Immunosuppressive Therapy and Nutritional Status of Patients after Kidney Transplantation: A Protocol for a Systematic Review
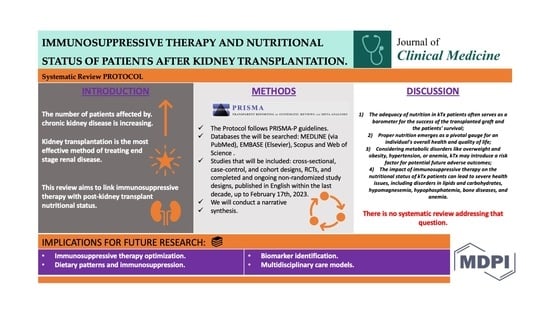
Abstract
:1. Introduction
2. Materials and Methods
2.1. Protocol and Registration
2.2. Eligibility Criteria
2.2.1. Types of Participants
2.2.2. Exposure(s)
2.2.3. Outcomes(s)
2.3. Information Sources
2.4. Search Strategy
2.5. Study Selection
2.6. Data Extraction
2.7. Quality Assessment
2.8. Data Analysis
3. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Acknowledgments
Conflicts of Interest
Abbreviations
| BIA | bioimpedance analysis |
| BMI | body mass index |
| CKD | chronic kidney disease |
| CMV | cytomegalovirus |
| CNIs | calcineurin inhibitors |
| CsA | cyclosporine A |
| EBV | Epstein-Barr virus |
| ESRD | end-stage renal disease |
| kTx | kidney transplantation |
| mTOR | mammalian target of rapamycin |
| PTDM | post-transplant diabetes mellitus |
| PRISMA | Preferred Reporting Items for Systematic Reviews and Meta-Analyses |
| PRISMA-P | Preferred Reporting Items for Systematic Reviews and Meta-Analyses Protocols |
| PROSPERO | International Prospective Register for Systematic Reviews |
| RCTs | randomized controlled trials |
| RevMan | Review Manager |
| RoB2 | the Cochrane Risk of Bias tool |
| Tac | tacrolimus |
References
- World Health Organization. Transplantation. 2023. Available online: https://www.who.int/health-topics/transplantation#tab=tab_1 (accessed on 6 October 2023).
- World Health Organization. Human Organ and Tissue Transplantation. Report. 2022. Available online: https://apps.who.int/gb/ebwha/pdf_files/WHA75/A75_41-en.pdf (accessed on 6 October 2023).
- Durlik, M.; Przybyłowski, P.; Bączkowska, T. Zalecenia Dotyczące Leczenia Immunosupresyjnego Po Przeszczepieniu Narządów Unaczynionych; Fundacja Zjednoczeni dla Transplantacji: Warszawa, Poland, 2021. [Google Scholar]
- Europe PMC; Abramyan, S.; Matthew, H. Kidney Transplantation, Europe PMC. 2023. Available online: https://europepmc.org/article/nbk/nbk567755#free-full-text (accessed on 29 August 2023).
- Elflein, J. Organ Transplant Statistics Worldwide 2021, Statista. 2023. Available online: https://www.statista.com/statistics/398645/global-estimation-of-organ-transplantations/ (accessed on 29 August 2023).
- WHO-ONT. Global Observatory on Donation and Transplantation. GODT. 2023. Available online: https://www.transplant-observatory.org/ (accessed on 6 October 2023).
- Kompendium dla Chorych i ich Rodzin Oraz Personelu Medycznego. 2019. Available online: https://zgodanazycie.pl/wp-content/uploads/2019/06/Kompendium_Transplantacja_nerki_www.pdf (accessed on 29 August 2023).
