Surgery for Aortic Prosthetic Valve Endocarditis in the Transcatheter Era
Abstract
:1. Introduction
2. Patients and Methods
2.1. Study Design
2.2. Preoperative Risk Determination
2.3. Data Collection, Statistical Analysis, and Illustrations
3. Results
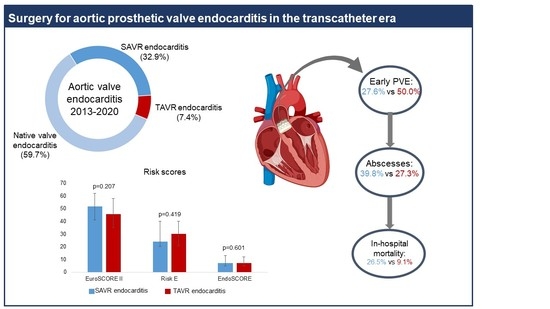
3.1. Patient Population
3.2. Causative Organisms
3.3. Surgical Data
3.4. Morbidities and Outcomes
4. Comment
4.1. Surgical Considerations
4.2. Decision-Making and the Role of an Endocarditis Team
4.3. Limitations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Abbreviations
| BCNIE | Blood culture negative infective endocarditis |
| BMI | Body mass index |
| CABG | Coronary artery bypass grafting |
| CoNS | Coagulase-negative staphylococci |
| COPD | Chronic obstructive pulmonary disease |
| ECLS | Extracorporeal life support |
| EuroSCORE II | European System for Cardiac Operative Risk Evaluation II |
| HACEK | Haemophilus species, Aggregatibacter species, Cardiobacterium hominis, Eikenella corrodens, and Kingella species |
| HIV | Human immunodeficiency virus |
| IABP | Intra-aortic balloon pump |
| ICU | Intensive care unit |
| IE | Infective endocarditis |
| LCOS | Low cardiac output syndrome |
| LVEF | Left ventricle ejection fraction |
| MRSA | Methicillin-resistant Staphylococcus aureus |
| MSSA | Methicillin-susceptible Staphylococcus aureus |
| NVE | Native valve endocarditis |
| NYHA | New York Heart Association |
| PMV | Postoperative mechanical ventilation |
| PVE | Prosthetic valve endocarditis |
| SAVR–PVE | Prosthetic valve endocarditis following surgical aortic valve replacement |
| STS-PROM | Society of thoracic surgeons predicted risk of mortality |
| TAVR | Transcatheter aortic valve replacement |
| TIE | Prosthetic valve endocarditis following transcatheter aortic valve replacement |
References
- Habib, G.; Lancellotti, P.; Antunes, M.J.; Bongiorni, M.G.; Casalta, J.P.; Del Zotti, F.; Dulgheru, R.; El Khoury, G.; Erba, P.A.; Iung, B.; et al. 2015 ESC Guidelines for the management of infective endocarditis. Eur. Heart J. 2015, 36, 3075–3123. [Google Scholar] [CrossRef] [PubMed]
- Nishimura, R.A.; Otto, C.M.; Bonow, R.O.; Carabello, B.A.; Erwin, J.P.; Guyton, R.A.; O’Gara, P.T.; Ruiz, C.E.; Skubas, N.J.; Sorajja, P.; et al. 2014 AHA/ACC guideline for the management of patients with valvular heart disease: A report of the American college of cardiology/American heart association task force on practice guidelines. J. Am. Coll. Cardiol. 2014, 63, e57–e185. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Regueiro, A.; Linke, A.; Latib, A.; Ihlemann, N.; Urena, M.; Walther, T.; Husser, O.; Herrmann, H.C.; Nombela-Franco, L.; Cheema, A.; et al. Infective Endocarditis following Transcatheter Aortic Valve Replacement: Comparison of Balloon-Versus Self-Expandable Valves. Circ. Cardiovasc. Interv. 2019, 12, e007938. [Google Scholar] [CrossRef] [PubMed]
