Diagnostic Utility of a Combined MPO/D-Dimer Score to Distinguish Abdominal Aortic Aneurysm from Peripheral Artery Disease
Abstract
:1. Introduction
2. Methods
2.1. Study Design
2.2. Analysis of Blood Parameters
2.3. Statistical Analysis
3. Results
3.1. Patient Cohorts Show Comparable Demographics and Co-Morbidities While Healthy Controls Differ Significantly
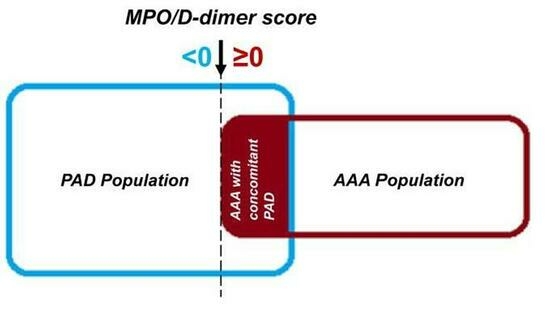
3.2. The Combined Score Is Superior to Single-Parameter Analysis in Discriminating AAA from PAD Patients
3.3. The Score Prevails as an Independent Diagnostic Parameter for AAA
4. Discussion
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Sakalihasan, N.; Michel, J.B.; Katsargyris, A.; Kuivaniemi, H.; Defraigne, J.O.; Nchimi, A.; Powell, J.T.; Yoshimura, K.; Hultgren, R. Abdominal aortic aneurysms. Nat. Rev. Dis. Primers 2018, 4, 34. [Google Scholar] [CrossRef]
- Anjorin, A.C.; Greiner, M.A.; Vemulapalli, S.; Svetkey, L.; Southerland, K.W.; Bosworth, H.B. Underutilization of Guideline-based Abdominal Aortic Aneurysm Screening in an Academic Health System. Ann. Vasc. Surg. 2022, 83, 184–194. [Google Scholar] [CrossRef]
- Force, U.S.P.S.T.; Owens, D.K.; Davidson, K.W.; Krist, A.H.; Barry, M.J.; Cabana, M.; Caughey, A.B.; Doubeni, C.A.; Epling, J.W., Jr.; Kubik, M.; et al. Screening for Abdominal Aortic Aneurysm: US Preventive Services Task Force Recommendation Statement. JAMA 2019, 322, 2211–2218. [Google Scholar] [CrossRef]
- Norman, P.E.; Jamrozik, K.; Lawrence-Brown, M.M.; Le, M.T.; Spencer, C.A.; Tuohy, R.J.; Parsons, R.W.; Dickinson, J.A. Population based randomised controlled trial on impact of screening on mortality from abdominal aortic aneurysm. BMJ 2004, 329, 1259. [Google Scholar] [CrossRef] [PubMed]
- Wanhainen, A.; Verzini, F.; Van Herzeele, I.; Allaire, E.; Bown, M.; Cohnert, T.; Dick, F.; van Herwaarden, J.; Karkos, C.; Koelemay, M.; et al. Editor’s Choice—European Society for Vascular Surgery (ESVS) 2019 Clinical Practice Guidelines on the Management of Abdominal Aorto-iliac Artery Aneurysms. Eur. J. Vasc. Endovasc. Surg. 2019, 57, 8–93. [Google Scholar] [CrossRef] [PubMed]
- Chaikof, E.L.; Dalman, R.L.; Eskandari, M.K.; Jackson, B.M.; Lee, W.A.; Mansour, M.A.; Mastracci, T.M.; Mell, M.; Murad, M.H.; Nguyen, L.L.; et al. The Society for Vascular Surgery practice guidelines on the care of patients with an abdominal aortic aneurysm. J. Vasc. Surg. 2018, 67, 2–77.e72. [Google Scholar] [CrossRef] [PubMed]
- Hellenthal, F.A.; Buurman, W.A.; Wodzig, W.K.; Schurink, G.W. Biomarkers of AAA progression. Part 1: Extracellular matrix degeneration. Nat. Rev. Cardiol. 2009, 6, 464–474. [Google Scholar] [CrossRef]
- Hellenthal, F.A.; Buurman, W.A.; Wodzig, W.K.; Schurink, G.W. Biomarkers of abdominal aortic aneurysm progression. Part 2: Inflammation. Nat. Rev. Cardiol. 2009, 6, 543–552. [Google Scholar] [CrossRef]
