Orofacial Pain, Musical Performance and Associated Coping Behaviors, Psychological Distress and Disability among Asian Young Adults
Abstract
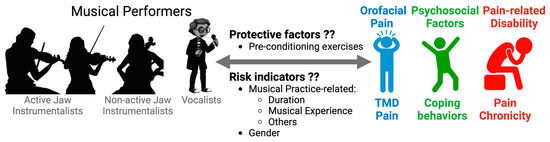
:1. Introduction
2. Materials and Methods
2.1. Participants
2.2. Survey Questionnaires
2.3. Statistical Analysis
3. Results
4. Discussion
4.1. OFP Prevalence and Musical Practice Outcomes
4.2. OFP Chronicity, Disability, and Psychosocial Factors among Musicians
4.3. Limitations of the Study
4.4. Future Research
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Von Korff, M.; Dworkin, S.F.; Le Resche, L.; Kruger, A. An epidemiologic comparison of pain complaints. Pain 1988, 32, 173–183. [Google Scholar] [CrossRef] [PubMed]
- Goulet, J.P.; Lavigne, G.J.; Lund, J.P. Jaw pain prevalence among French-speaking Canadians in Quebec and related symptoms of temporomandibular disorders. J. Dent. Res. 1995, 74, 1738–1744. [Google Scholar] [CrossRef] [PubMed]
- Ohrbach, R.; Bair, E.; Fillingim, R.B.; Gonzalez, Y.; Gordon, S.M.; Lim, P.-F.; Ribeiro-Dasilva, M.; Diatchenko, L.; Dubner, R.; Greenspan, J.D.; et al. Clinical orofacial characteristics associated with risk of first-onset TMD: The OPPERA prospective cohort study. J. Pain 2013, 14, T33–T50. [Google Scholar] [CrossRef]
- Slade, G.D.; Fillingim, R.B.; Sanders, A.E.; Bair, E.; Greenspan, J.D.; Ohrbach, R.; Dubner, R.; Diatchenko, L.; Smith, S.B.; Knott, C.; et al. Summary of findings from the OPPERA prospective cohort study of incidence of first-onset temporomandibular disorder: Implications and future directions. J. Pain 2013, 14, T116–T124. [Google Scholar] [CrossRef]
- van Selms, M.K.A.; Wiegers, J.W.; van der Meer, H.A.; Ahlberg, J.; Lobbezoo, F.; Visscher, C.M. Temporomandibular disorders, pain in the neck and shoulder area, and headache among musicians. J. Oral Rehabil. 2020, 47, 132–142. [Google Scholar] [CrossRef] [PubMed]
- Zimmers, P.L.; Gobetti, J.P. Head and neck lesions commonly found in musicians. J. Am. Dent. Assoc. 1994, 125, 1487–1490. [Google Scholar] [CrossRef] [PubMed]
- Rodríguez-Lozano, F.J.; Sáez-Yuguero, M.R.; Bermejo-Fenoll, A. Prevalence of temporomandibular disorder-related findings in violinists compared with control subjects. Oral Surg. Oral Med. Oral Pathol. Oral Radiol. 2010, 109, E15–E19. [Google Scholar] [CrossRef]
- Steinmetz, A.; Zeh, A.; Delank, K.S.; Peroz, I. Symptoms of craniomandibular dysfunction in professional orchestra musicians. Occup. Med. 2014, 64, 17–22. [Google Scholar] [CrossRef]
- Taddey, J.J. Musicians and temporomandibular disorders: Prevalence and occupational etiologic considerations. CRANIO 1992, 10, 241–244. [Google Scholar] [CrossRef] [PubMed]
- Piron, A.; Roch, J.B. Temporomandibular dysfunction and dysphonia (TMD). Rev. Laryngol. Otol. Rhinol. 2010, 131, 31–34. [Google Scholar]
- van Selms, M.K.A.; Wiegers, J.W.; Lobbezoo, F.; Visscher, C.M. Are vocalists prone to temporomandibular disorders? J. Oral Rehabil. 2019, 46, 1127–1132. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- van Selms, M.K.A.; Ahlberg, J.; Lobbezoo, F.; Visscher, C.M. Evidence-based review on temporomandibular disorders among musicians. Occup. Med. 2017, 67, 336–343. [Google Scholar] [CrossRef] [PubMed]