- Summers, M.R.; Leon, M.B.; Smith, C.R.; Kodali, S.K.; Thourani, V.H.; Herrmann, H.C.; Makkar, R.R.; Pibarot, P.; Webb, J.G.; Leipsic, J.; et al. Prosthetic Valve Endocarditis after TAVR and SAVR: Insights from the PARTNER Trials. Circulation 2019, 140, 1984–1994. [Google Scholar] [CrossRef]
- Brouwer, J.; van den Brink, F.S.; Nijenhuis, V.J.; Vossenberg, T.N.; Delewi, R.; van Mourik, M.S.; den Heijer, P.; Tanis, W.; Kievit, P.C.; Holvoet, W.; et al. Incidence and outcome of prosthetic valve endocarditis after transcatheter aortic valve replacement in the Netherlands. Neth. Heart J. 2020, 28, 520–525. [Google Scholar] [CrossRef]
- Saha, S.; Peterss, S.; Mueller, C.; Deseive, S.; Sadoni, S.; Massberg, S.; Hagl, C.; Joskowiak, D. Cardiac surgery following transcatheter aortic valve replacement. Eur. J. Cardio Thorac. Surg. 2021, 60, 1149–1155. [Google Scholar] [CrossRef]
- Malvindi, P.G.; Luthra, S.; Sarvananthan, S.; Zingale, A.; Olevano, C.; Ohri, S. Surgical treatment of transcatheter aortic valve infective endocarditis. Neth. Heart J. 2021, 29, 71–77. [Google Scholar] [CrossRef]
- Varela, L.; López-Menéndez, J.; Redondo, A.; Fajardo, E.R.; Miguelena, J.; Centella, T.; Martín, M.; Muñoz, R.; Navas, E.; Moya, J.L.; et al. Mortality risk prediction in infective endocarditis surgery: Reliability analysis of specific scores. Eur. J. Cardio Thorac. Surg. 2018, 53, 1049–1054. [Google Scholar] [CrossRef]
- Perrotta, S.; Jeppsson, A.; Fröjd, V.; Svensson, G. Surgical Treatment of Aortic Prosthetic Valve Endocarditis: A 20-Year Single-Center Experience. Ann. Thorac. Surg. 2016, 101, 1426–1432. [Google Scholar] [CrossRef] [Green Version]
- Saha, S.; Dudakova, A.; Danner, B.C.; Kutschka, I.; Schulze, M.H.; Niehaus, H. Bacterial Spectrum and Infective Foci in Patients Operated for Infective Endocarditis: Time to Rethink Strategies? Thorac. Cardiovasc. Surg. 2022. [Google Scholar] [CrossRef]
- Nashef, S.A.M.; Roques, F.; Sharples, L.D.; Nilsson, J.; Smith, C.; Goldstone, A.R.; Lockowandt, U. Euroscore II. Eur. J. Cardio Thorac. Surg. 2012, 41, 734–745. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Di Mauro, M.; Dato, G.M.A.; Barili, F.; Gelsomino, S.; Santè, P.; Della Corte, A.; Carrozza, A.; Della Ratta, E.; Cugola, D.; Galletti, L.; et al. A predictive model for early mortality after surgical treatment of heart valve or prosthesis infective endocarditis. The EndoSCORE. Int. J. Cardiol. 2017, 241, 97–102. [Google Scholar] [CrossRef] [PubMed]
