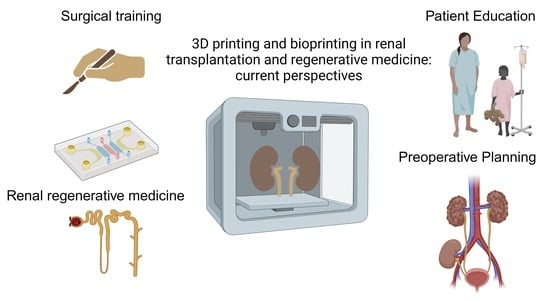
Three-Dimensional Printing and Bioprinting in Renal Transplantation and Regenerative Medicine: Current Perspectives
Abstract
:1. Introduction
2. Search Strategy
- Our foremost objective was to comprehensively identify all relevant studies that employ 3D printing techniques within the context of renal transplantation.
- A secondary aim was to encompass additional literature pertaining to skills and methodologies applicable to the field of renal transplantation.
- Lastly, we aimed to present a comprehensive review of the existing literature on the state of bioprinting in the realm of renal regenerative medicine.
3. Three-Dimensional Printing in Renal Transplantation
3.1. Educational Purposes
3.1.1. Surgical Training—Core Skills
3.1.2. Surgical Training—Further Skills
3.1.3. Patient Education
3.2. Preoperative Planning
4. Bioprinting in Renal Regenerative Medicine
5. Discussion
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Those 2020 data are based on the Global Observatory on Donation and Transplantation (GODT) data, produced by the WHO-ONT collaboration. Available online: https://www.transplant-observatory.org/ (accessed on 7 August 2023).
- Tonelli, M.; Wiebe, N.; Knoll, G.; Bello, A.; Browne, S.; Jadhav, D.; Klarenbach, S.; Gill, J. Systematic Review: Kidney Transplantation Compared with Dialysis in Clinically Relevant Outcomes. Am. J. Transplant. 2011, 11, 2093–2109. [Google Scholar] [CrossRef]
- Akbar, S.A.; Jafri, S.Z.H.; Amendola, M.A.; Madrazo, B.L.; Salem, R.; Bis, K.G. Complications of Renal Transplantation. Radiographics 2005, 25, 1335–1356. [Google Scholar] [CrossRef]
- Mitsouras, D.; Liacouras, P.; Imanzadeh, A.; Giannopoulos, A.A.; Cai, T.; Kumamaru, K.K.; George, E.; Wake, N.; Caterson, E.J.; Pomahac, B.; et al. Medical 3D Printing for the Radiologist. Radiographics 2015, 35, 1965–1988. [Google Scholar] [CrossRef]
- Pietrabissa, A.; Marconi, S.; Negrello, E.; Mauri, V.; Peri, A.; Pugliese, L.; Marone, E.M.; Auricchio, F. An Overview on 3D Printing for Abdominal Surgery. Surg. Endosc. 2020, 34, 1–13. [Google Scholar] [CrossRef] [PubMed]
- Christou, C.D.; Tsoulfas, G. Role of Three-Dimensional Printing and Artificial Intelligence in the Management of Hepatocellular Carcinoma: Challenges and Opportunities. World J. Gastrointest. Oncol. 2022, 14, 765–793. [Google Scholar] [CrossRef] [PubMed]
- Hart, A.; Lentine, K.L.; Smith, J.M.; Miller, J.M.; Skeans, M.A.; Prentice, M.; Robinson, A.; Foutz, J.; Booker, S.E.; Israni, A.K.; et al. OPTN/SRTR 2019 Annual Data Report: Kidney. Am. J. Transplant. 2021, 21, 21–137. [Google Scholar] [CrossRef]
- Hospodiuk, M.; Dey, M.; Sosnoski, D.; Ozbolat, I.T. The Bioink: A Comprehensive Review on Bioprintable Materials. Biotechnol. Adv. 2017, 35, 217–239. [Google Scholar] [CrossRef]
- Zadpoor, A.A.; Malda, J. Additive Manufacturing of Biomaterials, Tissues, and Organs. Ann. Biomed. Eng. 2017, 45, 1–11. [Google Scholar] [CrossRef] [PubMed]
- Melchels, F.P.W.; Domingos, M.A.N.; Klein, T.J.; Malda, J.; Bartolo, P.J.; Hutmacher, D.W. Additive Manufacturing of Tissues and Organs. Prog. Polym. Sci. 2012, 37, 1079–1104. [Google Scholar] [CrossRef]
- MacKay, S.M.; Funke, A.J.; Buffington, D.A.; Humes, H.D. Tissue Engineering of a Bioartificial Renal Tubule. ASAIO J. Am. Soc. Artif. Intern. Organs 1992 1998, 44, 179–183. [Google Scholar] [CrossRef]
- Cieslinski, D.A.; David Humes, H. Tissue Engineering of a Bioartificial Kidney. Biotechnol. Bioeng. 1994, 43, 678–681. [Google Scholar] [CrossRef]
