified Chitosan/PMLA Nanoparticles against Multidrug-Resistant Helicobacter Pylori. Int. J. Biol. Macromol. 2022, 223, 418–432. [Google Scholar] [CrossRef] [PubMed]
- Bank, R.P.D. RCSB PDB—1EGG: Structure of a C-Type Carbohydrate-Recognition Domain (CRD-4) from the Macrophage Mannose Receptor. Available online: https://www.rcsb.org/structure/1egg (accessed on 19 January 2023).
- Feinberg, H.; Jégouzo, S.A.F.; Lasanajak, Y.; Smith, D.F.; Drickamer, K.; Weis, W.I.; Taylor, M.E. Structural Analysis of Carbohydrate Binding by the Macrophage Mannose Receptor CD206. J. Biol. Chem. 2021, 296, 100368. [Google Scholar] [CrossRef] [PubMed]
- Li, J.; Abel, R.; Zhu, K.; Cao, Y.; Zhao, S.; Friesner, R.A. The VSGB 2.0 Model: A next Generation Energy Model for High Resolution Protein Structure Modeling. Proteins Struct. Funct. Bioinform. 2011, 79, 2794–2812. [Google Scholar] [CrossRef]
- Friesner, R.A.; Banks, J.L.; Murphy, R.B.; Halgren, T.A.; Klicic, J.J.; Mainz, D.T.; Repasky, M.P.; Knoll, E.H.; Shelley, M.; Perry, J.K.; et al. Glide: A New Approach for Rapid, Accurate Docking and Scoring. 1. Method and Assessment of Docking Accuracy. J. Med. Chem. 2004, 47, 1739–1749. [Google Scholar] [CrossRef] [PubMed]
- Fernandes, G.; Pusuluri, S.L.A.; Nikam, A.N.; Birangal, S.; Shenoy, G.G.; Mutalik, S. Solvent Free Twin Screw Processed Silybin Nanophytophospholipid: In Silico, In Vitro and In Vivo Insights. Pharmaceutics 2022, 14, 2729. [Google Scholar] [CrossRef] [PubMed]
- Bothiraja, C.; Pawar, A.P.; Dama, G.Y.; Joshi, P.P.; Shaikh, K.S. Novel Solvent-Free Gelucire Extract of Plumbago Zeylanica Using Non-Everted Rat Intestinal Sac Method for Improved Therapeutic Efficacy of Plumbagin. J. Pharmacol. Toxicol. Methods 2012, 66, 35–42. [Google Scholar] [CrossRef] [PubMed]
- Agrawal, M.; Saraf, S.; Pradhan, M.; Patel, R.J.; Singhvi, G.; Ajazuddin; Alexander, A. Design and Optimization of Curcumin Loaded Nano Lipid Carrier System Using Box-Behnken Design. Biomed. Pharmacother. 2021, 141, 111919. [Google Scholar] [CrossRef] [PubMed]
- Sabir, F.; Katona, G.; Pallagi, E.; Dobó, D.G.; Akel, H.; Berkesi, D.; Kónya, Z.; Csóka, I. Quality-by-Design-Based Development of n-Propyl-Gallate-Loaded Hyaluronic-Acid-Coated Liposomes for Intranasal Administration. Molecules 2021, 26, 1429. [Google Scholar] [CrossRef]
- AlSawaftah, N.M.; Awad, N.S.; Paul, V.; Kawak, P.S.; Al-Sayah, M.H.; Husseini, G.A. Transferrin-Modified Liposomes Triggered with Ultrasound to Treat HeLa Cells. Sci. Rep. 2021, 11, 11589. [Google Scholar] [CrossRef]
- Sebaaly, C.; Trifan, A.; Sieniawska, E.; Greige-Gerges, H. Chitosan-Coating Effect on the Characteristics of Liposomes: A Focus on Bioactive Compounds and Essential Oils: A Review. Processes 2021, 9, 445. [Google Scholar] [CrossRef]
- Midya, D.K.; Pramanik, K.C.; Chatterjee, T.K. Effect of Andrographolide-Encapsulated Liposomal Formulation on Hepatic Damage and Oxidative Stress. Int. J. Biomed. Pharm. Sci. 2009, 3, 55–59. [Google Scholar]
- Souza, T.G.F.; Ciminelli, V.S.T.; Mohallem, N.D.S. A Comparison of TEM and DLS Methods to Characterize Size Distribution of Ceramic Nanoparticles. J. Phys. Conf. Ser. 2016, 733, 012039. [Google Scholar] [CrossRef]
- Nguyen, T.X.; Huang, L.; Liu, L.; Elamin Abdalla, A.M.; Gauthier, M.; Yang, G. Chitosan-Coated Nano-Liposomes for the Oral Delivery of Berberine Hydrochloride. J. Mater. Chem. B 2014, 2, 7149–7159. [Google Scholar] [CrossRef]











| Factors | Name/Variables | Units | Levels | |
|---|---|---|---|---|