- Olmos, C.; Vilacosta, I.; Habib, G.; Maroto, L.; Fernández, C.; López, J.; Sarriá, C.; Salaun, E.; Di Stefano, S.; Carnero, M.; et al. Risk score for cardiac surgery in active left-sided infective endocarditis. Heart 2017, 103, 1435–1442. [Google Scholar] [CrossRef] [Green Version]
- De Feo, M.; Cotrufo, M.; Carozza, A.; De Santo, L.S.; Amendolara, F.; Giordano, S.; Della Ratta, E.E.; Nappi, G.; Della Corte, A. The need for a specific risk prediction system in native valve infective endocarditis surgery. Sci. World J. 2012, 2012, 307571. [Google Scholar] [CrossRef] [PubMed]
- Park, L.P.; Chu, V.H.; Peterson, G.; Skoutelis, A.; Lejko-Zupa, T.; Bouza, E.; Tattevin, P.; Habib, G.; Tan, R.; Gonzalez, J.; et al. Validated risk score for predicting 6-month mortality in infective endocarditis. J. Am. Heart Assoc. 2016, 5, e003016. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Habib, G. Infective endocarditis after transcatheter aortic valve replacement: The worst that can happen. J. Am. Heart Assoc. 2018, 7, e010287. [Google Scholar] [CrossRef]
- Fukuhara, S.; Brescia, A.A.; Shiomi, S.; Rosati, C.M.; Yang, B.; Kim, K.M.; Deeb, G.M. Surgical explantation of transcatheter aortic bioprostheses: Results and clinical implications. J. Thorac. Cardiovasc. Surg. 2020, 162, 539–547. [Google Scholar] [CrossRef]
- Saha, S.; Joskowiak, D.; Marin-Cuartas, M.; Diab, M.; Schwaiger, B.M.; Sandoval-Boburg, R.; Popov, A.-F.; Weber, C.; Varghese, S.; Martens, A.; et al. Surgery for infective endocarditis following low-intermediate risk transcatheter aortic valve replacement-a multicentre experience. Eur. J. Cardio Thorac. Surg. 2022. [Google Scholar] [CrossRef]
- Mangner, N.; Leontyev, S.; Woitek, F.J.; Kiefer, P.; Haussig, S.; Binner, C.; Mende, M.; Schlotter, F.; Stachel, G.; Höllriegel, R.; et al. Cardiac Surgery Compared With Antibiotics Only in Patients Developing Infective Endocarditis After Transcatheter Aortic Valve Replacement. J. Am. Heart Assoc. 2018, 7, e010027. [Google Scholar] [CrossRef]
- Chourdakis, E.; Koniari, I.; Hahalis, G.; Kounis, N.G.; Hauptmann, K.E. Endocarditis after transcatheter aortic valve implantation: A current assessment. J. Geriatr. Cardiol. 2018, 15, 61–65. [Google Scholar]
- Kuttamperoor, F.; Yandrapalli, S.; Siddhamsetti, S.; Frishman, W.H.; Tang, G.H.L. Infectious Endocarditis after Transcatheter Aortic Valve Replacement: Epidemiology and Outcomes. Cardiol. Rev. 2019, 27, 236–241. [Google Scholar] [CrossRef] [PubMed]
- Davierwala, P.M.; Marin-Cuartas, M.; Misfeld, M.; Borger, M.A. The value of an “Endocarditis Team”. Ann. Cardiothorac. Surg. 2019, 8, 621–629. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Gomes, A.; Jainandunsing, J.S.; van Assen, S.; van Geel, P.P.; Sinha, B.; Gelsomino, S.; Johnson, D.M.; Natour, E. A standardized approach to treat complex aortic valve endocarditis: A case series. J. Cardiothorac. Surg. 2018, 13, 32. [Google Scholar] [CrossRef] [PubMed]