- Ziogas, I.A.; Zein, N.N.; Quintini, C.; Miller, C.M.; Tsoulfas, G. Chapter 7—Three-Dimensional (3D) Printing and Liver Transplantation. In 3D Printing: Applications in Medicine and Surgery; Elsevier: Amsterdam, The Netherlands, 2020; pp. 97–116. [Google Scholar]
- Sun, Z.; Liu, D. A Systematic Review of Clinical Value of Three-Dimensional Printing in Renal Disease. Quant. Imaging Med. Surg. 2018, 8, 311–325. [Google Scholar] [CrossRef]
- Peired, A.J.; Mazzinghi, B.; De Chiara, L.; Guzzi, F.; Lasagni, L.; Romagnani, P.; Lazzeri, E. Bioengineering Strategies for Nephrologists: Kidney Was Not Built in a Day. Expert Opin. Biol. Ther. 2020, 20, 467–480. [Google Scholar] [CrossRef] [PubMed]
- Uwechue, R.; Gogalniceanu, P.; Kessaris, N.; Byrne, N.; Chandak, P.; Olsburgh, J.; Ahmed, K.; Mamode, N.; Loukopoulos, I. A Novel 3D-Printed Hybrid Simulation Model for Robotic-Assisted Kidney Transplantation (RAKT). J. Robot. Surg. 2018, 12, 541–544. [Google Scholar] [CrossRef] [PubMed]
- Claflin, J.; Waits, S.A. Three Dimensionally Printed Interactive Training Model for Kidney Transplantation. J. Surg. Educ. 2020, 77, 1013–1017. [Google Scholar] [CrossRef] [PubMed]
- Saba, P.; Belfast, E.; Melnyk, R.; Patel, A.; Kashyap, R.; Ghazi, A. Development of a High-Fidelity Robot-Assisted Kidney Transplant Simulation Platform Using Three-Dimensional Printing and Hydrogel Casting Technologies. J. Endourol. 2020, 34, 1088–1094. [Google Scholar] [CrossRef]
- Peri, A.; Marconi, S.; Gallo, V.; Mauri, V.; Negrello, E.; Abelli, M.; Ticozzelli, E.; Caserini, O.; Pugliese, L.; Auricchio, F.; et al. Three-D-Printed Simulator for Kidney Transplantation. Surg. Endosc. 2022, 36, 844–851. [Google Scholar] [CrossRef]
- Campi, R.; Pecoraro, A.; Vignolini, G.; Spatafora, P.; Sebastianelli, A.; Sessa, F.; Li Marzi, V.; Territo, A.; Decaestecker, K.; Breda, A.; et al. The First Entirely 3D-Printed Training Model for Robot-Assisted Kidney Transplantation: The RAKT Box. Eur. Urol. Open Sci. 2023, 53, 98–105. [Google Scholar] [CrossRef] [PubMed]
- Sweet, R.M. The CREST Simulation Development Process: Training the Next Generation. J. Endourol. 2017, 31, S69–S75. [Google Scholar] [CrossRef]
- Turney, B.W. A New Model with an Anatomically Accurate Human Renal Collecting System for Training in Fluoroscopy-Guided Percutaneous Nephrolithotomy Access. J. Endourol. 2014, 28, 360–363. [Google Scholar] [CrossRef]
- Adams, F.; Qiu, T.; Mark, A.; Fritz, B.; Kramer, L.; Schlager, D.; Wetterauer, U.; Miernik, A.; Fischer, P. Soft 3D-Printed Phantom of the Human Kidney with Collecting System. Ann. Biomed. Eng. 2017, 45, 963–972. [Google Scholar] [CrossRef]
- Tatar, İ.; Huri, E.; Selçuk, İ.; Moon, Y.L.; Paoluzzi, A.; Skolarikos, A. Review of the Effect of 3D Medical Printing and Virtual Reality on Urology Training with ‘MedTRain3DModsim’ Erasmus + European Union Project. Turk. J. Med. Sci. 2019, 49, 1257–1270. [Google Scholar] [CrossRef] [PubMed]
- Trelles Guzmán, C.R.; Mainez Rodríguez, J.A.; Aguado-Maestro, I.; Cansino Alcaide, R.; Pérez-Carral, J.R.; Martínez-Piñeiro, L. 3D Printed Model for Flexible Ureteroscopy Training, a Low-Cost Option for Surgical Training. Actas Urol. Esp. 2022, 46, 16–21. [Google Scholar] [CrossRef] [PubMed]
- Ho, T.P.; El-Sheikh, M.F.A.; Talbot, D. Case Report: Living Related Renal Transplantation with a Donor Kidney with Pelviureteric Junction Obstruction Using an Anderson-Hynes Pyeloplasty. Transplant. Proc. 2002, 34, 1193–1194. [Google Scholar] [CrossRef]
- Poniatowski, L.H.; Wolf Jr, J.S.; Nakada, S.Y.; Reihsen, T.E.; Sainfort, F.; Sweet, R.M. Validity and Acceptability of a High-Fidelity Physical Simulation Model for Training of Laparoscopic Pyeloplasty. J. Endourol. 2014, 28, 393–398. [Google Scholar] [CrossRef] [PubMed]
