Sex-Related Differences among Adults with Hypertrophic Obstructive Cardiomyopathy Undergoing Transcoronary Ablation of Septal Hypertrophy
Abstract
:1. Introduction
2. Materials and Methods
2.1. Study Population and Design
2.2. TASH Protocol and Non-Invasive Investigations
2.3. Statistical Analysis
3. Results
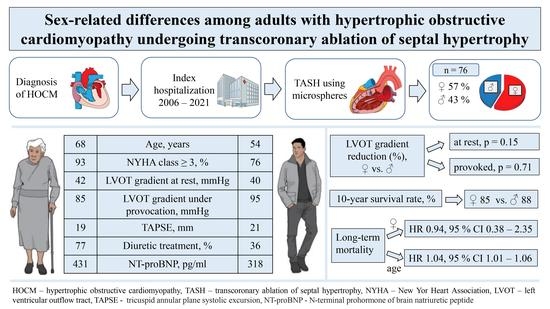
3.1. Baseline Characteristics
3.2. Periprocedural Outcomes
3.3. Long-Term Follow-up
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Pelliccia, F.; Limongelli, G.; Autore, C.; Gimeno-Blanes, J.R.; Basso, C.; Elliott, P. Sex-related differences in cardiomyopathies. Int. J. Cardiol. 2019, 286, 239–243. [Google Scholar] [CrossRef]
- Geske, J.B.; Ong, K.C.; Siontis, K.C.; Hebl, V.B.; Ackerman, M.J.; Hodge, D.O.; Miller, V.M.; Nishimura, R.A.; Oh, J.K.; Schaff, H.V.; et al. Women with hypertrophic cardiomyopathy have worse survival. Eur. Heart J. 2017, 38, 3434–3440. [Google Scholar] [CrossRef] [PubMed]
- Kim, M.; Kim, B.; Choi, Y.J.; Lee, H.J.; Lee, H.; Park, J.B.; Lee, S.P.; Han, K.D.; Kim, Y.J.; Kim, H.K. Sex differences in the prognosis of patients with hypertrophic cardiomyopathy. Sci. Rep. 2021, 11, 4854. [Google Scholar] [CrossRef]
- Kubo, T.; Kitaoka, H.; Okawa, M.; Hirota, T.; Hayato, K.; Yamasaki, N.; Matsumura, Y.; Yabe, T.; Doi, Y.L. Gender-specific differences in the clinical features of hypertrophic cardiomyopathy in a community-based Japanese population: Results from Kochi RYOMA study. J. Cardiol. 2010, 56, 314–319. [Google Scholar] [CrossRef]
- Preveden, A.; Golubovic, M.; Bjelobrk, M.; Miljkovic, T.; Ilic, A.; Stojsic, S.; Gajic, D.; Glavaski, M.; Maier, L.S.; Okwose, N.; et al. Gender Related Differences in the Clinical Presentation of Hypertrophic Cardiomyopathy-An Analysis from the SILICOFCM Database. Medicina 2022, 58, 314. [Google Scholar] [CrossRef] [PubMed]
- Rowin, E.J.; Maron, M.S.; Wells, S.; Patel, P.P.; Koethe, B.C.; Maron, B.J. Impact of Sex on Clinical Course and Survival in the Contemporary Treatment Era for Hypertrophic Cardiomyopathy. J. Am. Heart Assoc. 2019, 8, e012041. [Google Scholar] [CrossRef]
- Ommen, S.R.; Mital, S.; Burke, M.A.; Day, S.M.; Deswal, A.; Elliott, P.; Evanovich, L.L.; Hung, J.; Joglar, J.A.; Kantor, P.; et al. 2020 AHA/ACC Guideline for the Diagnosis and Treatment of Patients With Hypertrophic Cardiomyopathy: Executive Summary: A Report of the American College of Cardiology/American Heart Association Joint Committee on Clinical Practice Guidelines. Circulation 2020, 142, e533–e557. [Google Scholar]
- Elliott, P.M.; Anastasakis, A.; Borger, M.A.; Borggrefe, M.; Cecchi, F.; Charron, P.; Hagege, A.A.; Lafont, A.; Limongelli, G.; Mahrholdt, H.; et al. 2014 ESC Guidelines on diagnosis and management of hypertrophic cardiomyopathy: The Task Force for the Diagnosis and Management of Hypertrophic Cardiomyopathy of the European Society of Cardiology (ESC). Eur. Heart J. 2014, 35, 2733–2779. [Google Scholar]
- Spirito, P.; Rossi, J.; Maron, B.J. Alcohol septal ablation: In which patients and why? Ann. Cardiothorac. Surg. 2017, 6, 369–375. [Google Scholar] [CrossRef] [PubMed]
- Affronti, A.; Pruna-Guillen, R.; Sandoval, E.; Pereda, D.; Alcocer, J.; Castellà, M.; Quintana, E. Surgery for Hypertrophic Obstructive Cardiomyopathy: Comprehensive LVOT Management beyond Septal Myectomy. J. Clin. Med. 2021, 10, 4397. [Google Scholar] [CrossRef]
- Embozene™ Color-Advanced Microspheres. Available online: https://www.bostonscientific.com/content/dam/Manuals/bz/current-rev-pt/50913186-01A_Embozene_eDFU_bz_s.pdf (accessed on 20 February 2023).
