Prospective, Long-Term Functional Outcomes of Extra-Osseous Talotarsal Stabilization (EOTTS) Using HyProCure in Adult Patients with Talotarsal Joint Instability: Assessment of Physical Activity and Patient Satisfaction
Abstract
:1. Introduction
2. Materials and Methods
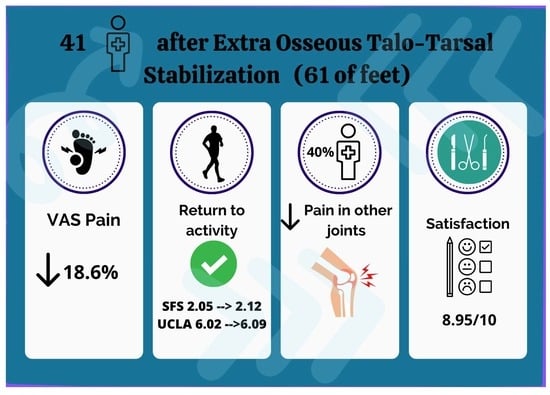
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Huson, A. Biomechanics of the Tarsal Mechanism. A Key to the Function of the Normal Human Foot. J. Am. Podiatr. Med. Assoc. 2000, 90, 12–17. [Google Scholar] [CrossRef] [PubMed]
- Graham, M.E.; Jawrani, N.T.; Chikka, A. Extraosseous Talotarsal Stabilization Using HyProCure® in Adults: A 5-Year Retrospective Follow-Up. J. Foot Ankle Surg. 2012, 51, 23–29. [Google Scholar] [CrossRef] [PubMed]
- Leung, A.K.; Mak, A.F.; Evans, J.H. Biomedical Gait Evaluation of the Immediate Effect of Orthotic Treatment for Flexible Flat Foot. Prosthet. Orthot. Int. 1998, 22, 25–34. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Blackwood, C.B.; Yuen, T.J.; Sangeorzan, B.J.; Ledoux, W.R. The Midtarsal Joint Locking Mechanism. Foot Ankle Int. 2005, 26, 1074–1080. [Google Scholar] [CrossRef]
- Biz, C.; Baldin, G.; Cappelletto, C.; Bragazzi, N.L.; Nicoletti, P.; Crimì, A.; Ruggieri, P. Isolated Medial Subtalar Joint Dislocation during Sports Activities: A Systematic Review of the Literature with Individual Participant Data Analysis. Osteology 2021, 1, 48–61. [Google Scholar] [CrossRef]
- Pereira, B.S.; Andrade, R.; Espregueira-Mendes, J.; Marano, R.P.C.; Oliva, X.M.; Karlsson, J. Current Concepts on Subtalar Instability. Orthop. J. Sports Med. 2021, 9, 23259671211021352. [Google Scholar] [CrossRef]
- Khamis, S.; Yizhar, Z. Effect of Feet Hyperpronation on Pelvic Alignment in a Standing Position. Gait Posture 2007, 25, 127–134. [Google Scholar] [CrossRef] [PubMed]
- Giannini, S.; Catani, F.; Ceccarelli, F.; Girolami, M.; Benedetti, M.G. Kinematic and Isokinetic Evaluation of Patients with Flat Foot. Ital. J. Orthop. Traumatol. 1992, 18, 241–251. [Google Scholar]
- Inman, V.T. The Influence of the Foot-Ankle Complex on the Proximal Skeletal Structures. Artif. Limbs 1969, 13, 59–65. [Google Scholar]
- Kolodziej, L.; Summers, R.K.; Graham, M.E. The Effect of Extra-Osseous Talotarsal Stabilization (EOTTS) to Reduce Medial Knee Compartment Forces—An in Vivo Study. PLoS ONE 2019, 14, e0224694. [Google Scholar] [CrossRef] [Green Version]
- Saito, E.T.; Akashi, P.M.H.; de Camargo Neves Sacco, I. Global Body Posture Evaluation in Patients with Temporomandibular Joint Disorder. Clinics 2009, 64, 35–39. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Gross, K.D.; Felson, D.T.; Niu, J.; Hunter, D.J.; Guermazi, A.; Roemer, F.W.; Dufour, A.B.; Gensure, R.H.; Hannan, M.T. Flat Feet Are Associated With Knee Pain and Cartilage Damage in Older Adults. Arthritis Care Res. 2011, 63, 937–944. [Google Scholar] [CrossRef] [Green Version]