- Sidloff, D.A.; Stather, P.W.; Choke, E.; Bown, M.J.; Sayers, R.D. A systematic review and meta-analysis of the association between markers of hemostasis and abdominal aortic aneurysm presence and size. J. Vasc. Surg. 2014, 59, 528–535.e524. [Google Scholar] [CrossRef]
- Fan, Y.N.; Ke, X.; Yi, Z.L.; Lin, Y.Q.; Deng, B.Q.; Shu, X.R.; Yang, D.H.; Liao, Z.Y.; Nie, R.Q. Plasma D-dimer as a predictor of intraluminal thrombus burden and progression of abdominal aortic aneurysm. Life Sci. 2020, 240, 117069. [Google Scholar] [CrossRef]
- Weitz, J.I.; Fredenburgh, J.C.; Eikelboom, J.W. A Test in Context: D-Dimer. J. Am. Coll. Cardiol. 2017, 70, 2411–2420. [Google Scholar] [CrossRef]
- Arfan, S.; Zamzam, A.; Syed, M.H.; Jain, S.; Jahanpour, N.; Abdin, R.; Qadura, M. The Clinical Utility of D-Dimer and Prothrombin Fragment (F1+2) for Peripheral Artery Disease: A Prospective Study. Biomedicines 2022, 10, 878. [Google Scholar] [CrossRef]
- Folsom, A.R.; Gottesman, R.F.; Appiah, D.; Shahar, E.; Mosley, T.H. Plasma d-Dimer and Incident Ischemic Stroke and Coronary Heart Disease: The Atherosclerosis Risk in Communities Study. Stroke 2016, 47, 18–23. [Google Scholar] [CrossRef]
- Willeit, P.; Thompson, A.; Aspelund, T.; Rumley, A.; Eiriksdottir, G.; Lowe, G.; Gudnason, V.; Di Angelantonio, E. Hemostatic factors and risk of coronary heart disease in general populations: New prospective study and updated meta-analyses. PLoS ONE 2013, 8, e55175. [Google Scholar] [CrossRef]
- Mayyas, F.A.; Al-Jarrah, M.I.; Ibrahim, K.S.; Alzoubi, K.H. Level and significance of plasma myeloperoxidase and the neutrophil to lymphocyte ratio in patients with coronary artery disease. Exp. Ther. Med. 2014, 8, 1951–1957. [Google Scholar] [CrossRef]
- Tangeten, C.; Zouaoui Boudjeltia, K.; Delporte, C.; Van Antwerpen, P.; Korpak, K. Unexpected Role of MPO-Oxidized LDLs in Atherosclerosis: In between Inflammation and Its Resolution. Antioxidants 2022, 11, 874. [Google Scholar] [CrossRef]
- Karakas, M.; Koenig, W. Myeloperoxidase production by macrophage and risk of atherosclerosis. Curr. Atheroscler. Rep. 2012, 14, 277–283. [Google Scholar] [CrossRef] [PubMed]
- Haslacher, H.; Perkmann, T.; Gruenewald, J.; Exner, M.; Endler, G.; Scheichenberger, V.; Wagner, O.; Schillinger, M. Plasma myeloperoxidase level and peripheral arterial disease. Eur. J. Clin. Investig. 2012, 42, 463–469. [Google Scholar] [CrossRef] [PubMed]
- Schahab, N.; Mansuroglu, S.; Schaefer, C.; Fimmers, R.; Nickenig, G.; Tiyerili, V. Prognostic value of myeloperoxidase in patients with peripheral artery disease. Vascular 2021, 29, 363–371. [Google Scholar] [CrossRef] [PubMed]