- Daugirdas, J.T.; Rocco, M.V.; Depner, T.A.; Inrig, J.; Mehrotra, R.; Suri, R.S.; Weiner, D.E.; Greer, N.; Ishani, A.; MacDonald, R.; et al. KDOQI clinical practice guideline for hemodialysis adequacy: 2015 update. Am. J. Kidney Dis. 2015, 66, 884–930. [Google Scholar] [CrossRef] [PubMed]
- Mudiayi, D.; Shojai, S.; Okpechi, I.; Christie, E.A.; Wen, K.; Kamaleldin, M.; Osman, M.E.; Lunney, M.M.; Prasad, B.; Ye, F.M.; et al. Global estimates of capacity for kidney transplantation in world countries and regions. Transplantation 2022, 106, 1113–1122. [Google Scholar] [CrossRef] [PubMed]
- Al-Adra, D.; Al-Qaoud, T.; Fowler, K.; Wong, G. De novo malignancies after kidney transplantation. Clin. J. Am. Soc. Nephrol. 2022, 17, 434–443. [Google Scholar] [CrossRef] [PubMed]
- Agrawal, A.; Ison, M.G.; Danziger-Isakov, L. Long-term infectious complications of kidney transplantation. Clin. J. Am. Soc. Nephrol. 2022, 17, 286–295. [Google Scholar] [CrossRef]
- Gupta, K.; Bagai, S.; Ramachandran, R.; Kumar, V.; Rathi, M.; Kohli, H.S.; Sharma, A.; Chakrabarti, A. Fungal infection in post-renal transplant patient: Single-center experience. Indian J. Pathol. Microbiol. 2020, 63, 587. [Google Scholar] [CrossRef]
- Małgorzewicz, S.; Ciechanowski, K.; Kozłowska, L. Principles of nutrition in chronic kidney disease—Position of the Working Group of the Polish Society of Nephrology. Nephrol. Forum 2019, 12, 240–278. [Google Scholar]
- Favi, E.; Molinari, P.; Alfieri, C.; Castellano, G.; Ferraresso, M.; Cresseri, D. Case report: Eculizumab Plus obinutuzumab induction in a deceased donor kidney transplant recipient with DEAP-hus. Front. Immunol. 2022, 13, 1073808. [Google Scholar] [CrossRef]
- Szumilas, K.; Wilk, A.; Wiśniewski, P.; Gimpel, A.; Dziedziejko, V.; Kipp, M.; Pawlik, A. Current status regarding immunosuppressive treatment in patients after renal transplantation. Int. J. Mol. Sci. 2023, 24, 10301. [Google Scholar] [CrossRef]
- Bauer, A.C.; Franco, R.F.; Manfro, R.C. Immunosuppression in kidney transplantation: State of the art and current protocols. Curr. Pharm. Des. 2020, 26, 3440–3450. [Google Scholar] [CrossRef]
- Bentata, Y. Tacrolimus: 20 years of use in adult kidney transplantation. what we should know about its nephrotoxicity. Artif. Organs 2019, 44, 140–152. [Google Scholar] [CrossRef] [PubMed]
- Yu, M.; Liu, M.; Zhang, W.; Ming, Y. Pharmacokinetics, pharmacodynamics and pharmacogenetics of Tacrolimus in kidney transplantation. Curr. Drug Metab. 2018, 19, 513–522. [Google Scholar] [CrossRef]
- Kajiwara, M.; Masuda, S. Role of mtor inhibitors in kidney disease. Int. J. Mol. Sci. 2016, 17, 975. [Google Scholar] [CrossRef] [PubMed]
- Meneghini, M.; Bestard, O.; Grinyo, J.M. Immunosuppressive drugs modes of action. Best Pract. Res. Clin. Gastroenterol. 2021, 54–55, 101757. [Google Scholar] [CrossRef] [PubMed]
- Sandal, S.; Bae, S.; McAdams-DeMarco, M.; Massie, A.B.; Lentine, K.L.; Cantarovich, M.; Segev, D.L. Induction immunosuppression agents as risk factors for incident cardiovascular events and mortality after kidney transplantation. Am. J. Transplant. 2019, 19, 1150–1159. [Google Scholar] [CrossRef]