- Lemarteleur, V.; Peycelon, M.; Sablayrolles, J.-L.; Plaisance, P.; El-Ghoneimi, A.; Ceccaldi, P.-F. Realization of Open Software Chain for 3D Modeling and Printing of Organs in Simulation Centers: Example of Renal Pelvis Reconstruction. J. Surg. Educ. 2021, 78, 232–244. [Google Scholar] [CrossRef]
- Melnyk, R.; Ezzat, B.; Belfast, E.; Saba, P.; Farooq, S.; Campbell, T.; McAleavey, S.; Buckley, M.; Ghazi, A. Mechanical and Functional Validation of a Perfused, Robot-Assisted Partial Nephrectomy Simulation Platform Using a Combination of 3D Printing and Hydrogel Casting. World J. Urol. 2020, 38, 1631–1641. [Google Scholar] [CrossRef]
- Porpiglia, F.; Bertolo, R.; Checcucci, E.; Amparore, D.; Autorino, R.; Dasgupta, P.; Wiklund, P.; Tewari, A.; Liatsikos, E.; Fiori, C.; et al. Development and Validation of 3D Printed Virtual Models for Robot-Assisted Radical Prostatectomy and Partial Nephrectomy: Urologists’ and Patients’ Perception. World J. Urol. 2018, 36, 201–207. [Google Scholar] [CrossRef]
- Bernhard, J.-C.; Isotani, S.; Matsugasumi, T.; Duddalwar, V.; Hung, A.J.; Suer, E.; Baco, E.; Satkunasivam, R.; Djaladat, H.; Metcalfe, C.; et al. Personalized 3D Printed Model of Kidney and Tumor Anatomy: A Useful Tool for Patient Education. World J. Urol. 2016, 34, 337–345. [Google Scholar] [CrossRef]
- Kusaka, M.; Sugimoto, M.; Fukami, N.; Sasaki, H.; Takenaka, M.; Anraku, T.; Ito, T.; Kenmochi, T.; Shiroki, R.; Hoshinaga, K. Initial Experience with a Tailor-Made Simulation and Navigation Program Using a 3-D Printer Model of Kidney Transplantation Surgery. Transpl. Proc. 2015, 47, 596–599. [Google Scholar] [CrossRef]
- Chandak, P.; Byrne, N.; Coleman, A.; Karunanithy, N.; Carmichael, J.; Marks, S.D.; Stojanovic, J.; Kessaris, N.; Mamode, N. Patient-Specific 3D Printing: A Novel Technique for Complex Pediatric Renal Transplantation. Ann. Surg. 2019, 269, e18–e23. [Google Scholar] [CrossRef]
- Denizet, G.; Calame, P.; Lihoreau, T.; Kleinclauss, F.; Aubry, S. 3D Multi-Tissue Printing for Kidney Transplantation. Quant. Imaging Med. Surg. 2019, 9, 101–106. [Google Scholar] [CrossRef]
- Zhang, J.; Yan, H.; Xue, W.; Zheng, J.; Li, X.; Hao, L.; Guo, T.; Wang, Y.; Ding, X. 3D Printing Technology in Open Living Donor Nephrectomy. Chin. Med. J. 2022, 135, 2140–2141. [Google Scholar] [CrossRef]
- Cui, D.; Wu, B.; He, D.; Wang, Y.; Jiao, Y.; Zhang, B. 3D-Printed Cold Preservation Device in Renal Autotransplantation for the Treatment of a Patient with Renal Artery Stenosis. Front. Bioeng. Biotechnol. 2022, 9, 738434. [Google Scholar] [CrossRef]
- Weng, J.-Y.; Wang, C.-C.; Chen, P.-J.; Lim, S.-W.; Kuo, J.-R. The Application of a Three-Dimensional Printed Product to Fill the Space after Organ Removal. World Neurosurg. 2017, 107, 1045.e17–1045.e19. [Google Scholar] [CrossRef] [PubMed]
- Wu, X.; Jiang, C.; Wu, G.; Shen, C.; Fu, Q.; Chen, Y.; Liu, D.; Xue, W. Comparison of Three Dimensional Reconstruction and Conventional Computer Tomography Angiography in Patients Undergoing Zero-Ischemia Laparoscopic Partial Nephrectomy. BMC Med. Imaging 2020, 20, 47. [Google Scholar] [CrossRef] [PubMed]
- Skrzat, J.; Heryan, K.; Tarasiuk, J.; Wroński, S.; Proniewska, K.; Walecki, P.; Zarzecki, M.; Goncerz, G.; Walocha, J. A 3D Model of the Renal Vasculature—A Joined Result of the Corrosion Casting Technique, Micro-CT Imaging and Rapid Prototyping Technology. Folia Med. Cracov. 2021, 61, 45–54. [Google Scholar] [CrossRef] [PubMed]