- Memon, A.A.; Zarrouk, M.; Agren-Witteschus, S.; Sundquist, J.; Gottsater, A.; Sundquist, K. Identification of novel diagnostic and prognostic biomarkers for abdominal aortic aneurysm. Eur. J. Prev. Cardiol. 2020, 27, 132–142. [Google Scholar] [CrossRef]
- Zagrapan, B.; Eilenberg, W.; Prausmueller, S.; Nawrozi, P.; Muench, K.; Hetzer, S.; Elleder, V.; Rajic, R.; Juster, F.; Martelanz, L.; et al. A Novel Diagnostic and Prognostic Score for Abdominal Aortic Aneurysms Based on D-Dimer and a Comprehensive Analysis of Myeloid Cell Parameters. Thromb. Haemost. 2019, 119, 807–820. [Google Scholar] [CrossRef]
- Starlinger, P.; Moll, H.P.; Assinger, A.; Nemeth, C.; Hoetzenecker, K.; Gruenberger, B.; Gruenberger, T.; Kuehrer, I.; Schoppmann, S.F.; Gnant, M.; et al. Thrombospondin-1: A unique marker to identify in vitro platelet activation when monitoring in vivo processes. J. Thromb. Haemost. 2010, 8, 1809–1819. [Google Scholar] [CrossRef] [PubMed]
- Nomura, F.; Ihara, A.; Yoshitatsu, M.; Tamura, K.; Katayama, A.; Ihara, K. Relationship between coagulation cascade, cytokine, adhesion molecule and aortic aneurysm. Eur. J. Cardiothorac. Surg. 2003, 23, 1034–1038, discussion 1038–1039. [Google Scholar] [CrossRef] [PubMed]
- Dale, M.A.; Ruhlman, M.K.; Baxter, B.T. Inflammatory cell phenotypes in AAAs: Their role and potential as targets for therapy. Arterioscler. Thromb. Vasc. Biol. 2015, 35, 1746–1755. [Google Scholar] [CrossRef] [PubMed]
- Aday, A.W.; Matsushita, K. Epidemiology of Peripheral Artery Disease and Polyvascular Disease. Circ. Res. 2021, 128, 1818–1832. [Google Scholar] [CrossRef] [PubMed]
- Tong, J.; Cohnert, T.; Holzapfel, G.A. Diameter-related variations of geometrical, mechanical, and mass fraction data in the anterior portion of abdominal aortic aneurysms. Eur. J. Vasc. Endovasc. Surg. 2015, 49, 262–270. [Google Scholar] [CrossRef] [PubMed]
- Narula, N.; Olin, J.W.; Narula, N. Pathologic Disparities between Peripheral Artery Disease and Coronary Artery Disease. Arterioscler. Thromb. Vasc. Biol. 2020, 40, 1982–1989. [Google Scholar] [CrossRef]
- Moxon, J.V.; Liu, D.; Wong, G.; Weir, J.M.; Behl-Gilhotra, R.; Bradshaw, B.; Kingwell, B.A.; Meikle, P.J.; Golledge, J. Comparison of the serum lipidome in patients with abdominal aortic aneurysm and peripheral artery disease. Circ. Cardiovasc. Genet. 2014, 7, 71–79. [Google Scholar] [CrossRef]
- Vega de Ceniga, M.; Esteban, M.; Barba, A.; Estallo, L.; Blanco-Colio, L.M.; Martin-Ventura, J.L. Assessment of biomarkers and predictive model for short-term prospective abdominal aortic aneurysm growth—A pilot study. Ann. Vasc. Surg. 2014, 28, 1642–1648. [Google Scholar] [CrossRef]
- Busti, C.; Falcinelli, E.; Momi, S.; Gresele, P. Matrix metalloproteinases and peripheral arterial disease. Intern. Emerg. Med. 2010, 5, 13–25. [Google Scholar] [CrossRef]