- Prendki, V. Management of elderly patients with infective endocarditis. Clin. Microbiol. Infect. 2019, 25, 1169–1170. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Saha, S.; Varghese, S.; Al Ahmad, A.; Jebran, A.F.; Waezi, N.; Niehaus, H.; Baraki, H.; Kutschka, I. Complex Valve Surgery in Elderly Patients: Increasingly Necessary and Surprisingly Feasible. Thorac. Cardiovasc. Surg. 2020, 68, 107–113. [Google Scholar] [CrossRef]



| SAVR–PVE (n = 98) | TIE (n = 22) | p-Value | |
|---|---|---|---|
| Age, (years) | 69 (58–76) | 77 (70–80) | 0.010 |
| BMI (kg/m2) | 25.7 (24.3–27.2) | 25.7 (24.3–27.2) | 0.645 |
| Male (%) | 88 (89.8) | 18 (81.8) | 0.285 |
| NYHA class | 0.073 | ||
| 21 (21.4) | 1 (4.5) | |
| 77 (78.6) | 21 (95.5) | |
| Charlson Comorbidity Index | 5 (4–7) | 7 (6–8) | 0.005 |
| Arterial hypertension (%) | 76 (77.6) | 19 (86.4) | 0.560 |
| Hyperlipoproteinemia (%) | 50 (51.0) | 15 (68.1) | 0.235 |
| Coronary artery disease (%) | 0.966 | ||
| One-vessel disease (%) | 10 (10.2) | 1 (4.5) | |
| Two-vessel disease (%) | 15 (15.3) | 2 (9.1) | |
| Three-vessel disease (%) | 15 (15.3) | 5 (22.7) | |
| PCI within 90 days (%) | 6 (6.1) | 1 (4.5) | 1.000 |
| Diabetes mellitus (%) | 27 (27.6) | 7 (31.8) | 0.794 |
| Chronic kidney disease (%) | 26 (26.5) | 10 (45.5) | 0.120 |
| Dialysis (%) | 3 (3.1) | 3 (13.6) | 0.074 |
| Creatinine clearance (mL/min) | 54 (41–75) | 49 (33–69) | 0.201 |
| Smoker (%) | 22 (22.4) | 7 (31.8) | 0.410 |
| COPD (%) | 11 (11.2) | 4 (18.2) | 0.473 |
| Pacemaker (%) | 12 (12.2) | 9 (40.9) | 0.003 |
| Atrial fibrillation (%) | 23 (23.5) | 7 (31.8) | 0.423 |
| Peripheral vascular disease (%) | 9 (9.2) | 5 (22.7) | 0.133 |
| Preoperative cerebral emboli (%) | 14 (14.3) | 3 (13.6) | 1.000 |
| Intravenous drug use (%) | 2 (2.0) | 0 (0.0) | 1.000 |
| HIV infection (%) | 1 (1.0) | 0 (0.0) | 1.000 |
| Chronic steroid therapy (%) | 1 (1.0) | 3 (13.6) | 0.019 |
| Previous malignancy (%) | 13 (13.3) | 5 (22.7) | 0.320 |
| Alcohol abuse (%) | 8 (8.2) | 2 (9.1) | 1.000 |
| Preoperative ventilation (%) | 6 (6.1) | 0 (0.0) | 0.591 |
| Preoperative LCOS (%) | 9 (9.2) | 1 (4.5) | 0.687 |
| Previous open cardiac surgery (%) | 98 (100.0) | 9 (40.9) | <0.001 |
| Previous endocarditis (%) | 11 (11.2) | 1 (4.5) | 0.693 |
| Time to PVE (years) | 3.7 (0.8–9.5) | 1.2 (0.4–2.8) | 0.001 |
| Early PVE (%) | 27 (27.6) | 11 (50.0) | 0.073 |
| SAVR–PVE (n = 98) | TIE (n = 22) | p-Value | |
|---|---|---|---|
| Non-Specific Scores | |||
| STS PROM | 1.8 (1.6–2.1) | 1.9 (1.4–2.2) | 0.622 |
| EuroSCORE II | 52.1 (40.6–62.0) | 45.4 (32.6–58.1) | 0.207 |