- Checcucci, E.; De Cillis, S.; Porpiglia, F. 3D-Printed Models and Virtual Reality as New Tools for Image-Guided Robot-Assisted Nephron-Sparing Surgery: A Systematic Review of the Newest Evidences. Curr. Opin. Urol. 2020, 30, 55–64. [Google Scholar] [CrossRef]
- Fan, G.; Meng, Y.; Zhu, S.; Ye, M.; Li, M.; Li, F.; Ye, Y.; Liu, Z.; Weiqin, H.; Xie, Y. Three-Dimensional Printing for Laparoscopic Partial Nephrectomy in Patients with Renal Tumors. J. Int. Med. Res. 2019, 47, 4324–4332. [Google Scholar] [CrossRef]
- Girón-Vallejo, Ó.; García-Calderón, D.; Ruiz-Pruneda, R.; Cabello-Laureano, R.; Doménech-Abellán, E.; Fuster-Soler, J.L.; Ruiz-Jiménez, J.I. Three-Dimensional Printed Model of Bilateral Wilms Tumor: A Useful Tool for Planning Nephron Sparing Surgery. Pediatr. Blood Cancer 2018, 65, e26894. [Google Scholar] [CrossRef]
- Kyung, Y.S.; Kim, N.; Jeong, I.G.; Hong, J.H.; Kim, C.-S. Application of 3-D Printed Kidney Model in Partial Nephrectomy for Predicting Surgical Outcomes: A Feasibility Study. Clin. Genitourin. Cancer 2019, 17, e878–e884. [Google Scholar] [CrossRef]
- Wake, N.; Rude, T.; Kang, S.K.; Stifelman, M.D.; Borin, J.F.; Sodickson, D.K.; Huang, W.C.; Chandarana, H. 3D Printed Renal Cancer Models Derived from MRI Data: Application in Pre-Surgical Planning. Abdom. Radiol. 2017, 42, 1501–1509. [Google Scholar] [CrossRef]
- Cernat, E.; Docquier, P.-L.; Paul, L.; Banse, X.; Codorean, I.-B. Patient Specific Instruments for Complex Tumor Resection-Reconstruction Surgery within the Pelvis: A Series of 4 Cases. Chirurgia 2016, 111, 439–444. [Google Scholar] [CrossRef]
- Park, C.-J.; Kim, H.-W.; Jeong, S.; Seo, S.; Park, Y.; Moon, H.S.; Lee, J.-H. Anti-Reflux Ureteral Stent with Polymeric Flap Valve Using Three-Dimensional Printing: An in Vitro Study. J. Endourol. 2015, 29, 933–938. [Google Scholar] [CrossRef] [PubMed]
- Edgar, L.; Pu, T.; Porter, B.; Aziz, J.M.; La Pointe, C.; Asthana, A.; Orlando, G. Regenerative Medicine, Organ Bioengineering and Transplantation. Br. J. Surg. 2020, 107, 793–800. [Google Scholar] [CrossRef] [PubMed]
- Reske, A.; Metze, M. Complications of Immunosuppressive Agents Therapy in Transplant Patients. Minerva Anestesiol. 2014, 81, 1244–1261. [Google Scholar] [PubMed]
- Coulson, M.T.; Jablonski, P.; Howden, B.O.; Thomson, N.M.; Stein, A.N. Beyond Operational Tolerance: Effect of Ischemic Injury on Development of Chronic Damage in Renal Grafts. Transplantation 2005, 80, 353–361. [Google Scholar] [CrossRef]
- Wang, D.; Gust, M.; Ferrell, N. Kidney-on-a-Chip: Mechanical Stimulation and Sensor Integration. Sensors 2022, 22, 6889. [Google Scholar] [CrossRef]
- Yao, R.; Xu, G.; Mao, S.-S.; Yang, H.-Y.; Sang, X.-T.; Sun, W.; Mao, Y.-L. Three-Dimensional Printing: Review of Application in Medicine and Hepatic Surgery. Cancer Biol. Med. 2016, 13, 443–451. [Google Scholar] [CrossRef]
- Ravnic, D.J.; Leberfinger, A.N.; Koduru, S.V.; Hospodiuk, M.; Moncal, K.K.; Datta, P.; Dey, M.; Rizk, E.; Ozbolat, I.T. Transplantation of Bioprinted Tissues and Organs: Technical and Clinical Challenges and Future Perspectives. Ann. Surg. 2017, 266, 48–58. [Google Scholar] [CrossRef]
- Homan, K.A.; Kolesky, D.B.; Skylar-Scott, M.A.; Herrmann, J.; Obuobi, H.; Moisan, A.; Lewis, J.A. Bioprinting of 3D Convoluted Renal Proximal Tubules on Perfusable Chips. Sci. Rep. 2016, 6, 34845. [Google Scholar] [CrossRef]
- Lin, N.Y.C.; Homan, K.A.; Robinson, S.S.; Kolesky, D.B.; Duarte, N.; Moisan, A.; Lewis, J.A. Renal Reabsorption in 3D Vascularized Proximal Tubule Models. Proc. Natl. Acad. Sci. USA 2019, 116, 5399–5404. [Google Scholar] [CrossRef]