- Wagner, S.J.; Brennan, D.C. Induction therapy in renal transplant recipients. Drugs 2012, 72, 671–683. [Google Scholar] [CrossRef]
- Parlakpinar, H.; Gunata, M. Transplantation and immunosuppression: A review of novel transplant-related Immunosuppressant Drugs. Immunopharmacol. Immunotoxicol. 2021, 43, 651–665. [Google Scholar] [CrossRef] [PubMed]
- Tambur, A.R.; Campbell, P.; Chong, A.S.; Feng, S.; Ford, M.L.; Gebel, H.; Gill, R.G.; Kelsoe, G.; Kosmoliaptsis, V.; Mannon, R.B.; et al. Sensitization in transplantation: Assessment of risk (STAR) 2019 Working Group Meeting Report. Am. J. Transplant. 2020, 20, 2652–2668. [Google Scholar] [CrossRef]
- Farouk, S.S.; Rein, J.L. The many faces of calcineurin inhibitor toxicity—What the FK? Adv. Chronic Kidney Dis. 2020, 27, 56–66. [Google Scholar] [CrossRef]
- Flechner, S.M. MTOR inhibition and clinical transplantation. Transplantation 2018, 102, S17–S18. [Google Scholar] [CrossRef]
- Reggiani, F.; Moroni, G.; Ponticelli, C. Cardiovascular risk after kidney transplantation: Causes and current approaches to a relevant burden. J. Pers. Med. 2022, 12, 1200. [Google Scholar] [CrossRef]
- Zarifi, S.H.; Shadnoush, M.; Pahlavani, N.; Malekahmadi, M.; Firouzi, S.; Sabbagh, M.G.; Rezaiyan, M.K.; Islam, S.M.S.; Yahyapoor, F.; Arabi, S.M.; et al. Nutritional status in kidney transplant patients before and 6-month after transplantation: Result of PNSI study. Clin. Nutr. ESPEN 2021, 41, 268–274. [Google Scholar] [CrossRef]
- Górska, M.; Kurnatowska, I. Nutrition Disturbances and Metabolic Complications in Kidney Transplant Recipients: Etiology, Methods of Assessment and Prevention—A Review. Nutrients 2022, 14, 4996. [Google Scholar] [CrossRef]
- Saxena, A.; Sharma, R.K.; Gupta, A. Graft function and nutritional parameters in stable post renal transplant patients. Clin. Queries: Nephrol. 2013, 2, 141–144. [Google Scholar] [CrossRef]
- Baker, J.P.; Detsky, A.S.; Wesson, D.E.; Wolman, S.L.; Stewart, S.; Whitewell, J.; Langer, B.; Jeejeebhoy, K.N. Nutritional assessment. N. Engl. J. Med. 1982, 306, 969–972. [Google Scholar] [CrossRef] [PubMed]
- Jeejeebhoy, K.N.; Detsky, A.S.; Baker, J.P. Assessment of Nutritional Status. J. Parenter. Enter. Nutr. 1990, 14, 193–196. [Google Scholar] [CrossRef]
- Pontes, K.S.; Klein, M.R.S.T.; da Costa, M.S.; Rosina, K.T.d.C.; Barreto, A.P.M.M.; Silva, M.I.B.; Rioja, S.d.S. Vitamin B12 status in kidney transplant recipients: Association with dietary intake, body adiposity and immunosuppression. Br. J. Nutr. 2019, 122, 450–458. [Google Scholar] [CrossRef] [PubMed]
- Perrea, D.N.; Moulakakis, K.G.; Poulakou, M.V.; Vlachos, I.S.; Nikiteas, N.; Kostakis, A. Correlation between lipid abnormalities and immunosuppressive therapy in renal transplant recipients with stable renal function. Int. Urol. Nephrol. 2007, 40, 521–527. [Google Scholar] [CrossRef] [PubMed]
- Małgorzewicz, S.; Wołoszyk, P.; Chamienia, A.; Jankowska, M.; Dębska-Ślizień, A. Obesity risk factors in patients after kidney transplantation. Transplant. Proc. 2018, 50, 1786–1789. [Google Scholar] [CrossRef] [PubMed]
- Khalili, N.; Rostami, Z.; Kalantar, E.; Einollahi, B. Hyperglycemia after renal transplantation: Frequency and risk factors. Nephro-Urol. Mon. 2013, 5, 753–757. [Google Scholar] [CrossRef] [PubMed]