- Campos, L.G.N.; Pedrosa, B.H.; Cavalcanti, R.V.A.; Stechman-Neto, J.; Gadotti, I.C.; de Araujo, C.M.; Taveira, K.V.M. Prevalence of temporomandibular disorders in musicians: A systematic review and meta-analysis. J. Oral Rehabil. 2021, 48, 632–642. [Google Scholar] [CrossRef]
- Ackermann, B.; Driscoll, T.; Kenny, D.T. Musculoskeletal pain and injury in professional orchestral musicians in Australia. Med. Probl. Perform. Art. 2012, 27, 181–187. [Google Scholar] [CrossRef] [PubMed]
- Steinmetz, A.; Scheffer, I.; Esmer, E.; Delank, K.S.; Peroz, I. Frequency, severity and predictors of playing-related musculoskeletal pain in professional orchestral musicians in Germany. Clin. Rheumatol. 2015, 34, 965–973. [Google Scholar] [CrossRef] [PubMed]
- Kenny, D.T.; Driscoll, T.; Ackermann, B.J. Is Playing in the Pit Really the Pits?: Pain, Strength, Music Performance Anxiety, and Workplace Satisfaction in Professional Musicians in Stage, Pit, and Combined Stage/Pit Orchestras. Med. Probl. Perform. Art. 2016, 31, 1–7. [Google Scholar] [CrossRef]
- Gonzalez, Y.M.; Schiffman, E.; Gordon, S.M.; Seago, B.; Truelove, E.L.; Slade, G.; Ohrbach, R. Development of a brief and effective temporomandibular disorder pain screening questionnaire: Reliability and validity. J. Am. Dent. Assoc. 2011, 142, 1183–1191. [Google Scholar] [CrossRef]
- Von Korff, M. Assessment of chronic pain in epidemiological and health services research: Empirical bases and new directions. In Handbook of Pain Assessment, 3rd ed.; Turk, D.C., Melzack, R., Eds.; Guilford Press: New York, NY, USA, 2011; pp. 455–473. [Google Scholar]
- Sinclair, V.G.; Wallston, K.A. The development and psychometric evaluation of the Brief Resilient Coping Scale. Assessment 2004, 11, 94–101. [Google Scholar] [CrossRef]
- Kroenke, K.; Spitzer, R.L.; Williams, J.B.; Löwe, B. An ultra-brief screening scale for anxiety and depression: The PHQ-4. Psychosomatics 2009, 50, 613–621. [Google Scholar] [CrossRef]
- Spitzer, R.L.; Kroenke, K.; Williams, J.B.; Löwe, B. A brief measure for assessing generalized anxiety disorder: The GAD-7. Arch. Intern. Med. 2006, 166, 1092–1097. [Google Scholar] [CrossRef]
- Mitchell, A.M.; Crane, P.A.; Kim, Y. Perceived stress in survivors of suicide: Psychometric properties of the Perceived Stress Scale. Res. Nurs. Health 2008, 31, 576–585. [Google Scholar] [CrossRef] [PubMed]
- Vaiano, T.; Guerrieri, A.C.; Behlau, M. Body pain in classical choral singers. CoDAS 2013, 25, 303–309. [Google Scholar] [CrossRef] [PubMed]
- Middlestadt, S.E.; Fishbein, M. Health and occupational correlates of perceived occupational stress in symphony orchestra musicians. J. Occup. Med. 1988, 30, 687–692. [Google Scholar]
- Pow, E.H.; Leung, K.C.; McMillan, A.S. Prevalence of symptoms associated with temporomandibular disorders in Hong Kong Chinese. J. Orofac. Pain 2001, 15, 228–234. [Google Scholar]
- Yap, A.U.; Dworkin, S.F.; Chua, E.K.; List, T.; Tan, K.B.; Tan, H.H. Prevalence of temporomandibular disorder subtypes, psychologic distress, and psychosocial dysfunction in Asian patients. J. Orofac. Pain 2003, 17, 21–28. [Google Scholar] [PubMed]
- Steinmetz, A.; Ridder, P.H.; Methfessel, G.; Muche, B. Professional musicians with craniomandibular dysfunctions treated with oral splints. CRANIO 2009, 27, 221–230. [Google Scholar] [CrossRef] [PubMed]