- King, S.M.; Higgins, J.W.; Nino, C.R.; Smith, T.R.; Paffenroth, E.H.; Fairbairn, C.E.; Docuyanan, A.; Shah, V.D.; Chen, A.E.; Presnell, S.C. 3D Proximal Tubule Tissues Recapitulate Key Aspects of Renal Physiology to Enable Nephrotoxicity Testing. Front. Physiol. 2017, 8, 123. [Google Scholar] [CrossRef]
- Ali, M.; Pr, A.K.; Yoo, J.J.; Zahran, F.; Atala, A.; Lee, S.J. A Photo-crosslinkable Kidney ECM-derived Bioink Accelerates Renal Tissue Formation. Adv. Healthc. Mater. 2019, 8, 1800992. [Google Scholar] [CrossRef] [PubMed]
- Addario, G.; Djudjaj, S.; Fare, S.; Boor, P.; Moroni, L.; Mota, C. Microfluidic Bioprinting towards a Renal in Vitro Model. Bioprinting 2020, 20, e00108. [Google Scholar] [CrossRef]
- Lawlor, K.T.; Vanslambrouck, J.M.; Higgins, J.W.; Chambon, A.; Bishard, K.; Arndt, D.; Er, P.X.; Wilson, S.B.; Howden, S.E.; Tan, K.S.; et al. Cellular Extrusion Bioprinting Improves Kidney Organoid Reproducibility and Conformation. Nat. Mater. 2021, 20, 260–271. [Google Scholar] [CrossRef] [PubMed]
- Jo, H.; Choi, B.Y.; Jang, G.; Lee, J.P.; Cho, A.; Kim, B.; Park, J.H.; Lee, J.; Kim, Y.H.; Ryu, J. Three-Dimensional Bio-Printed Autologous Omentum Patch Ameliorates Unilateral Ureteral Obstruction-Induced Renal Fibrosis. Tissue Eng. Part C Methods 2022, 28, 672–682. [Google Scholar] [CrossRef]
- Singh, N.K.; Han, W.; Nam, S.A.; Kim, J.W.; Kim, J.Y.; Kim, Y.K.; Cho, D.-W. Three-Dimensional Cell-Printing of Advanced Renal Tubular Tissue Analogue. Biomaterials 2020, 232, 119734. [Google Scholar] [CrossRef]
- Turunen, S.; Kaisto, S.; Skovorodkin, I.; Mironov, V.; Kalpio, T.; Vainio, S.; Rak-Raszewska, A. 3D Bioprinting of the Kidney—Hype or Hope? Cell Tissue Eng. 2018, 2, 119–162. [Google Scholar] [CrossRef]
- Hallman, M.A.; Zhuang, S.; Schnellmann, R.G. Regulation of Dedifferentiation and Redifferentiation in Renal Proximal Tubular Cells by the Epidermal Growth Factor Receptor. J. Pharmacol. Exp. Ther. 2008, 325, 520–528. [Google Scholar] [CrossRef]
- Lin, Z.; Will, Y. Evaluation of Drugs with Specific Organ Toxicities in Organ-Specific Cell Lines. Toxicol. Sci. 2012, 126, 114–127. [Google Scholar] [CrossRef] [PubMed]
- van den Berg, C.W.; Ritsma, L.; Avramut, M.C.; Wiersma, L.E.; van den Berg, B.M.; Leuning, D.G.; Lievers, E.; Koning, M.; Vanslambrouck, J.M.; Koster, A.J. Renal Subcapsular Transplantation of PSC-Derived Kidney Organoids Induces Neo-Vasculogenesis and Significant Glomerular and Tubular Maturation in Vivo. Stem Cell Rep. 2018, 10, 751–765. [Google Scholar] [CrossRef]
- Locatelli, F.; Buoncristiani, U.; Canaud, B.; Köhler, H.; Petitclerc, T.; Zucchelli, P. Dialysis Dose and Frequency. Nephrol. Dial. Transplant. 2005, 20, 285–296. [Google Scholar] [CrossRef] [PubMed]
- Thomas, M.; Rentsch, M.; Drefs, M.; Andrassy, J.; Meiser, B.; Stangl, M.; Jauch, K.-W.; Guba, M. Impact of Surgical Training and Surgeon’s Experience on Early Outcome in Kidney Transplantation. Langenbeck’s Arch. Surg. 2013, 398, 581–585. [Google Scholar] [CrossRef] [PubMed]
- Jurgaitis, J.; Paskonis, M.; Mehrabi, A.; Kashfi, A.; Gragert, S.; Hinz, U.; Schemmer, P.; Strupas, K.; Büchler, M.W.; Schmidt, J.; et al. Controlled-Surgical Education in Clinical Liver Transplantation Is Not Associated with Increased Patient Risks. Clin. Transplant. 2006, 20 (Suppl. S1), 69–74. [Google Scholar] [CrossRef]
- Ntakakis, G.; Plomariti, C.; Frantzidis, C.; Antoniou, P.E.; Bamidis, P.D.; Tsoulfas, G. Exploring the Use of Virtual Reality in Surgical Education. World J. Transplant. 2023, 13, 36–43. [Google Scholar] [CrossRef]
- Danila, R. Objective Evaluation of Minimally Invasive Surgical Skills for Transplantation Surgeons Using a Virtual Reality Simulator. Chirurgia 2009, 2. [Google Scholar]