- Schechter, A.; Gafter-Gvili, A.; Shepshelovich, D.; Rahamimov, R.; Gafter, U.; Mor, E.; Chagnac, A.; Rozen-Zvi, B. Post renal transplant anemia: Severity, causes and their association with graft and patient survival. BMC Nephrol. 2019, 20, 51. [Google Scholar] [CrossRef]
- Douwes, R.M.; Gomes-Neto, A.W.; Eisenga, M.F.; Vinke, J.S.J.; de Borst, M.H.; van den Berg, E.; Berger, S.P.; Touw, D.J.; Hak, E.; Blokzijl, H.; et al. Chronic use of Proton-pump inhibitors and iron status in renal transplant recipients. J. Clin. Med. 2019, 8, 1382. [Google Scholar] [CrossRef] [PubMed]
- Baxmann, A.C.; Menon, V.B.; Medina-Pestana, J.O.; Carvalho, A.B.; Heilberg, I.P. Overweight and body fat are predictors of hypovitaminosis D in renal transplant patients. Clin. Kidney J. 2015, 8, 49–53. [Google Scholar] [CrossRef] [PubMed]
- Zeng, S.; Yang, Y.; Li, S.; Hocher, C.F.; Chu, C.; Wang, Z.; Zheng, Z.; Krämer, B.K.; Hocher, B. 25(OH)D-but not 1,25(OH)2D–Is an independent risk factor predicting graft loss in stable kidney transplant recipients. Front. Med. 2023, 10, 1141646. [Google Scholar] [CrossRef] [PubMed]
- Eyal, O.; Aharon, M.; Safadi, R.; Elhalel, M.D. Serum vitamin D levels in kidney transplant recipients: The importance of an immunosuppression regimen and sun exposure. Isr. Med. Assoc. J. 2013, 15, 628–633. [Google Scholar] [PubMed]
- Filipov, J.J.; Zlatkov, B.K.; Dimitrov, E.P.; Svinarov, D. Relationship between vitamin D status and immunosuppressive therapy in kidney transplant recipients. Biotechnol. Biotechnol. Equip. 2015, 29, 331–335. [Google Scholar] [CrossRef]
- Bouquegneau, A.; Salam, S.; Delanaye, P.; Eastell, R.; Khwaja, A. Bone Disease after Kidney Transplantation. Clin. J. Am. Soc. Nephrol. 2016, 11, 1282–1296. [Google Scholar] [CrossRef]
- Malluche, H.H.; Monier-Faugere, M.-C.; Herberth, J. Bone disease after Renal Transplantation. Nat. Rev. Nephrol. 2009, 6, 32–40. [Google Scholar] [CrossRef] [PubMed]
- Brandenburg, V.M.; Salam, S.; Delanaye, P.; Eastell, R.; Khwaja, A. Early rapid loss followed by long-term consolidation characterizes the development of lumbar bone mineral density after kidney transplantation. Transplantation 2004, 77, 1566–1571. [Google Scholar] [CrossRef]
- Iyer, S.P.; Nikkel, L.E.; Nishiyama, K.K.; Dworakowski, E.; Cremers, S.; Zhang, C.; McMahon, D.J.; Boutroy, S.; Liu, X.S.; Ratner, L.E.; et al. Kidney transplantation with early corticosteroid withdrawal. J. Am. Soc. Nephrol. 2014, 25, 1331–1341. [Google Scholar] [CrossRef]
- Culliford, A.; Phagura, N.; Sharif, A. Autosomal dominant polycystic kidney disease is a risk factor for posttransplantation diabetes mellitus: An updated systematic review and meta-analysis. Transplant. Direct 2020, 6, e553. [Google Scholar] [CrossRef] [PubMed]
- Penfornis, A.; Kury-Paulin, S. Immunosuppressive drug-induced diabetes. Diabetes Metab. 2006, 32, 539–546. [Google Scholar] [CrossRef] [PubMed]
- Martin-Moreno, P.L.; Shin, H.-S.; Chandraker, A. Obesity and post-transplant diabetes mellitus in kidney transplantation. J. Clin. Med. 2021, 10, 2497. [Google Scholar] [CrossRef]