- Tiberio, D. The Effect of Excessive Subtalar Joint Pronation on Patellofemoral Mechanics: A Theoretical Model. J. Orthop. Sports Phys. Ther. 1987, 9, 160–165. [Google Scholar] [CrossRef] [Green Version]
- Uden, H.; Scharfbillig, R.; Causby, R. The Typically Developing Paediatric Foot: How Flat Should It Be? A Systematic Review. J. Foot Ankle Res. 2017, 10, 37. [Google Scholar] [CrossRef] [Green Version]
- Stovitz, S.D.; Coetzee, J.C. Hyperpronation and Foot Pain: Steps toward Pain-Free Feet. Phys. Sportsmed. 2004, 32, 19–26. [Google Scholar] [CrossRef] [PubMed]
- Graham, M.E.; Jawrani, N.T.; Chikka, A.; Rogers, R.J. Surgical Treatment of Hyperpronation Using an Extraosseous Talotarsal Stabilization Device: Radiographic Outcomes in 70 Adult Patients. J. Foot Ankle Surg. 2012, 51, 548–555. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Schon, L.C. Subtalar Arthroereisis: A New Exploration of an Old Concept. Foot Ankle Clin. 2007, 12, 329–339. [Google Scholar] [CrossRef]
- Viladot, R.; Pons, M.; Alvarez, F.; Omaña, J. Subtalar Arthroereisis for Posterior Tibial Tendon Dysfunction: A Preliminary Report. Foot Ankle Int. 2003, 24, 600–606. [Google Scholar] [CrossRef]
- Needleman, R.L. Current Topic Review: Subtalar Arthroereisis for the Correction of Flexible Flatfoot. Foot Ankle Int. 2005, 26, 336–346. [Google Scholar] [CrossRef]
- Graham, M.E.; Jawrani, N.T. Extraosseous Talotarsal Stabilization Devices: A New Classification System. J. Foot Ankle Surg. 2012, 51, 613–619. [Google Scholar] [CrossRef]
- Pagenstert, G.; Leumann, A.; Hintermann, B.; Valderrabano, V. Sports and Recreation Activity of Varus and Valgus Ankle Osteoarthritis before and after Realignment Surgery. Foot Ankle Int. 2008, 29, 985–993. [Google Scholar] [CrossRef]
- Steber, S.J. Analysis of Radiographic Outcomes Comparing Foot Orthosis to Extra-Osseous Talotarsal Stabilization in the Treatment of Recurrent Talotarsal Joint Dislocation. J. Minim. Invasive Orthop. 2015, 1, 1–11. [Google Scholar] [CrossRef] [Green Version]
- Martinelli, N.; Bianchi, A.; Martinkevich, P.; Sartorelli, E.; Romeo, G.; Bonifacini, C.; Malerba, F. Return to Sport Activities after Subtalar Arthroereisis for Correction of Pediatric Flexible Flatfoot. J. Pediatr. Orthop. B 2018, 27, 82. [Google Scholar] [CrossRef] [PubMed]
- Herdea, A.; Neculai, A.-G.; Ulici, A. The Role of Arthroereisis in Improving Sports Performance, Foot Aesthetics and Quality of Life in Children and Adolescents with Flexible Flatfoot. Children 2022, 9, 973. [Google Scholar] [CrossRef]
- Feng, P.; Li, J.; Ouyang, X.; Gao, F.; Zhang, H. Short-term effectiveness of hyprocure subtalar stabilization in treatment of adolescent flexible flatfoot. Zhongguo Xiu Fu Chong Jian Wai Ke Za Zhi 2016, 30, 975–979. [Google Scholar] [CrossRef] [PubMed]