- Wake, N.; Nussbaum, J.E.; Elias, M.I.; Nikas, C.V.; Bjurlin, M.A. 3D Printing, Augmented Reality, and Virtual Reality for the Assessment and Management of Kidney and Prostate Cancer: A Systematic Review. Urology 2020, 143, 20–32. [Google Scholar] [CrossRef]
- Ghazi, A. A Call for Change. Can 3D Printing Replace Cadavers for Surgical Training? Urol. Clin. N. Am. 2022, 49, 39–56. [Google Scholar] [CrossRef]
- Thurlow, J.S.; Joshi, M.; Yan, G.; Norris, K.C.; Agodoa, L.Y.; Yuan, C.M.; Nee, R. Global Epidemiology of End-Stage Kidney Disease and Disparities in Kidney Replacement Therapy. Am. J. Nephrol. 2021, 52, 98–107. [Google Scholar] [CrossRef]
- Davenport, A.; Gura, V.; Ronco, C.; Beizai, M.; Ezon, C.; Rambod, E. A Wearable Haemodialysis Device for Patients with End-Stage Renal Failure: A Pilot Study. Lancet 2007, 370, 2005–2010. [Google Scholar] [CrossRef] [PubMed]
- Gura, V.; Ronco, C.; Nalesso, F.; Brendolan, A.; Beizai, M.; Ezon, C.; Davenport, A.; Rambod, E. A Wearable Hemofilter for Continuous Ambulatory Ultrafiltration. Kidney Int. 2008, 73, 497–502. [Google Scholar] [CrossRef] [PubMed]
- Fissell, W.H.; Roy, S.; Davenport, A. Achieving More Frequent and Longer Dialysis for the Majority: Wearable Dialysis and Implantable Artificial Kidney Devices. Kidney Int. 2013, 84, 256–264. [Google Scholar] [CrossRef] [PubMed]
- Groth, T.; Stegmayr, B.G.; Ash, S.R.; Kuchinka, J.; Wieringa, F.P.; Fissell, W.H.; Roy, S. Wearable and Implantable Artificial Kidney Devices for End-stage Kidney Disease Treatment: Current Status and Review. Artif. Organs 2023, 47, 649–666. [Google Scholar] [CrossRef]
- Porrett, P.M.; Orandi, B.J.; Kumar, V.; Houp, J.; Anderson, D.; Cozette Killian, A.; Hauptfeld-Dolejsek, V.; Martin, D.E.; Macedon, S.; Budd, N. First Clinical-grade Porcine Kidney Xenotransplant Using a Human Decedent Model. Am. J. Transplant. 2022, 22, 1037–1053. [Google Scholar] [CrossRef]
- Montgomery, R.A.; Stern, J.M.; Lonze, B.E.; Tatapudi, V.S.; Mangiola, M.; Wu, M.; Weldon, E.; Lawson, N.; Deterville, C.; Dieter, R.A. Results of Two Cases of Pig-to-Human Kidney Xenotransplantation. N. Engl. J. Med. 2022, 386, 1889–1898. [Google Scholar] [CrossRef]
- Witowski, J.S.; Pędziwiatr, M.; Major, P.; Budzyński, A. Cost-Effective, Personalized, 3D-Printed Liver Model for Preoperative Planning before Laparoscopic Liver Hemihepatectomy for Colorectal Cancer Metastases. Int. J. Comput. Assist. Radiol. Surg. 2017, 12, 2047–2054. [Google Scholar] [CrossRef]
| First Author | Imaging Modality | Printer Type/Employed Materials | Number of 3D-Printed Models | Printing Time | Cost (per Model) | Aim | |
|---|---|---|---|---|---|---|---|
| 1. | Uwechue R. [16] | Abdominal and pelvic CT imaging | NR | Two (donor and recipient) | NR | GBP 1000 | Two robotic surgeons performed vascular anastomoses between the donor’s and recipient’s iliac vessels. |
| 2. | Claflin J. [17] | Abdominal and pelvic CT imaging | PrintrBot (©PrintrBot, Lincoln, California)/Polylactic acid filament | One | NR | USD 178 | Residents were trained to perform end-to-side arterial and vein anastomoses with the instruction of an attending transplant surgeon. |
| 3. | Saba P. [18] | Abdominal and pelvic CT imaging | Fusion3 F400-S (©Fusion3 Design, Greensboro, NC)/PVA hydrogel mixture | Two (donor and recipient) | NR | USD 95 worth of materials | A certified transplant surgeon completed a robotic training curriculum, including four RAKT simulation procedures |