| Specific Risk Scores | |||
| Risk E score | 24.2 (19.5–38.2) | 31.0 (21.3–39.6) | 0.419 |
| Endoscore | 7.2 (4.5–12.6) | 7.2 (4.3–12.6) | 0.601 |
| DeFeo Score | 17 (14–21) | 20 (16–23) | 0.132 |
| Mid-Term Mortality Risk Score | |||
| ICE Score | 37.4 (25.7–45.0) | 39.8 (33.7–46.3) | 0.207 |
| SAVR–PVE (n = 98) | TIE (n = 22) | p-Value | |
|---|---|---|---|
| LVEF | 0.554 | ||
| 41 (41.8) | 9 (40.9) | |
| 50 (51.0) | 9 (40.9) | |
| 7 (7.1) | 4 (18.2) | |
| Paravalvular leakage (%) | 12 (12.2) | 8 (36.4) | 0.013 |
| Aortic Stenosis | 0.462 | ||
| 2 (2.0) | 0 (0.0) | |
| 10 (10.2) | 4 (18.2) | |
| Aortic Regurgitation | 0.072 | ||
| 37 (37.8) | 2 (9.1) | |
| 13 (13.3) | 12 (54.5) | |
| Mitral regurgitation | 0.085 | ||
| 28 (28.6) | 4 (18.2) | |
| 25 (25.5) | 10 (45.5) | |
| Tricuspid regurgitation | 0.346 | ||
| 33 (33.7) | 6 (27.3) | |
| 3 (3.1) | 4 (18.2) | |
| Pulmonary hypertension (%) | 12 (12.2) | 5 (22.7) | 0.306 |
| Presence of vegetations (%) | 76 (77.6) | 13 (59.1) | 0.104 |
| Size of vegetations | 0.022 | ||
| 13 (13.3) | 3 (13.6) | |
| 21 (21.4) | 6 (27.3) | |
| 42 (42.9) | 4 (18.2) | |
| Abscess (%) | 39 (39.8) | 6 (27.3) | 0.335 |
| Pathogen | SAVR–PVE (n = 98) | TIE (n = 22) | p-Value |
|---|---|---|---|
| BCNIE | 27 (27.8) | 1 (4.5) | 0.024 |
| Gram-positive organisms | |||
| Enterococcus sp. | 15 (15.3) | 6 (27.3) | 0.215 |
| Enterococcus faecalis | 13 (13.3) a | 5 (22.7) | |
| Enterococcus faecium | 2 (2.0) | 1 (4.5) | |
| Staphylococcus aureus | 18 (18.4) | 4 (18.2) | 1.000 |
| MRSA | 1 (1.0) | 0 (0.0) | |
| MSSA | 17 (17.3) | 4 (18.2) | |
| Staphylococcus lugdunensis | 1 (1.0) | 0 (0.0) | 1.000 |
| Other CoNS b | 5 (5.1) | 7 (31.8) c | 0.001 |
| Streptococcus sp. | 12 (12.2) | 2 (9.1) | 1.000 |
| Streptococcus Group B d | 2 (2.0) | 0 (0.0) | |
| Streptococcus Group D e | 1 (1.0) | 0 (0.0) | |
| Orally occurring viridans streptococci f | 7 (7.1) g | 2 (9.1) | |
| Viridans streptococci not defined | 2 (2.0) | 0 (0.0) | |
| Micrococcus luteus | 1 (1.0) | 0 (0.0) | 1.000 |
| Lactococcus garvieae | 1 (1.0) | 0 (0.0) | 1.000 |
| Lactobacillus paracasei | 1 (1.0) | 0 (0.0) | 1.000 |
| Cutibacterium acnes | 11 (11.2) | 1 (4.5) | 0.693 |
| Parvimonas micra | 1 (1.0) | 0 (0.0) | 1.000 |
| Gram-negative organisms | |||
| HACEK group h | 1 (1.0) | 1 (4.5) | 0.334 |
| Moraxella catarrhalis | 1 (1.0) | 0 (0.0) | 1.000 |
| PVE (n = 98) | TIE (n = 22) | p-Value | |
|---|---|---|---|
| Details of surgery | |||
| Cardiopulmonary bypass time (min) | 203 (149–271) | 127 (87–232) | 0.005 |
| Cross-clamp time (min) | 134 (106–169) | 95 (58–168) | 0.003 |
| Bentall procedures (%) | 34 (34.7) | 1 (4.5) | 0.004 |
| Repair of aortomitral curtain (%) | 2 (2.0) | 1 (4.5) | 0.458 |