- Dickmann, B.; Baars, T.; Heusch, G.; Erbel, R. Transcoronary septal ablation in hypertrophic obstructive cardiomyopathy by embolizing microspheres. Eur. Heart J. 2013, 34, 2489. [Google Scholar] [CrossRef]
- Bandyopadhyay, D.; Chakraborty, S.; Amgai, B.; Kapadia, S.R.; Braunwald, E.; Naidu, S.S.; Kalra, A. Association of Hypertrophic Obstructive Cardiomyopathy With Outcomes Following Transcatheter Aortic Valve Replacement. JAMA Netw. Open 2020, 3, e1921669. [Google Scholar] [CrossRef]
- Desai, M.Y.; Alashi, A.; Popovic, Z.B.; Wierup, P.; Griffin, B.P.; Thamilarasan, M.; Johnston, D.; Svensson, L.G.; Lever, H.M.; Smedira, N.G. Outcomes in Patients With Obstructive Hypertrophic Cardiomyopathy and Concomitant Aortic Stenosis Undergoing Surgical Myectomy and Aortic Valve Replacement. J. Am. Heart Assoc. 2021, 10, e018435. [Google Scholar] [CrossRef] [PubMed]
- Lakdawala, N.K.; Olivotto, I.; Day, S.M.; Han, L.; Ashley, E.A.; Michels, M.; Ingles, J.; Semsarian, C.; Jacoby, D.; Jefferies, J.L.; et al. Associations Between Female Sex, Sarcomere Variants, and Clinical Outcomes in Hypertrophic Cardiomyopathy. Circ. Genom. Precis. Med. 2021, 14, e003062. [Google Scholar] [CrossRef]
- Gimeno, J.R.; Tomé-Esteban, M.; Lofiego, C.; Hurtado, J.; Pantazis, A.; Mist, B.; Lambiase, P.; McKenna, W.J.; Elliott, P.M. Exercise-induced ventricular arrhythmias and risk of sudden cardiac death in patients with hypertrophic cardiomyopathy. Eur. Heart J. 2009, 30, 2599–2605. [Google Scholar] [CrossRef] [PubMed]
- McLeod, C.J.; Ackerman, M.J.; Nishimura, R.A.; Tajik, A.J.; Gersh, B.J.; Ommen, S.R. Outcome of patients with hypertrophic cardiomyopathy and a normal electrocardiogram. J. Am. Coll. Cardiol. 2009, 54, 229–233. [Google Scholar] [CrossRef]
- Varnava, A.M.; Elliott, P.M.; Sharma, S.; McKenna, W.J.; Davies, M.J. Hypertrophic cardiomyopathy: The interrelation of disarray, fibrosis, and small vessel disease. Heart 2000, 84, 476–482. [Google Scholar] [CrossRef]
- Yang, H.; Woo, A.; Monakier, D.; Jamorski, M.; Fedwick, K.; Wigle, E.D.; Rakowski, H. Enlarged left atrial volume in hypertrophic cardiomyopathy: A marker for disease severity. J. Am. Soc. Echocardiogr. 2005, 18, 1074–1082. [Google Scholar] [CrossRef] [PubMed]
- Mahmod, M.; Raman, B.; Chan, K.; Sivalokanathan, S.; Smillie, R.W.; Samat, A.H.A.; Ariga, R.; Dass, S.; Ormondroyd, E.; Watkins, H.; et al. Right ventricular function declines prior to left ventricular ejection fraction in hypertrophic cardiomyopathy. J. Cardiovasc. Magn. Reson. 2022, 24, 36. [Google Scholar] [CrossRef] [PubMed]
- Butters, A.; Lakdawala, N.K.; Ingles, J. Sex Differences in Hypertrophic Cardiomyopathy: Interaction With Genetics and Environment. Curr. Heart Fail. Rep. 2021, 18, 264–273. [Google Scholar] [CrossRef] [PubMed]