| 4. | Peri A. [19] | Abdominal and pelvic CT and MRI imaging | Objet260 Connex 3 (©Stratasys, Eden Prairie, MN, USA)/Combination of rigid and deformable materials (photo-rather polymeric resins) | 35 (five pilot models) | 15 h for each procedure | EUR 2665 for the fixed platform plus EUR 220 for each procedure | Two surgical trainees completed a series of 15 simulation transplantations each while their anastomotic time was recorded, and three experts visually rated anastomotic quality. |
| 5. | Campi R. [20] | Abdominal and pelvic CT imaging | FDM printer/Combination of poly(lactic acid), silicon elastomer, and soft materials | One box | NR | EUR 5000 for the box and EUR 100 for disposable vessels | Four surgical trainees performed training sessions with the RAKT box, performing vascular anastomoses between the graft’s renal and recipient’s iliac vessels. |
| First Author | Imaging Modality | Printer Type/Employed Materials | Number of 3D-Printed Models | Printing Time | Cost (per Model) | Aim | |
|---|---|---|---|---|---|---|---|
| 1. | Kusaka M. [32] | Abdominal and pelvic CT imaging | Objet500 Connex 3 (©Stratasys, Eden Prairie, MN, USA)/VeroClear, VeroMagenta, VeroCyan, TangoPlus | Two graft models and one recipient model | NR | NR | Surgeons performed preoperatively vascular anastomoses in patient-specific models and discussed the results with the transplant team. |
| 2. | Chandak P. [33] | Abdominal and pelvic CT and MRI imaging | Objet500 Connex1 (©Objet-Stratasys, Rehovot, Israel)/Acrylic photopolymers | Three | 9 h | USD 1500 per case | Preoperative planning and decision-making (regarding feasibility) in three complex pediatric renal transplantation cases |
| 3. | Denizet G. [34] | Abdominal and pelvic CT without contrast | Multi-jet printer (©Scalia, Cryla Group, Besancon, France)/Elastomeric resin and acrylonitrile butadiene styrene | Four | 10–14 h | EUR 300–400 | Assess the feasibility of the anastomosis at various potential sites of anastomosis by palpation—simulation of clamping. |
| 4. | Zhang J. [35] | CT angiography and CT urography | NR/Photoreceptor resin | 60 | 4–6 h | NR | Assist preoperative planning, including assessing vascular variations, performing simulations of the planned operation, and deciding on the surgical site of living donor renal transplantations. |
| 5. | Cui D. [36] | Abdominal and pelvic CT imaging | ©Shanghai liantai Technology Co., Ltd. rs4500 China/PLA filament | One | 8 h | NR | Development of a 3D-printed cold preservation device that makes feasible the laparoscopic intracorporeal renal autotransplantation |
| 6. | Weng JY. [37] | Use of a standard template | FreeDMake (©Blooming Electronics Co Ltd., Taiwan)Polylactic acid | Four | 6 h 35 min | USD 4 per hour printing | Maintain body integrity following organ retrieval as psychological support to the family. Alter the stance toward transplantation from a deceased donor. |
| First Author | Cell Lines-Subjects | Printer Type/Bioink | Printing Strategy | Aim | Results | |
|---|---|---|---|---|---|---|
| 1. | Homan KA. [53] | PTEC | AGB 10000, (©Aerotech Inc., Pittsburgh, PA, USA)/gelatin-fibrin hydrogel, fugitive ink, silicone elastomer | Scaffold based | Develop 3D convoluted renal proximal tubules within microfluidic chips | The microfluidic-based model showed high cell viability, gene expression pattern close to primary renal PTEC, and superior functional albumin uptake compared with 2D controls |
| 2. | Lin NYC. [54] | PTEC, vascular endothelial cells | 3D-Bioplotter (©EnvisionTEC)/gelatin-fibrin-based ECM, fugitive ink | Scaffold based | Vascularized proximal tubules (microfluidic platform) demonstrating reabsorption of solutes (tubular-vascular exchange) | The model demonstrated active albumin and glucose reabsorption. |