| Aortic root enlargement (%) | 0 (0.0) | 1 (4.5) | 0.183 |
| Patch repair (%) | 19 (19.4) | 3 (13.6) | 0.762 |
| Aortic valve replacement | 0.669 | ||
| Biological prosthesis (%) | 91 (92.9) | 20 (90.9) | |
| Mechanical prosthesis (%) | 7 (7.1) | 2 (9.1) | |
| Concomitant procedures | |||
| Mitral valve replacement (%) | 18 (18.4) | 5 (22.7) | 0.499 |
| Mitral valve repair (%) | 2 (2.0) | 0 (0.0) | 1.000 |
| Tricuspid valve replacement (%) | 3 (3.1) | 0 (0.0) | 1.000 |
| Tricuspid valve repair (%) | 2 (2.0) | 1 (4.5) | 0.458 |
| CABG procedure | 8 (8.2) | 1 (4.5) | 1.000 |
| Morbidities | |||
| Adverse cerebrovascular events (%) | 26 (26.5) | 4 (18.2) | 0.431 |
| Severe bleeding with re-exploration (%) | 20 (20.4) | 4 (18.2) | 1.000 |
| Surgical site infection (%) | 3 (3.1) | 0 (0.0) | 1.000 |
| Tracheostomy (%) | 10 (10.2) | 3 (13.6) | 0.709 |
| Pacemaker implantation (%) | 26 (26.5) | 5 (22.7) | 0.792 |
| Renal replacement therapy (%) | 18 (18.4) | 8 (36.4) | 0.091 |
| LCOS (%) | 16 (16.3) | 7 (31.8) | 0.137 |
| Septic shock (%) | 24 (24.5) | 7 (31.8) | 0.430 |
| ECLS support (%) | 17 (17.3) | 2 (9.1) | 0.521 |
| IABP (%) | 4 (4.1) | 1 (4.5) | 1.000 |
| Outcomes | |||
| In-hospital mortality (%) | 26 (26.5) | 2 (9.1) | 0.098 |
| Length of hospital stay (days) | 19 (14–33) | 23 (16–37) | 0.234 |
| Length of ICU stay (days) | 5 (2–9) | 4 (3–14) | 0.953 |
| Length of PMV (hours) | 19 (12–75) | 20 (13–113) | 0.612 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Saha, S.; Ali, A.; Schnackenburg, P.; Horke, K.M.; Oberbach, A.; Schlichting, N.; Sadoni, S.; Rizas, K.; Braun, D.; Luehr, M.; et al. Surgery for Aortic Prosthetic Valve Endocarditis in the Transcatheter Era. J. Clin. Med. 2022, 11, 3418. https://doi.org/10.3390/jcm11123418
Saha S, Ali A, Schnackenburg P, Horke KM, Oberbach A, Schlichting N, Sadoni S, Rizas K, Braun D, Luehr M, et al. Surgery for Aortic Prosthetic Valve Endocarditis in the Transcatheter Era. Journal of Clinical Medicine. 2022; 11(12):3418. https://doi.org/10.3390/jcm11123418
Chicago/Turabian StyleSaha, Shekhar, Ahmad Ali, Philipp Schnackenburg, Konstanze Maria Horke, Andreas Oberbach, Nadine Schlichting, Sebastian Sadoni, Konstantinos Rizas, Daniel Braun, Maximilian Luehr, and et al. 2022. "Surgery for Aortic Prosthetic Valve Endocarditis in the Transcatheter Era" Journal of Clinical Medicine 11, no. 12: 3418. https://doi.org/10.3390/jcm11123418
APA StyleSaha, S., Ali, A., Schnackenburg, P., Horke, K. M., Oberbach, A., Schlichting, N., Sadoni, S., Rizas, K., Braun, D., Luehr, M., Bagaev, E., Hagl, C., & Joskowiak, D. (2022). Surgery for Aortic Prosthetic Valve Endocarditis in the Transcatheter Era. Journal of Clinical Medicine, 11(12), 3418. https://doi.org/10.3390/jcm11123418