- Eilenberg, W.; Zagrapan, B.; Bleichert, S.; Ibrahim, N.; Knobl, V.; Brandau, A.; Martelanz, L.; Grasl, M.T.; Hayden, H.; Nawrozi, P.; et al. Histone citrullination as a novel biomarker and target to inhibit progression of abdominal aortic aneurysms. Transl. Res. 2021, 233, 32–46. [Google Scholar] [CrossRef] [PubMed]
- Houard, X.; Touat, Z.; Ollivier, V.; Louedec, L.; Philippe, M.; Sebbag, U.; Meilhac, O.; Rossignol, P.; Michel, J.B. Mediators of neutrophil recruitment in human abdominal aortic aneurysms. Cardiovasc. Res. 2009, 82, 532–541. [Google Scholar] [CrossRef] [PubMed]
- Plana, E.; Oto, J.; Medina, P.; Fernandez-Pardo, A.; Miralles, M. Novel contributions of neutrophils in the pathogenesis of abdominal aortic aneurysm, the role of neutrophil extracellular traps: A systematic review. Thromb. Res. 2020, 194, 200–208. [Google Scholar] [CrossRef] [PubMed]
- Raffort, J.; Lareyre, F.; Clement, M.; Hassen-Khodja, R.; Chinetti, G.; Mallat, Z. Monocytes and macrophages in abdominal aortic aneurysm. Nat. Rev. Cardiol. 2017, 14, 457–471. [Google Scholar] [CrossRef] [PubMed]
- Libby, P. Inflammation during the life cycle of the atherosclerotic plaque. Cardiovasc. Res. 2021, 117, 2525–2536. [Google Scholar] [CrossRef] [PubMed]
- Back, M.; Weber, C.; Lutgens, E. Regulation of atherosclerotic plaque inflammation. J. Intern. Med. 2015, 278, 462–482. [Google Scholar] [CrossRef] [PubMed]
- Signorelli, S.S.; Fiore, V.; Malaponte, G. Inflammation and peripheral arterial disease: The value of circulating biomarkers (Review). Int. J. Mol. Med. 2014, 33, 777–783. [Google Scholar] [CrossRef]
- Treska, V.; Topolcan, O.; Pecen, L. Cytokines as plasma markers of abdominal aortic aneurysm. Clin. Chem. Lab. Med. 2000, 38, 1161–1164. [Google Scholar] [CrossRef]
- Norman, P.; Spencer, C.A.; Lawrence-Brown, M.M.; Jamrozik, K. C-reactive protein levels and the expansion of screen-detected abdominal aortic aneurysms in men. Circulation 2004, 110, 862–866. [Google Scholar] [CrossRef]
- Speidl, W.S.; Exner, M.; Amighi, J.; Mlekusch, W.; Sabeti, S.; Kastl, S.P.; Zorn, G.; Maurer, G.; Wagner, O.; Huber, K.; et al. Complement component C5a predicts restenosis after superficial femoral artery balloon angioplasty. J. Endovasc. Ther. 2007, 14, 62–69. [Google Scholar] [CrossRef]
- Zagrapan, B.; Eilenberg, W.; Scheuba, A.; Klopf, J.; Brandau, A.; Story, J.; Dosch, K.; Hayden, H.; Domenig, C.M.; Fuchs, L.; et al. Complement Factor C5a Is Increased in Blood of Patients with Abdominal Aortic Aneurysm and Has Prognostic Potential for Aneurysm Growth. J. Cardiovasc. Transl. Res. 2021, 14, 761–769. [Google Scholar] [CrossRef]
- Wiernicki, I.; Stachowska, E.; Safranow, K.; Cnotliwy, M.; Rybicka, M.; Kaczmarczyk, M.; Gutowski, P. Enhanced matrix-degrading proteolytic activity within the thin thrombus-covered wall of human abdominal aortic aneurysms. Atherosclerosis 2010, 212, 161–165. [Google Scholar] [CrossRef] [PubMed]