- Chen, C.; Jiang, J.; Fu, S.; Wang, C.; Su, Y.; Mei, G.; Xue, J.; Zou, J.; Li, X.; Shi, Z. HyProCure for Pediatric Flexible Flatfoot: What Affects the Outcome. Front. Pediatr. 2022, 10, 857458. [Google Scholar] [CrossRef]
- Kheyrandish, I.; Hadadnezhad, M.; Shojaedin, S.S. Comparison of Functional Lower Extremity Evaluation Scores in Active Adolescents with Normal and Flexible Flat Foot. Sci. J. Rehabil. Med. 2019, 7, 198–207. [Google Scholar] [CrossRef]
- Merkle, S.L.; Sluka, K.A.; Frey-Law, L.A. The Interaction between Pain and Movement. J. Hand Ther. 2020, 33, 60–66. [Google Scholar] [CrossRef]
- Fujita, T.; Hamai, S.; Shiomoto, K.; Okazawa, K.; Nasu, Y.; Hara, D.; Harada, S.; Motomura, G.; Ikemura, S.; Fujii, M.; et al. Analysis of Factors Influencing Patient Satisfaction after Total Hip Arthroplasty in a Japanese Cohort: The Significant Effect of Postoperative Physical Activity. J. Phys. Ther. Sci. 2022, 34, 76–84. [Google Scholar] [CrossRef]
- Ciechanowicz, D.; Kozłowski, J.; Kołodziej, Ł.; Kromuszczyńska, J. Return to Physical Activities after Scarf Osteotomy for Hallux Valgus. Ortop. Traumatol. Rehabil. 2020, 22, 95–106. [Google Scholar] [CrossRef]
- Martinelli, N.; Bianchi, A.; Prandoni, L.; Maiorano, E.; Sansone, V. Quality of Life in Young Adults after Flatfoot Surgery: A Case-Control Study. J. Clin. Med. 2021, 10, 451. [Google Scholar] [CrossRef] [PubMed]
- Fuller, R.M.; Eble, S.K.; Day, J.; Cororaton, A.D.; Rajan, L.; Deland, J.T.; Kumar, P.; Ellis, S.J. Return to Physical Activity Following Flatfoot Reconstruction. Foot Ankle Int. 2022, 43, 772–782. [Google Scholar] [CrossRef] [PubMed]
- Rao, S.; Riskowski, J.; Hannan, M.T. Musculoskeletal Conditions of the Foot and Ankle: Assessments and Treatment Options. Best Pract. Res. Clin. Rheumatol. 2012, 26, 345–368. [Google Scholar] [CrossRef] [Green Version]
- Gross, K.D.; Niu, J.; Zhang, Y.Q.; Felson, D.T.; McLennan, C.; Hannan, M.T.; Holt, K.G.; Hunter, D.J. Varus Foot Alignment and Hip Conditions in Older Adults. Arthritis Rheum. 2007, 56, 2993–2998. [Google Scholar] [CrossRef]
- Ålund, M. Subtalar Arthroereisis as a Surgical Option in the Reconstruction of Progressive Collapsing Foot Deformity: A Prospective 3-Year Follow-up Study on Patient Satisfaction and Causes for Implant Removal in 40 Cases Treated with the HyProCure Implant. J. Foot Ankle Surg. 2023, 10, 92–101. [Google Scholar] [CrossRef]
- Bresnahan, P.J.; Chariton, J.T.; Vedpathak, A. Extraosseous Talotarsal Stabilization Using HyProCure®: Preliminary Clinical Outcomes of a Prospective Case Series. J. Foot Ankle Surg. 2013, 52, 195–202. [Google Scholar] [CrossRef] [Green Version]




| Symptom-Related Ankle Activity Scale (SAAS) | Pre-Operative (n, %) | Post-Operative (n, %) |