- Taheri, A.; Lajevardi, M.; Shabani, S.; Emami, S.; Sharifi, H. Could the Addition of Alexander Technique Improve the Effectiveness of Physical Therapy in Reducing Violinists’ Neck Pain in Comparison to Physical Therapy Alone? Med. Probl. Perform. Art. 2017, 32, 60. [Google Scholar] [CrossRef] [PubMed]
- Klein, S.D.; Bayard, C.; Wolf, U. The Alexander Technique and musicians: A systematic review of controlled trials. BMC Complement. Altern. Med. 2014, 14, 414. [Google Scholar] [CrossRef] [PubMed]
- Kuo, Y.L.; Lee, T.H.; Tsai, Y.J. Evaluation of a Cervical Stabilization Exercise Program for Pain, Disability, and Physical Impairments in University Violinists with Nonspecific Neck Pain. Int. J. Environ. Res. Public Health 2020, 17, 5430. [Google Scholar] [CrossRef]
- Kok, L.M.; Groenewegen, K.A.; Huisstede, B.M.A.; Nelissen, R.G.H.H.; Rietveld, A.B.M.; Haitjema, S. The high prevalence of playing-related musculoskeletal disorders (PRMDs) and its associated factors in amateur musicians playing in student orchestras: A cross-sectional study. PLoS ONE 2018, 13, e0191772. [Google Scholar] [CrossRef] [Green Version]
| Musician Categories | Definition Criteria | Musical Instruments |
|---|---|---|
| Vocal | Vocalists | Not applicable |
| Active Jaw | Musicians that require oromandibular activities to play an instrument. | Violin, Viola, Clarinet, Trombone, Euphonium, French Horn, Trumpet, Oboe, Tuba, Flute, Bassoon, Harmonica, Saxophone |
| Non-active Jaw | Musicians that do not require oromandibular activities to play an instrument. | Piano, Guitar, Cello, Guzheng, Harp, Drum, Keyboard |
| Vocal | Instrumentalists | p Value | ||
|---|---|---|---|---|
| Active Jaw | Non-Active Jaw | |||
| (n = 64) | (n = 70) | (n = 25) | ||
| Age (y), mean ± SD | 20.67 ± 1.6 | 20.20 ± 1.4 | 19.40 ± 4.2 | 0.068 |
| Gender, n (%) | 0.568 | |||
| Male | 27 (42.2) | 30 (42.9) | 8 (32) | |
| Female | 37 (57.8) | 40 (57.1) | 17 (68) | |
| Race, n (%) | 0.056 | |||
| Chinese | 61 (95.3) | 62 (88.6) | 23 (92) | |
| Non-Chinese | 3 (4.7) | 8 (11.4) | 2 (8) | |
| Musical experience (years), n (%) | 0.015 | |||
| 1–3 | 19 (29.7) | 5 (7.1) | 3 (12) | |
| 4–6 | 18 (28.1) | 19 (27.1) | 5 (20) | |
| 7–9 | 10 (15.6) | 16 (22.9) | 8 (32) | |
| ≥10 | 17 (26.6) | 30 (42.9) | 9 (36) | |
| Average duration of each musical practice (min), n (%) | 0.01 | |||
| <30 | 37 (57.8) | 23 (32.9) | 14 (56) | |
| 30–60 | 20 (31.3) | 33 (47.1) | 11 (44) | |
| >60 | 7 (10.9) | 14 (20) | 0 (0) | |
| Breaks during musical practice, n (%) | 0.344 | |||
| No | 11 (17.2) | 7 (10) | 2 (8) | |
| Yes | 53 (82.8) | 63 (90) | 23 (92) | |
| History of trauma while playing, n (%) | 0.75 | |||
| No | 59 (92.2) | 63 (90) | 24 (96) | |
| Yes | 5 (7.8) | 7 (10) | 1 (4) | |
| Jaw/neck pre-conditioning exercises, n (%) | <0.0001 | |||
| No | 16 (25) | 61 (87.1) | 24 (96) | |
| Yes | 48 (75) | 9 (12.9) | 1 (4) | |
| Vocal | Active Jaw | Non-Active Jaw | p Value | |
|---|---|---|---|---|
| (n = 64) | (n = 70) | (n = 25) | ||
| TMD pain (TMD-PS), n (%) | ||||
| No | 56 (87.5) | 62 (88.6) | 24 (96) | 0.681 |
| Yes | 8 (12.5) | 8 (11.4) | 1 (4) | |
| CPI (0–10) | 0.15 (0–7) | 0 (0–6) | 0 (0–4) | 0.756 |
| Median (range) | ||||
| Pain duration/chronicity, days | 2 (0–90) | 0 (0–180) | 0 (0–20) | 0.193 |
| Median (range) | ||||