- Koch, V.; Booz, C.; Gruenewald, L.D.; Albrecht, M.H.; Gruber-Rouh, T.; Eichler, K.; Yel, I.; Mahmoudi, S.; Scholtz, J.E.; Martin, S.S.; et al. Diagnostic performance and predictive value of D-dimer testing in patients referred to the emergency department for suspected myocardial infarction. Clin. Biochem. 2022, 104, 22–29. [Google Scholar] [CrossRef] [PubMed]
- Kikkert, W.J.; Claessen, B.E.; Stone, G.W.; Mehran, R.; Witzenbichler, B.; Brodie, B.R.; Wohrle, J.; Witkowski, A.; Guagliumi, G.; Zmudka, K.; et al. D-dimer levels predict ischemic and hemorrhagic outcomes after acute myocardial infarction: A HORIZONS-AMI biomarker substudy. J. Thromb. Thrombolysis 2014, 37, 155–164. [Google Scholar] [CrossRef] [PubMed]
- Kim, H.W.; Blomkalns, A.L.; Ogbi, M.; Thomas, M.; Gavrila, D.; Neltner, B.S.; Cassis, L.A.; Thompson, R.W.; Weiss, R.M.; Lindower, P.D.; et al. Role of myeloperoxidase in abdominal aortic aneurysm formation: Mitigation by taurine. Am. J. Physiol. Heart Circ. Physiol. 2017, 313, H1168–H1179. [Google Scholar] [CrossRef]
- Cai, H.; Pan, B.; Xu, J.; Liu, S.; Wang, L.; Wu, K.; Yang, P.; Huang, J.; Wang, W. D-Dimer is a Diagnostic Biomarker of Abdominal Aortic Aneurysm in Patients with Peripheral Artery Disease. Front. Cardiovasc. Med. 2022, 9, 890228. [Google Scholar] [CrossRef]


| Parameter | Healthy (n = 41) | PAD (n = 43) | AAA Cohort 1 (n = 41) | AAA Cohort 2 (n = 37) | p-Value | ||
|---|---|---|---|---|---|---|---|
| Metric variables | n | Median (IQR) | Median (IQR) | Median (IQR) | Median (IQR) | ||
| Age [years] | 41/43/41/37 | 71.4 (13.3) | 72.3 (11.9) | 71.8 (12.4) | 69.2 (11.7) | n.s. a | |
| Smoking pack-years [py] | 40/43/39/35 | 8.5 (27.5) | 37.0 (45.0) | 38.0 (35.0) | 40.0 (18.0) | H:P—<0.001 a H:A1—<0.001 a H:A2—<0.001 a | |
| Body mass index | 32/43/40/37 | 26.1 (4.6) | 25.8 (3.7) | 27.6 (5.6) | 26.8 (6.5) | P:A1—0.021 a P:A2—0.011 a | |
| Thrombocytes [109/l] | 40/42/38/34 | 239 (102) | 228 (105) | 208 (65) | 218 (79) | H:A1—0.030 a | |
| Leukocytes [109/l] | 40/42/38/34 | 6.99 (3.21) | 7.48 (2.93) | 6.96 (2.43) | 7.40 (3.37) | n.s. a | |
| Neutrophils [109/l] | 39/38/38/31 | 4.3 (2.4) | 4.7 (2.0) | 4.7 (2.1) | 4.3 (2.6) | n.s. a | |
| Fibrinogen [mg/dl] | 39/42/38/34 | 359 (90) | 342 (90) | 354 (141) | 361 (90) | n.s. a | |
| Cholesterol total [mg/dl] | 41/43/39/36 | 198 (49) | 145 (49) | 172 (77) | 179 (55) | H:P—<0.001 a H:A2—0.027 a P:A1—0.008 a P:A2—0.005 a | |
| High-density lipoprotein [mg/dl] | 41/43/39/36 | 53 (18) | 53 (26) | 49 (21) | 48 (24) | H:A1—0.049 a | |
| Triglycerides [mg/dl] | 41/43/39/36 | 136 (91) | 89 (74) | 136 (127) | 120 (130) | P:A1—0.006 a P:A2—0.030 a | |