|---|---|---|
| 0 = no ADL, disabled by ankle | 0 (0%) | 0 (0%) |
| 20 = symptoms with ADL, not disabled; sedentary work and walking on even ground possible | 1 (2.4%) | 0 (0%) |
| 40 = no symptoms with ADL; light work (e.g., nursing), swimming, walking on uneven ground possible | 3 (7.3%) | 3 (7.3%) |
| 60 = no symptoms with light work; moderate work (e.g., truck driving, heavy domestic work), recreational jogging, skiing, cycling possible | 17 (41.5%) | 6 (14.6%) |
| 80 = no symptoms with moderate work; strenuous work (e.g., building, forestry), jogging on uneven ground, competitive cycling, skiing possible | 11 (26.8%) | 14 (34.1%) |
| 100 = no symptoms with strenuous work, all recreational and competitive sports possible (e.g., soccer) | 9 (22.0%) | 18 (44.0%) |
| Pre-Operative | Post-Operative | p Value | |
|---|---|---|---|
| Number of physical activities [x/week], mean (SD) | 1.95 (±1.1) | 1.83 (±1.0) | 0.372 |
| Time of physical activity [min/week], mean (SD) | 153.7 (±126.3) | 170 (±102) | 0.145 |
| UCLA activity score, mean (SD) | 6.02 (±2.7) | 6.09 (±2.5) | 0.787 |
| SAAS, mean (SD) | 71.7 (±20.0) | 82.9 (±18.7) | 0.002 |
| LEFS, mean (SD) | 74.2 (±23.7) | 88.6 (±15.3) | 0.0006 |
| VAS, mean (SD) | 4.6 (±3.3) | 0.9 (±1.5) | <0.0001 |
| Physical Activity | Pre-Operative | Post-Operative | Change | Joint-Stress Activities |
|---|---|---|---|---|
| Walking | 19 | 19 | 0 | Low |
| Cycling | 17 | 17 | 0 | Low |
| Swimming | 7 | 7 | 0 | Low |
| Running | 6 | 6 | 0 | High |
| Weightlifting | 6 | 7 | +1 | High |
| Fitness | 6 | 4 | −2 | High |
| Nordic Walking | 4 | 4 | 0 | High |
| Skiing | 4 | 3 | −1 | High |
| Dance | 2 | 2 | 0 | High |
| Volleyball | 2 | 1 | −1 | High |
| Mountain trekking | 1 | 0 | −1 | High |
| Go-karts | 1 | 0 | −1 | Low |
| Canoeing | 1 | 0 | −1 | Low |
| Climbing | 1 | 1 | 0 | High |
| Martial arts | 1 | 1 | 0 | High |
| Squash | 1 | 1 | 0 | High |
| Time of Physical Activity [min/week], | Number of Physical Activities [x/week] | UCLA | SAAS | VAS | Satisfaction | LEFS | |
|---|---|---|---|---|---|---|---|
| MFS score | 0.2203 | 0.0981 | 0.0862 | 0.3241 | −0.4427 | 0.2552 | −0.1240 |
| p = 0.166 | p = 0.542 | p = 0.592 | p = 0.039 | p = 0.004 | p = 0.107 | p = 0.440 | |
| Pain | 0.2573 | 0.0287 | −0.1125 | 0.1418 | −0.5228 | 0.1284 | −0.1203 |
| p = 0.104 | p = 0.859 | p = 0.484 | p = 0.377 | p = 0.000 | p = 0.424 | p = 0.454 | |
| Distance walked | 0.2248 | 0.1687 | 0.0089 | 0.1581 | −0.0982 | 0.4231 | 0.0603 |
| p = 0.158 | p = 0.292 | p = 0.956 | p = 0.323 | p = 0.541 | p = 0.006 | p = 0.708 | |
| Stability | 0.0245 | 0.0096 | 0.1120 | 0.0520 | 0.0780 | −0.0532 | 0.1346 |
| p = 0.879 | p = 0.953 | p = 0.486 | p = 0.747 | p = 0.628 | p = 0.741 | p = 0.402 | |
| Support | -- | -- | -- | -- | -- | -- | -- |