- Lawrenz, T.; Lieder, F.; Bartelsmeier, M.; Leuner, C.; Borchert, B.; Meyer zu Vilsendorf, D.; Strunk-Mueller, C.; Reinhardt, J.; Feuchtl, A.; Stellbrink, C.; et al. Predictors of complete heart block after transcoronary ablation of septal hypertrophy: Results of a prospective electrophysiological investigation in 172 patients with hypertrophic obstructive cardiomyopathy. J. Am. Coll. Cardiol. 2007, 49, 2356–2363. [Google Scholar] [CrossRef]
- Vriesendorp, P.A.; Van Mieghem, N.M.; Vletter, W.B.; Ten Cate, F.J.; de Jong, P.L.; Schinkel, A.F.; Michels, M. Microsphere embolisation as an alternative for alcohol in percutaneous transluminal septal myocardial ablation. Neth. Heart J. 2013, 21, 245–248. [Google Scholar] [CrossRef] [PubMed]
- Nguyen, A.; Schaff, H.V.; Hang, D.; Nishimura, R.A.; Geske, J.B.; Dearani, J.A.; Lahr, B.D.; Ommen, S.R. Surgical myectomy versus alcohol septal ablation for obstructive hypertrophic cardiomyopathy: A propensity score-matched cohort. J. Thorac. Cardiovasc. Surg. 2019, 157, 306–315.e3. [Google Scholar] [CrossRef] [PubMed]
- Nguyen, A.; Schaff, H.V.; Hang, D.; Nishimura, R.A.; Geske, J.B.; Dearani, J.A.; Lahr, B.D.; Ommen, S.R. Long-term clinical outcome after alcohol septal ablation for obstructive hypertrophic cardiomyopathy: Results from the Euro-ASA registry. Eur. Heart J. 2016, 37, 1517–1523. [Google Scholar]
- Sawaya, F.J.; Louvard, Y.; Spaziano, M.; Morice, M.C.; Hage, F.; El-Khoury, C.; Roy, A.; Garot, P.; Hovasse, T.; Benamer, H. Short and long-term outcomes of alcohol septal ablation with the trans-radial versus the trans-femoral approach: A single center-experience. Int. J. Cardiol. 2016, 220, 7–13. [Google Scholar] [CrossRef]
- Saberi, S.; Cardim, N.; Yamani, M.; Schulz-Menger, J.; Li, W.; Florea, V.; Sehnert, A.J.; Kwong, R.Y.; Jerosch-Herold, M.; Masri, A. Mavacamten Favorably Impacts Cardiac Structure in Obstructive Hypertrophic Cardiomyopathy: EXPLORER-HCM Cardiac Magnetic Resonance Substudy Analysis. Circulation 2021, 143, 606–608. [Google Scholar] [CrossRef]
- Marian, A.J.; Braunwald, E. Hypertrophic cardiomyopathy: Genetics, pathogenesis, clinical manifestations, diagnosis, and therapy. Circ. Res. 2017, 121, 749–770. [Google Scholar] [CrossRef] [PubMed]
- Yang, H.; Yang, Y.; Xue, Y.; Luo, S. Efficacy and safety of radiofrequency ablation for hypertrophic obstructive cardiomyopathy: A systematic review and meta-analysis. Clin. Cardiol. 2020, 43, 450–458. [Google Scholar] [CrossRef] [PubMed]

| Patient Characteristics | Overall Population n = 76 | Male n = 33 (43.4) | Female n = 43 (56.6) | p Value |
|---|---|---|---|---|
| 1. Demographics | ||||
| Age, years | 60.5 [26.0] | 54.0 [22.0] | 68.0 [21.0] | <0.001 |
| BMI, kg/m2 | 28.2 ± 4.8 | 28.6 ± 4.8 | 27.9 ± 4.9 | 0.509 |
| BSA, m2 | 1.9 ± 0.3 | 2.0 ± 0.3 | 1.8 ± 0.2 | <0.001 |
| NYHA ≥ 3, n (%) | 65 (85.5) | 25 (75.8) | 40 (93.0) | 0.049 |