| 3. | King MS [55] | HUVEC, adult, renal, fibroblast, and renal PTEC | NovoGen Bioprinter Instrument (©Organovo Inc., San Diego, CA, USA)/NovoGel Bio-Ink | Scaffold based | Develop a renal proximal tubule model in vitro supported by renal fibroblast and endothelial cells. | The model demonstrated functions of the native proximal tubule, drug-induced nephrotoxicity, and renal fibrosis. |
| 4. | Ali M. [56] | Porcine kidneys/human primary kidney cells | ITOP system/KdECMMA-based | Scaffold based | Investigate the role of KdECMMA-based bio-ink in supporting 3D bioprinted renal constructs from human primary kidney cells | The constructs demonstrated high cell viability, and significantly higher sodium reabsorption and hydrolase activity compared to the control group. |
| 5. | Addario G. [57] | pmTEC, HUVEC fibroblasts | Microfluidic bioprinter (©RX1 Aspect Biosystems, Canada)/alginate, gelatin, pectin | Scaffold based | Development of a microfluidic-based tubulointerstitium model for in-vitro studies | The authors achieved to develop multiple models of different cell-line/bio-ink formulations comparing the cell viability and metabolic activity of the various constructs |
| 6. | Lawlor KT. [58] | hPSCs | NovoGen MMX extrusion-based 3D cellular bioprinter (©Organovo Inc., San Diego, CA, USA)/Cellular Bio-Ink. | Scaffold free | Develop renal organoids of highly reproducible cell number and viability by extrusion-based 3D cellular bioprinting. | Achieved the formation of renal organoids demonstrating a high resemblance to nephron histology, high reproducibility/cell viability, and drug-induced nephrotoxicity |
| 7. | Jo H. [59] | Autologous omentum tissue/UUO Rats | Dr. INVIVO (©ROKIT Healthcare, Inc., Seoul, Korea)/fibrinogen, thrombin | Scaffold free | Transplantation of an autologous omentum patch in the renal subcapsular space for immune regulation and tissue regeneration | Reduced tubular injury and downregulation of fibrosis-inducing mechanisms were observed in the omentum patch group. |
| 8. | Singh NK. [60] | Porcine kidneys, hBMMSC, renal PTEC, and HUVEC, UUO mice | In-house developed 3D cell-printing system/decellularized ECMs, alginate, pluronic | Scaffold based | Develop a 3D microfluidic vascularized renal tubular tissue-on-a-chip. Transplant grafts in UUO mice | Perfusable tubular constructs were developed with the ability to switch between monolayer and bilayer. Markers of tissue maturation were observed regarding renal tubular tissue and vascular tissue. UUO |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Christou, C.D.; Vasileiadou, S.; Sotiroudis, G.; Tsoulfas, G. Three-Dimensional Printing and Bioprinting in Renal Transplantation and Regenerative Medicine: Current Perspectives. J. Clin. Med. 2023, 12, 6520. https://doi.org/10.3390/jcm12206520
Christou CD, Vasileiadou S, Sotiroudis G, Tsoulfas G. Three-Dimensional Printing and Bioprinting in Renal Transplantation and Regenerative Medicine: Current Perspectives. Journal of Clinical Medicine. 2023; 12(20):6520. https://doi.org/10.3390/jcm12206520
Chicago/Turabian StyleChristou, Chrysanthos D., Stella Vasileiadou, Georgios Sotiroudis, and Georgios Tsoulfas. 2023. "Three-Dimensional Printing and Bioprinting in Renal Transplantation and Regenerative Medicine: Current Perspectives" Journal of Clinical Medicine 12, no. 20: 6520. https://doi.org/10.3390/jcm12206520
APA StyleChristou, C. D., Vasileiadou, S., Sotiroudis, G., & Tsoulfas, G. (2023). Three-Dimensional Printing and Bioprinting in Renal Transplantation and Regenerative Medicine: Current Perspectives. Journal of Clinical Medicine, 12(20), 6520. https://doi.org/10.3390/jcm12206520