| Pain-related disability days | 0 (0–7) | 0 (0–5) | 0 (0–2) | 0.805 |
| Median (range) |
| Vocal | Active Jaw | Non-Active | p Value | |
|---|---|---|---|---|
| Jaw | ||||
| (n = 64) | (n = 70) | (n = 25) | ||
| Resilient Coping Behaviors | 14 (10–20) | 14.5 (8–20) | 14 (9–18) | 0.475 |
| Median (range) | ||||
| Anxiety severity | 5.5 (0–17) | 5 (0–19) | 5 (0–11) | 0.443 |
| Median (range) | ||||
| Psychological distress | 3 (0–10) | 3.5 (0–9) | 4 (0–7) | 0.89 |
| Median (range) | ||||
| Perceived stress | 17 (7–28) | 17 (5–27) | 18 (7–26) | 0.722 |
| Median (range) |
| Types of Performance Related OFP | Vocal | Active Jaw | Non-Active | p Value |
|---|---|---|---|---|
| Jaw | ||||
| (n = 64) | (n = 70) | (n = 25) | ||
| OFP while playing, n (%) | 0.002 | |||
| No | 53 (82.8) | 41 (58.6) | 13 (52) | |
| Yes | 11 (17.2) | 29 (41.4) | 12 (48) | |
| OFP that progresses while playing, n (%) | 0.035 | |||
| No | 55 (85.9) | 49 (70) | 16 (64) | |
| Yes | 9 (14.1) | 21 (30) | 9 (36) | |
| OFP that persists after playing, n (%) | 0.113 | |||
| No | 55 (85.9) | 52 (74.3) | 17 (68) | |
| Yes | 9 (14.1) | 18 (25.7) | 8 (32) | |
| OFP that reduces playing, n (%) | 0.001 | |||
| No | 64 (100) | 56 (80) | 22 (88) | |
| Yes | 0 (0) | 14 (20) | 3 (12) |
| Dependent Variables | |||||||
|---|---|---|---|---|---|---|---|
| OFP while Playing | OFP That Progresses while Playing | ||||||
| OR | 95% CI | p Value | OR | 95% CI | p Value | ||
| Musician groups | Active Jaw vs. Vocal | 3.819 | 1.298–11.236 | 0.015 | 2.904 | 0.862–9.786 | 0.085 |
| Non-active Jaw vs. Vocal | 4.214 | 1.173–15.143 | 0.028 | 3.646 | 0.906–14.676 | 0.069 | |
| Musical Experience | 4–6 vs. 1–3 years | 0.988 | 0.338–2.890 | 0.982 | 0.325 | 0.105–1.010 | 0.052 |
| ≥10 vs. 7–9 years | 1.077 | 0.350–3.316 | 0.897 | 0.749 | 0.243–2.309 | 0.614 | |
| Duration of Each Musical Practice | 30–60 min vs. <30 min | 0.545 | 0.247–1.204 | 0.133 | 0.697 | 0.296–1.640 | 0.408 |
| >60 min vs. <30 min | 0.929 | 0.308–2.798 | 0.896 | 0.537 | 0.144–2.007 | 0.355 | |
| Jaw/Neck | Once a day/Everyday vs. Never | 0.946 | 0.341–2.627 | 0.915 | 0.746 | 0.235–2.372 | 0.62 |
| Pre-conditioning Exercises | |||||||
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Nair, R.; Tanikawa, C.; Ferreira, J.N. Orofacial Pain, Musical Performance and Associated Coping Behaviors, Psychological Distress and Disability among Asian Young Adults. J. Clin. Med. 2023, 12, 1271. https://doi.org/10.3390/jcm12041271
Nair R, Tanikawa C, Ferreira JN. Orofacial Pain, Musical Performance and Associated Coping Behaviors, Psychological Distress and Disability among Asian Young Adults. Journal of Clinical Medicine. 2023; 12(4):1271. https://doi.org/10.3390/jcm12041271
Chicago/Turabian StyleNair, Rahul, Chihiro Tanikawa, and Joao N. Ferreira. 2023. "Orofacial Pain, Musical Performance and Associated Coping Behaviors, Psychological Distress and Disability among Asian Young Adults" Journal of Clinical Medicine 12, no. 4: 1271. https://doi.org/10.3390/jcm12041271
APA StyleNair, R., Tanikawa, C., & Ferreira, J. N. (2023). Orofacial Pain, Musical Performance and Associated Coping Behaviors, Psychological Distress and Disability among Asian Young Adults. Journal of Clinical Medicine, 12(4), 1271. https://doi.org/10.3390/jcm12041271