| Previous syncope, n (%) | 14 (18.4) | 8 (24.2) | 6 (14.0) | 0.371 |
| Family history of SCD, n (%) | 11 (14.5) | 6 (18.2) | 5 (11.6) | 0.517 |
| Previous cardiac arrest or sustained VT, n (%) | 3 (3.9) | 2 (6.1) | 1 (2.3) | 0.576 |
| ICD, n (%) | 13 (17.1) | 8 (24.2) | 5 (11.6) | 0.219 |
| Pacemaker, n (%) | 2 (2.6) | 1 (3.0) | 1 (2.3) | 1.000 |
| CRT, n (%) | 1 (1.3) | 0 (0.0) | 1 (2.3) | 1.000 |
| 2. Comorbidities | ||||
| HTN, n (%) | 65 (85.5) | 28 (84.8) | 37 (86.0) | 1.000 |
| Diabetes mellitus, n (%) | 13 (17.1) | 5 (15.2) | 8 (18.6) | 0.766 |
| Atrial fibrillation, n (%) | 13 (17.1) | 6 (18.2) | 7 (16.3) | 1.000 |
| CAD, n (%) | 22 (28.9) | 7 (21.2) | 15 (34.9) | 0.214 |
| COPD, n (%) | 6 (7.9) | 3 (9.1) | 3 (7.0) | 1.000 |
| AV block, n (%) | 5 (6.7) | 1 (3.0) | 4 (9.3) | 0.381 |
| LAFB, n (%) | 5 (6.6) | 3 (9.1) | 2 (4.7) | 0.647 |
| LBBB, n (%) | 6 (7.9) | 2 (6.1) | 4 (9.3) | 0.692 |
| RBBB, n (%) | 6 (7.9) | 5 (15.2) | 1 (2.3) | 0.080 |
| nsVT, n (%) | 8 (10.5) | 3 (9.1) | 5 (11.6) | 1.000 |
| 3. Echocardiography | ||||
| LVEF, % | 61 [11.0] | 63 [14.0] | 60 [8.0] | 0.113 |
| LVOT gradient at rest, mmHg | 41.0 [27.0] | 40.0 [28.0] | 42.0 [32.0] | 0.560 |
| LVOT gradient (Valsalva), mmHg | 95.0 [71.0] | 95.0 [75.0] | 85.0 [60.0] | 0.208 |
| SAM, n (%) | 62 (81.6) | 29 (87.9) | 33 (76.7) | 0.248 |
| MR ≥ 2 grade, n (%) | 35 (46.1) | 16 (48.5) | 19 (44.2) | 0.817 |
| LA diameter/m2, mm | 22.0 [4.6] | 21.5 [4.7] | 23.7 [5.3] | 0.040 |
| LAVI/m2, mL | 38.9 [20.0] | 34.8 [4.7] | 40.1 [20.5] | 0.283 |
| TAPSE, mm | 19 [4.0] | 21 [5.0] | 19 [3.0] | 0.009 |
| sPAP > 35 mmHg, n (%) | 22 (28.9) | 9 (27.3) | 13 (30.2) | 0.805 |
| 4. Laboratory results | ||||
| NTproBNP, pg/mL | 388.0 [737.0] | 318.0 [562.0] | 430.7 [1142.0] | 0.099 |
| Creatinine, mg/dL | 1.1 [0.2] | 1.1 [0.3] | 1.1 [0.2] | 0.146 |
| CK, U/L | 75.0 [53.5] | 77.0 [33.0] | 69.0 [67.0] | 0.052 |
| TroponinI, ng/L | 20.0 [30.0] | 20.0 [48.5] | 20.0 [30.0] | 0.577 |
| Medical treatment | ||||
| Betablockers, n (%) | 62 (81.6) | 29 (87.9) | 33 (76.7) | 0.248 |
| Verapamil, n (%) | 16 (21.1) | 6 (18.2) | 10 (23.3) | 0.778 |
| Diltiazem, n (%) | 1 (1.3) | 1 (3.1) | 0 (0.0) | 0.427 |
| Diuretics, n (%) | 45 (59.2) | 12 (36.4) | 33 (76.7) | <0.001 |
| NOACs, n (%) | 4 (5.3) | 2 (6.1) | 2 (4.7) | 1.000 |
| Vitamin K antagonists, n (%) | 8 (10.5) | 4 (12.1) | 4 (9.3) | 0.721 |
| Antiplatelet agents, n (%) | 42 (55.3) | 17 (51.5) | 25 (58.1) | 0.644 |
| Peri- and Postprocedural Outcomes | Overall Population n = 76 | Male n = 33 | Female n = 43 | p Value |
|---|---|---|---|---|
| Volume of microspheres, mL | 2.0 [2.0] | 3.0 [3.0] | 2.0 [2.0] | 0.306 |
| ICU stay, days | 1.0 [0.0] | 1.0 [0.0] | 1.0 [1.0] | 0.133 |
| Hospitalisation, days | 12.5 [10.0] | 12.0 [8.0] | 13.0 [11.0] | 0.449 |
| CK max, U/L | 926.0 [949.0] | 1018.0 [1537.0] | 897 [947.0] | 0.234 |