| HbA1c [%] | 38/43/35/36 | 5.5 (0.5) | 5.7 (0.6) | 5.7 (0.5) | 5.8 (0.8) | H:P—0.021 a H:A1—0.008 a H:A2—0.002 a | |
| C-reactive protein [mg/dl] | 41/43/39/36 | 0.18 (0.28) | 0.20 (0.39) | 0.27 (0.45) | 0.24 (0.43) | n.s. a | |
| Maximal AAA diameter [mm] | 40/35 | 51.8 (10.9) | 47.8 (12.9) | n.s. a | |||
| Aortic segment volume [cm³] | 28/31 | 121.6 (95.7) | 93.3 (70.3) | n.s. a | |||
| Maximal ILT diameter [mm] | 30/31 | 15.1 (14.8) | 16.6 (14.1) | n.s. a | |||
| ILT volume [cm³] | 27/31 | 42.5 (77.7) | 35.5 (44.6) | n.s. a | |||
| Categorical variables | n | n (%) | n (%) | n (%) | n (%) | ||
| Sex | Men | 41/43/41/37 | 32 (78.0) | 34 (79.1) | 32 (78.0) | 31 (83.8) | n.s. b |
| Women | 9 (22.0) | 9 (20.9) | 9 (22.0) | 6 (16.2) | |||
| Smoking | Never | 41/43/41/36 | 13 (31.7) | 3 (7.0) | 3 (7.3) | 2 (5.6) | H:P—0.016 b H:A1—0.019 b H:A2—0.020 b |
| Past | 17 (41.5) | 24 (55.8) | 21 (51.2) | 18 (50.0) | |||
| Current | 11 (26.8) | 16 (37.2) | 17 (41.5) | 16 (44.4) | |||
| Hypertension | 41/43/41/37 | 22 (53.7) | 39 (90.7) | 38 (92.7) | 28 (75.7) | H:P—<0.001 b H:A1—<0.001 b H:A2—0.043 b A1:A2—0.038 b | |
| Hyperlipidaemia | 40/43/41/37 | 10 (25.0) | 31 (72.1) | 34 (82.9) | 32 (86.5) | H:P—<0.001 b H:A1—<0.001 b H:A2—<0.001 b | |
| Peripheral artery disease | 41/43/41/37 | 0 (0.0) | 43 (100.0) | 0 (0.0) | 13 (35.1) | H:P—<0.001 b H:A2—<0.001 b P:A1—<0.001 b P:A2—<0.001 b A1:A2—<0.001 b | |
| Coronary heart disease | 41/43/41/37 | 0 (0.0) | 19 (44.2) | 21 (51.2) | 18 (48.6) | H:P—<0.001 b H:A1—<0.001 b H:A2—<0.001 b | |
| Myocardial infarction | 41/43/40/37 | 0 (0.0) | 10 (23.3) | 12 (30.0) | 9 (24.3) | H:P—0.001 c H:A1—<0.001 b H:A2—0.001 c | |
| Stroke | 41/43/41/37 | 0 (0.0) | 6 (14.0) | 4 (9.8) | 3 (8.1) | H:P—0.026 c | |
| Vascular Stent | 41/43/40/36 | 0 (0.0) | 27 (62.8) | 10 (25.0) | 10 (27.8) | H:P—<0.001 b H:A1—0.002 b H:A2—0.001 b P:A1—0.001 b P:A2—0.005 b | |
| Diabetes mellitus type 2 | 41/43/41/37 | 5 (12.2) | 11 (25.6) | 12 (29.3) | 12 (32.4) | H:A2—0.031 b | |
| Chronic obstructive pulmonary disease | 41/43/41/37 | 1 (2.4) | 14 (32.6) | 9 (22.0) | 11 (29.7) | H:P—<0.001 b H:A1—0.007 b H:A2—<0.001 b | |
| Antiplatelet therapy | 41/43/41/37 | 6 (14.6) | 38 (88.4) | 38 (92.7) | 33 (89.2) | H:P—<0.001 b H:A1—<0.001 b H:A2—<0.001 b | |
| Anticoagulation therapy | 41/43/41/37 | 3 (7.3) | 7 (16.3) | 5 (12.2) | 5 (13.5) | n.s. b | |
| Antihypertensive therapy | 41/43/41/37 | 22 (53.7) | 36 (83.7) | 38 (92.7) | 33 (89.2) | H:P—0.003 b H:A1—<0.001 b H:A2—0.001 b | |
| Lipid-lowering agents | 41/43/41/37 | 7 (17.1) | 39 (90.7) | 35 (85.4) | 34 (91.9) | H:P—<0.001 b H:A1—<0.001 b H:A2—<0.001 b | |
| Parameter | Healthy (n = 41) | PAD (n = 43) | AAA Cohort 1 (n = 41) | AAA Cohort 2 (n = 37) | p-Value | |
|---|---|---|---|---|---|---|