- Sanyal, D.; Bhattacharjee, K.; Das, P. A new scoring system to predict the incidence of new onset diabetes after transplantation (NODAT). Clin. Diabetol. 2020, 9, 226–232. [Google Scholar] [CrossRef]
- Osté, M.C.J.; Corpeleijn, E.; Navis, G.J.; Keyzer, C.A.; Soedamah-Muthu, S.S.; Van Den Berg, E.; Postmus, D.; De Borst, M.H.; Kromhout, D.; Bakker, S.J.L. Mediterranean style diet is associated with low risk of new-onset diabetes after renal transplantation. BMJ Open Diabetes Res. Care 2017, 5, e000283. [Google Scholar] [CrossRef] [PubMed]
- Morales Febles, R.; Miranda, D.M.; Sosa, A.J.; Rinne, A.G.; Perera, C.C.; Rodríguez-Rodríguez, A.E.; González, A.; Martín, L.D.; Mena, N.N.; Sørensen, C.A.; et al. Exercise and Prediabetes after renal transplantation (EXPRED-I): A prospective study. Sports Med.-Open 2023, 9, 32. [Google Scholar] [CrossRef]
- Skulratanasak, P.; Larpparisuth, N. Lipid management to mitigate poorer postkidney transplant outcomes. Curr. Opin. Nephrol. Hypertens. 2022, 32, 27–34. [Google Scholar] [CrossRef]
- Durlik, M. Hypertension in solid organ transplant recipients. Ann. Transplant. 2012, 17, 100–107. [Google Scholar] [CrossRef]
- Dedinská, I.; Miklušica, J.; Palkoci, B.; Galajda, P.; Mokán, M. Body mass index before kidney transplantation—Principal risk factor for NODAT. Clin. Diabetol. 2016, 5, 1–6. [Google Scholar] [CrossRef]
- Wołoszyk, P.; Małgorzewicz, S.; Chamienia, A.; Dębska-Ślizień, A. Obesity after successful kidney transplantation. Transplant. Proc. 2020, 52, 2352–2356. [Google Scholar] [CrossRef]
- Ruangkanchanasetr, P.; Satirapoj, B.; Bunnag, S.; Vongwiwatana, A.; Premasathian, N.; Avihingsanon, Y. High prevalence of obesity in Thai renal transplant recipients: A multicenter study. Transplant. Proc. 2014, 46, 546–551. [Google Scholar] [CrossRef]
- Stefanelli, L.F.; Alessi, M.; Bertoldi, G.; Rossato, V.; Di Vico, V.; Nalesso, F.; Calò, L.A. Calcineurin-Inhibitor-Induced Hypomagnesemia in Kidney Transplant Patients: A Monocentric Comparative Study between Sucrosomial Magnesium and Magnesium Pidolate Supplementation. J. Clin. Med. 2023, 12, 752. [Google Scholar] [CrossRef]
- Jankowska, M.; Trzonkowski, P.; Dębska-Ślizień, A.; Marszał, M.; Rutkowski, B. Vitamin B6 status, immune response and inflammation markers in kidney transplant recipients treated with polyclonal anti-thymocyte globulin. Transplant. Proc. 2014, 46, 2631–2635. [Google Scholar] [CrossRef] [PubMed]
- Netto, M.C.A.S.; Alves-Filho, G.; Mazzali, M. Nutritional status and body composition in patients early after renal transplantation. Transplant. Proc. 2012, 44, 2366–2368. [Google Scholar] [CrossRef] [PubMed]
- Shamseer, L.; Moher, D.; Clarke, M.; Ghersi, D.; Liberati, A.; Petticrew, M.; Shekelle, P.; Stewart, L.; PRISMA-P Group. Preferred reporting items for systematic review and meta-analysis protocols (PRISMA-P) 2015: Elaboration and explanation. BMJ 2015, 349, g7647. [Google Scholar] [CrossRef] [PubMed]
- Kajdas, A.; Szostak-Węgierek, D.; Dąbrowska-Bender, M.; Normann, A.K.; Søndergaard Linde, D. Immunosuppressive Therapy and Nutritional Status of Patients after Kidney Transplantation—A Systematic Review, Prospero. 2023. Available online: https://www.crd.york.ac.uk/prospero/display_record.php?RecordID=396773 (accessed on 29 August 2023).