| Troponin I, ng/L | 2485.0 [2874.0] | 2311.0 [2908.0] | 2659.0 [2889.0] | 0.506 |
| Complications | ||||
| AV block, n (%) | 5 (6.6) | 2 (6.1) | 3 (7.0) | 1.000 |
| New LBBB, n (<%) | 1 (1.3) | 0 (0.0) | 1 (2.3) | 1.000 |
| New RBBB, n (%) | 3 (3.9) | 1 (3.0) | 2 (4.7) | 1.000 |
| Access site complications, n (%) | 4 (5.3) | 2 (6.1) | 2 (4.7) | 1.000 |
| Postprocedural death, n (%) | 1 (1.3) | 1 (3.0) | 0 (0.0) | 0.434 |
| Characteristics | Males (n = 33) | Females (n = 43) | Males vs. Females | ||||
|---|---|---|---|---|---|---|---|
| Pre-TASH | Post-TASH | p Value | Pre-TASH | Post-TASH | p Value | p Value for Δ | |
| LVOT gradient at rest, mmHg | 40 [22.0] | 16.0 [14.0] | <0.001 | 42.0 [32.0] | 15.0 [17.0] | <0.001 | 0.147 |
| Provoked LVOT gradient, mmHg | 95.0 [75.0] | 25.0 [41.0] | <0.001 | 85.0 [60.0] | 24.0 [42.0] | <0.001 | 0.709 |
| NT-proBNP, pg/mL | 318.0 [562.0] | 189.0 [367.0] | 0.073 | 430.7 [1142.0] | 281.0 [408.0] | 0.009 | 0.338 |
| NYHA ≥ 3, n (%) | 25 (75.8) | 1 (3.0) | <0.001 | 40 (93.0) | 2 (4.7) | <0.001 | 0.636 |
| IVSd > 20 mm, n (%) | 16 (48.5) | 4 (12.1) | <0.001 | 21 (48.8) | 3 (7.0) | <0.001 | 0.583 |
| Characteristics | HR | 95% CI | p Value |
|---|---|---|---|
| Age at TASH, years | 1.035 | 1.007–1.063 | 0.015 |
| NYHA ≥ 3 | 1.256 | 0.359–4.395 | 0.722 |
| Female sex | 0.940 | 0.376–2.350 | 0.895 |
| TAPSE, mm | 1.921 | 0.802–1.057 | 0.240 |
| Diuretics | 1.703 | 0.707–4.101 | 0.235 |
| LA diameter, mm | 1.007 | 0.974–1.040 | 0.697 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Alyaydin, E.; Vogel, J.K.; Luedike, P.; Rassaf, T.; Jánosi, R.A.; Papathanasiou, M. Sex-Related Differences among Adults with Hypertrophic Obstructive Cardiomyopathy Undergoing Transcoronary Ablation of Septal Hypertrophy. J. Clin. Med. 2023, 12, 3024. https://doi.org/10.3390/jcm12083024
Alyaydin E, Vogel JK, Luedike P, Rassaf T, Jánosi RA, Papathanasiou M. Sex-Related Differences among Adults with Hypertrophic Obstructive Cardiomyopathy Undergoing Transcoronary Ablation of Septal Hypertrophy. Journal of Clinical Medicine. 2023; 12(8):3024. https://doi.org/10.3390/jcm12083024
Chicago/Turabian StyleAlyaydin, Emyal, Julia Kirsten Vogel, Peter Luedike, Tienush Rassaf, Rolf Alexander Jánosi, and Maria Papathanasiou. 2023. "Sex-Related Differences among Adults with Hypertrophic Obstructive Cardiomyopathy Undergoing Transcoronary Ablation of Septal Hypertrophy" Journal of Clinical Medicine 12, no. 8: 3024. https://doi.org/10.3390/jcm12083024
APA StyleAlyaydin, E., Vogel, J. K., Luedike, P., Rassaf, T., Jánosi, R. A., & Papathanasiou, M. (2023). Sex-Related Differences among Adults with Hypertrophic Obstructive Cardiomyopathy Undergoing Transcoronary Ablation of Septal Hypertrophy. Journal of Clinical Medicine, 12(8), 3024. https://doi.org/10.3390/jcm12083024