| Metric variables | n | Median (IQR) | Median (IQR) | Median (IQR) | Median (IQR) | |
| MPO [ng/mL] | 41/43/41/37 | 9.16 (6.57–13.63) | 11.74 (8.70–13.64) | 13.63 (10.92–22.19) | 14.36 (10.08–19.73) | H:P—0.055 H:A1—<0.001 H:A2—<0.001 P:A1—0.004 P:A2—0.034 A1:A2—0.462 |
| D-dimer [µg/mL] | 41/43/41/37 | 0.38 (0.00–0.51) | 0.58 (0.42–0.97) | 1.27 (0.55–1.73) | 0.90 (0.52–1.60) | H:P—<0.001 H:A1—<0.001 H:A2—<0.001 P:A1—0.006 P:A2—0.070 A1:A2—0.258 |
| Score | 41/43/41/37 | −0.93 (−1.55–−0.09) | −0.19 (−0.73–0.71) | 1.26 (0.12—4.06) | 1.07 (−0.35—2.34) | H:P—0.002 H:A1—<0.001 H:A2—<0.001 P:A1—<0.001 P:A2—0.014 A1:A2—0.248 |
| Parameter | Exp(B) | 95% CI Lower Value | 95% CI Upper Value | p-Value |
|---|---|---|---|---|
| Score (dichotomised) | 22.296 | 5.841 | 85.113 | <0.001 |
| Smoking (ever) | 7.941 | 1.115 | 56.559 | 0.039 |
| Hypertension | 2.670 | 0.465 | 15.344 | 0.271 |
| Hyperlipidaemia | 10.880 | 2.701 | 43.823 | 0.001 |
| Coronary heart disease | 13.196 | 2.201 | 79.126 | 0.005 |
| Myocardial infarction | 1.577 | 0.294 | 8.463 | 0.595 |
| Stroke | 0.535 | 0.080 | 3.551 | 0.517 |
| Vascular Stent | 0.041 | 0.007 | 0.241 | <0.001 |
| Chronic obstructive pulmonary disease | 0.528 | 0.131 | 2.132 | 0.370 |
| Constant | 0.001 | <0.001 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Zagrapan, B.; Klopf, J.; Celem, N.D.; Brandau, A.; Rossi, P.; Gordeeva, Y.; Szewczyk, A.R.; Liu, L.; Ahmadi-Fazel, D.; Najarnia, S.; et al. Diagnostic Utility of a Combined MPO/D-Dimer Score to Distinguish Abdominal Aortic Aneurysm from Peripheral Artery Disease. J. Clin. Med. 2023, 12, 7558. https://doi.org/10.3390/jcm12247558
Zagrapan B, Klopf J, Celem ND, Brandau A, Rossi P, Gordeeva Y, Szewczyk AR, Liu L, Ahmadi-Fazel D, Najarnia S, et al. Diagnostic Utility of a Combined MPO/D-Dimer Score to Distinguish Abdominal Aortic Aneurysm from Peripheral Artery Disease. Journal of Clinical Medicine. 2023; 12(24):7558. https://doi.org/10.3390/jcm12247558
Chicago/Turabian StyleZagrapan, Branislav, Johannes Klopf, Nihan Dide Celem, Annika Brandau, Patrick Rossi, Yulia Gordeeva, Alexandra Regina Szewczyk, Linda Liu, Diana Ahmadi-Fazel, Sina Najarnia, and et al. 2023. "Diagnostic Utility of a Combined MPO/D-Dimer Score to Distinguish Abdominal Aortic Aneurysm from Peripheral Artery Disease" Journal of Clinical Medicine 12, no. 24: 7558. https://doi.org/10.3390/jcm12247558
APA StyleZagrapan, B., Klopf, J., Celem, N. D., Brandau, A., Rossi, P., Gordeeva, Y., Szewczyk, A. R., Liu, L., Ahmadi-Fazel, D., Najarnia, S., Fuchs, L., Hayden, H., Loewe, C., Eilenberg, W., Neumayer, C., & Brostjan, C. (2023). Diagnostic Utility of a Combined MPO/D-Dimer Score to Distinguish Abdominal Aortic Aneurysm from Peripheral Artery Disease. Journal of Clinical Medicine, 12(24), 7558. https://doi.org/10.3390/jcm12247558