| p = --- | p = --- | p = --- | p = --- | p = --- | p = --- | p = --- | |
| Limp | 0.2248 | 0.1687 | 0.0089 | 0.1581 | −0.0982 | 0.4231 | 0.0603 |
| p = 0.158 | p = 0.292 | p = 0.956 | p = 0.323 | p = 0.541 | p = 0.006 | p = 0.708 | |
| Shoes | 0.0137 | −0.0209 | 0.0995 | 0.3637 | −0.1795 | 0.1759 | −0.1324 |
| p = 0.932 | p = 0.897 | p = 0.536 | p = 0.019 | p = 0.261 | p = 0.271 | p = 0.409 | |
| Stairs | 0.1487 | 0.0305 | 0.3123 | 0.4492 | −0.0276 | 0.4996 | −0.0439 |
| p = 0.353 | p = 0.850 | p = 0.047 | p = 0.003 | p = 0.864 | p = 0.001 | p = 0.785 | |
| Terrain | −0.0404 | 0.1270 | 0.2367 | 0.1117 | −0.0921 | −0.1227 | −0.0233 |
| p = 0.802 | p = 0.429 | p = 0.136 | p = 0.487 | p = 0.567 | p = 0.445 | p = 0.885 | |
| Cosmesis | −0.1099 | 0.1178 | 0.1969 | −0.1458 | 0.0905 | −0.0042 | −0.1195 |
| p = 0.494 | p = 0.463 | p = 0.217 | p = 0.363 | p = 0.573 | p = 0.979 | p = 0.457 | |
| Motion | -- | -- | -- | -- | -- | -- | -- |
| p = --- | p = --- | p = --- | p = --- | p = --- | p = --- | p = --- |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kołodziej, Ł.; Ciechanowicz, D.; Wójtowicz, M.; Król, M.; Szabałowska, M.; Kwiatkowski, S.; Szymczak, M.; Czajka, R. Prospective, Long-Term Functional Outcomes of Extra-Osseous Talotarsal Stabilization (EOTTS) Using HyProCure in Adult Patients with Talotarsal Joint Instability: Assessment of Physical Activity and Patient Satisfaction. J. Clin. Med. 2023, 12, 4872. https://doi.org/10.3390/jcm12144872
Kołodziej Ł, Ciechanowicz D, Wójtowicz M, Król M, Szabałowska M, Kwiatkowski S, Szymczak M, Czajka R. Prospective, Long-Term Functional Outcomes of Extra-Osseous Talotarsal Stabilization (EOTTS) Using HyProCure in Adult Patients with Talotarsal Joint Instability: Assessment of Physical Activity and Patient Satisfaction. Journal of Clinical Medicine. 2023; 12(14):4872. https://doi.org/10.3390/jcm12144872
Chicago/Turabian StyleKołodziej, Łukasz, Dawid Ciechanowicz, Maria Wójtowicz, Marta Król, Małgorzata Szabałowska, Sebastian Kwiatkowski, Mateusz Szymczak, and Radomir Czajka. 2023. "Prospective, Long-Term Functional Outcomes of Extra-Osseous Talotarsal Stabilization (EOTTS) Using HyProCure in Adult Patients with Talotarsal Joint Instability: Assessment of Physical Activity and Patient Satisfaction" Journal of Clinical Medicine 12, no. 14: 4872. https://doi.org/10.3390/jcm12144872
APA StyleKołodziej, Ł., Ciechanowicz, D., Wójtowicz, M., Król, M., Szabałowska, M., Kwiatkowski, S., Szymczak, M., & Czajka, R. (2023). Prospective, Long-Term Functional Outcomes of Extra-Osseous Talotarsal Stabilization (EOTTS) Using HyProCure in Adult Patients with Talotarsal Joint Instability: Assessment of Physical Activity and Patient Satisfaction. Journal of Clinical Medicine, 12(14), 4872. https://doi.org/10.3390/jcm12144872