| Low Level (−1) | High Level (+1) | |||
| A | Lipid | mg | 70 | 90 |
| B | Amplitude | % | 30 | 40 |
| C | Sonication time | min | 6 | 10 |
| Run | Factor 1 A: Lipid (mg) | Factor 2 B: Amplitude | Factor 3 C: Sonication Time (min) | Response 1 Particle Size (nm) | Response 2 EE (%) |
|---|---|---|---|---|---|
| 1 | 70 | 35 | 10 | 126 | 76.8 |
| 2 | 90 | 35 | 6 | 112.2 | 95.16 |
| 3 | 90 | 40 | 8 | 106.33 | 68.48 |
| 4 | 70 | 40 | 8 | 104.3 | 96.1 |
| 5 | 80 | 35 | 8 | 112.23 | 78.31 |
| 6 | 80 | 30 | 10 | 120.03 | 50.6 |
| 7 | 90 | 30 | 8 | 80.23 | 66.1 |
| 8 | 80 | 40 | 10 | 103.8 | 75.4 |
| 9 | 80 | 30 | 6 | 112.5 | 75.2 |
| 10 | 80 | 35 | 8 | 122.5 | 75.82 |
| 11 | 80 | 40 | 6 | 141.36 | 94.36 |
| 12 | 90 | 35 | 10 | 97.91 | 54.64 |
| 13 | 70 | 35 | 6 | 133.9 | 83.74 |
| 14 | 70 | 30 | 8 | 122.8 | 68.6 |
| 15 | 80 | 35 | 8 | 110.2 | 67.01 |
| Content | Particle Size | Entrapment Efficiency | ||
|---|---|---|---|---|
| Source | p-value | Status | p-value | Status |
| Model | 0.0038 | Significant | 0.0003 | Significant |
| A-Lipid | 0.0010 | 0.0108 | ||
| B-Amplitude | 0.1853 | 0.0005 | ||
| C-Sonication time | 0.0107 | 0.0002 | ||
| AB | 0.0049 | 0.0146 | ||
| AC | 0.5233 | 0.0101 | ||
| BC | 0.0047 | 0.5892 | ||
| Lack of Fit | 0.9115 | Not significant | 0.7261 | Not significant |
| Independent Variables | Responses | ||||
|---|---|---|---|---|---|
| Lipid (mg) | Amplitude (%) | Time (min) | Particle Size (nm) | Entrapment Efficiency (%) | |
| The composition suggested by the software | 90 | 30 | 6 | 84.65 | 88.61 |
| Practically performed composition | 90 | 30 | 6 | 86.60 | 90.06 |
| Residual error (%) | - | - | - | −2.29 | −1.63 |
| Parameters | AG | AGL | MCS-AGL |
|---|---|---|---|
| t1/2 (h) | 4.06 ± 1.10 | 4.23 ± 1.13 | 16.17 ± 4.36 |
| Tmax (h) | 1.33 ± 0.57 | 1.5 ± 0.86 | 2.00 ± 0.00 |
| Cmax (ng/mL) | 207.14 ± 35.59 | 310.03 ± 12.64 | 495.90 ± 15.78 |
| AUC0–24 (ng/mL*h) | 1410.3 ± 84.40 | 1829.97 ± 141.66 | 2213.46 ± 50.05 |
| AUC0–I (ng/mL*h) | 1869.20 ± 170.47 | 2116.78 ± 317.46 | 4298.36 ± 580.31 |
| MRT (h) | 8.6 ± 0.66 | 5.93 ± 1.53 | 19.43 ± 4.84 |
| Ke (h−1) | 0.13 ± 0.022 | 0.21 ± 0.022 | 0.09 ± 0.09 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Metkar, S.P.; Fernandes, G.; Nikam, A.N.; Soman, S.; Birangal, S.; Seetharam, R.N.; Joshi, M.B.; Mutalik, S. Mannosylated-Chitosan-Coated Andrographolide Nanoliposomes for the Treatment of Hepatitis: In Vitro and In Vivo Evaluations. Membranes 2023, 13, 193. https://doi.org/10.3390/membranes13020193
Metkar SP, Fernandes G, Nikam AN, Soman S, Birangal S, Seetharam RN, Joshi MB, Mutalik S. Mannosylated-Chitosan-Coated Andrographolide Nanoliposomes for the Treatment of Hepatitis: In Vitro and In Vivo Evaluations. Membranes. 2023; 13(2):193. https://doi.org/10.3390/membranes13020193
Chicago/Turabian StyleMetkar, Sayali Pravin, Gasper Fernandes, Ajinkya Nitin Nikam, Soji Soman, Sumit Birangal, Raviraja N Seetharam, Manjunath Bandu Joshi, and Srinivas Mutalik. 2023. "Mannosylated-Chitosan-Coated Andrographolide Nanoliposomes for the Treatment of Hepatitis: In Vitro and In Vivo Evaluations" Membranes 13, no. 2: 193. https://doi.org/10.3390/membranes13020193
APA StyleMetkar, S. P., Fernandes, G., Nikam, A. N., Soman, S., Birangal, S., Seetharam, R. N., Joshi, M. B., & Mutalik, S. (2023). Mannosylated-Chitosan-Coated Andrographolide Nanoliposomes for the Treatment of Hepatitis: In Vitro and In Vivo Evaluations. Membranes, 13(2), 193. https://doi.org/10.3390/membranes13020193