- Page, M.J.; McKenzie, J.E.; Bossuyt, P.M.; Boutron, I.; Hoffmann, T.C.; Mulrow, C.D.; Shamseer, L.; Tetzlaff, J.M.; Akl, E.A.; Brennan, S.E.; et al. The Prisma 2020 statement: An updated guideline for reporting systematic reviews. BMJ 2021, 372, 71. [Google Scholar] [CrossRef]
- Better Systematic Review Management. Covidence. 2023. Available online: https://www.covidence.org/ (accessed on 29 August 2023).
- Higgins, J.P.; Altman, D.G.; Gøtzsche, P.C.; Jüni, P.; Moher, D.; Oxman, A.D.; Savović, J.; Schulz, K.F.; Weeks, L.; Sterne, J.A.C.; et al. The Cochrane Collaboration’s tool for assessing risk of bias in randomised trials. BMJ 2011, 343, d5928. [Google Scholar] [CrossRef]
- Revman Web. 2022. Available online: https://revman.cochrane.org/#/myReviews (accessed on 29 August 2023).
- Sterne, J.A.C.; Hernan, M.A.; Reeves, B.C.; Savović, J.; Berkman, N.D.; Viswanathan, M.; Henry, D.; Altman, D.G.; Ansari, M.T.; Boutron, I.; et al. ROBINS-I: A tool for assessing risk of bias in non-randomised studies of interventions. BMJ Br. Med. J. 2016, 355, i4919. [Google Scholar] [CrossRef]
- McGuinness, L.A.; Higgins, J.P.T. Risk-of-bias visualization (robvis): An R package and Shiny web app for visualizing risk-of-bias assessments. Res. Synth. Methods 2021, 12, 55–61. [Google Scholar] [CrossRef]
- Chapter 12: Synthesizing and Presenting Findings Using Other Methods|Cochrane Training. 2023. Available online: https://training.cochrane.org/handbook/current/chapter-12 (accessed on 29 August 2023).

Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kajdas, A.A.; Szostak-Węgierek, D.; Dąbrowska-Bender, M.; Normann, A.K.; Søndergaard Linde, D. Immunosuppressive Therapy and Nutritional Status of Patients after Kidney Transplantation: A Protocol for a Systematic Review. J. Clin. Med. 2023, 12, 6955. https://doi.org/10.3390/jcm12216955
Kajdas AA, Szostak-Węgierek D, Dąbrowska-Bender M, Normann AK, Søndergaard Linde D. Immunosuppressive Therapy and Nutritional Status of Patients after Kidney Transplantation: A Protocol for a Systematic Review. Journal of Clinical Medicine. 2023; 12(21):6955. https://doi.org/10.3390/jcm12216955
Chicago/Turabian StyleKajdas, Aleksandra Anna, Dorota Szostak-Węgierek, Marta Dąbrowska-Bender, Anne Katrine Normann, and Ditte Søndergaard Linde. 2023. "Immunosuppressive Therapy and Nutritional Status of Patients after Kidney Transplantation: A Protocol for a Systematic Review" Journal of Clinical Medicine 12, no. 21: 6955. https://doi.org/10.3390/jcm12216955
APA StyleKajdas, A. A., Szostak-Węgierek, D., Dąbrowska-Bender, M., Normann, A. K., & Søndergaard Linde, D. (2023). Immunosuppressive Therapy and Nutritional Status of Patients after Kidney Transplantation: A Protocol for a Systematic Review. Journal of Clinical Medicine, 12(21), 6955. https://doi.org/10.3390/jcm12216955