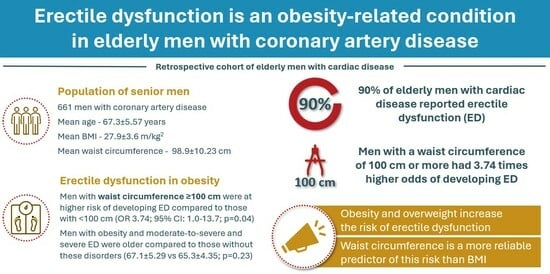
Erectile Dysfunction as an Obesity-Related Condition in Elderly Men with Coronary Artery Disease
Abstract
:1. Introduction
2. Materials and Methods
3. Results
3.1. Characteristics of the Study Group
3.2. Association between BMI and ED
3.3. Association between Waist Circumference and ED
3.4. Characteristics of Obese Men with ED
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Temple, N.J. The Origins of the Obesity Epidemic in the USA-Lessons for Today. Nutrients 2022, 14, 4253. [Google Scholar] [CrossRef] [PubMed]
- Obesity. World Health Organization (WHO). Available online: https://www.who.int/health-topics/obesity (accessed on 25 September 2023).
- Dai, H.; Alsalhe, T.A.; Chalghaf, N.; Riccò, M.; Bragazzi, N.L.; Wu, J. The global burden of disease attributable to high body mass index in 195 countries and territories, 1990-2017: An analysis of the Global Burden of Disease Study. PLoS Med. 2020, 17, e1003198. [Google Scholar] [CrossRef] [PubMed]
- Plackett, B. The vicious cycle of depression and obesity. Nature 2022, 608, S42–S43. [Google Scholar] [CrossRef] [PubMed]
- Cawley, J.; Biener, A.; Meyerhoefer, C.; Ding, Y.; Zvenyach, T.; Smolarz, B.G.; Ramasamy, A. Job Absenteeism Costs of Obesity in the United States: National and State-Level Estimates. J. Occup. Environ. Med. 2021, 63, 565–573. [Google Scholar] [CrossRef] [PubMed]
- Hecker, J.; Freijer, K.; Hiligsmann, M.; Evers, S. Burden of disease study of overweight and obesity; the societal impact in terms of cost-of-illness and health-related quality of life. BMC Public Health 2022, 22, 46. [Google Scholar] [CrossRef] [PubMed]
- What Is the Body Mass Index (BMI)? National Health Servise (NHS). Available online: https://www.nhs.uk/common-health-questions/lifestyle/what-is-the-body-mass-index-bmi/ (accessed on 25 September 2023).
- Powell-Wiley, T.M.; Poirier, P.; Burke, L.E.; Després, J.P.; Gordon-Larsen, P.; Lavie, C.J.; Lear, S.A.; Ndumele, C.E.; Neeland, I.J.; Sanders, P.; et al. Obesity and Cardiovascular Disease: A Scientific Statement From the American Heart Association. Circulation 2021, 143, e984–e1010. [Google Scholar] [CrossRef] [PubMed]
- Kałka, D.; Domagała, Z.; Rakowska, A.; Womperski, K.; Franke, R.; Sylwina-Krauz, E.; Stanisz, J.; Piłot, M.; Gebala, J.; Rusiecki, L.; et al. Modifiable risk factors for erectile dysfunction: An assessment of the awareness of such factors in patients suffering from ischaemic heart disease. Int. J. Impot. Res. 2016, 28, 14–19. [Google Scholar] [CrossRef] [PubMed]
- Pizzol, D.; Smith, L.; Fontana, L.; Caruso, M.G.; Bertoldo, A.; Demurtas, J.; McDermott, D.; Garolla, A.; Grabovac, I.; Veronese, N. Associations between body mass index, waist circumference and erectile dysfunction: A systematic review and META-analysis. Rev. Endocr. Metab. Disord. 2020, 21, 657–666. [Google Scholar] [CrossRef] [PubMed]
- Li, H.; Xu, W.; Wang, T.; Wang, S.; Liu, J.; Jiang, H. Effect of weight loss on erectile function in men with overweight or obesity: A meta-analysis of randomised controlled trials. Andrologia 2022, 54, e14250. [Google Scholar] [CrossRef]
- Rey, R.A.; Grinspon, R.P.; Gottlieb, S.; Pasqualini, T.; Knoblovits, P.; Aszpis, S.; Pacenza, N.; Stewart Usher, J.; Bergadá, I.; Campo, S.M. Male hypogonadism: An extended classification based on a developmental, endocrine physiology-based approach. Andrology 2013, 1, 3–16. [Google Scholar] [CrossRef]
- Kałka, D.; Biernikiewicz, M.; Gebala, J.; Sobieszczańska, M.; Jakima, S.; Pilecki, W.; Rusiecki, L. Diagnosis of hypogonadism in patients treated with low energy shock wave therapy for erectile dysfunction: A narrative review. Transl. Androl. Urol. 2020, 9, 2786–2796. [Google Scholar] [CrossRef] [PubMed]
- Wu, F.C.; Tajar, A.; Pye, S.R.; Silman, A.J.; Finn, J.D.; O’Neill, T.W.; Bartfai, G.; Casanueva, F.; Forti, G.; Giwercman, A.; et al. Hypothalamic-pituitary-testicular axis disruptions in older men are differentially linked to age and modifiable risk factors: The European Male Aging Study. J. Clin. Endocrinol. Metab. 2008, 93, 2737–2745. [Google Scholar] [CrossRef]
- Kelly, D.M.; Jones, T.H. Testosterone and obesity. Obes. Rev. 2015, 16, 581–606. [Google Scholar] [CrossRef] [PubMed]
- Cohen, P.G. The hypogonadal–obesity cycle: Role of aromatase in modulating the testosterone–estradiol shunt—A major factor in the genesis of morbid obesity. Med. Hypotheses 1999, 52, 49–51. [Google Scholar] [CrossRef]
- Drygas, W.; Kostka, T.; Jegier, A.; Kuński, H. Long-term effects of different physical activity levels on coronary heart disease risk factors in middle-aged men. Int. J. Sports Med. 2000, 21, 235–241. [Google Scholar] [CrossRef]
- Arsenault, B.J.; Rana, J.S.; Lemieux, I.; Després, J.P.; Wareham, N.J.; Kastelein, J.J.; Boekholdt, S.M.; Khaw, K.T. Physical activity, the Framingham risk score and risk of coronary heart disease in men and women of the EPIC-Norfolk study. Atherosclerosis 2010, 209, 261–265. [Google Scholar] [CrossRef] [PubMed]
- Rosen, R.C.; Cappelleri, J.C.; Smith, M.D.; Lipsky, J.; Peña, B.M. Development and evaluation of an abridged, 5-item version of the International Index of Erectile Function (IIEF-5) as a diagnostic tool for erectile dysfunction. Int. J. Impot. Res. 1999, 11, 319–326. [Google Scholar] [CrossRef]
- World Population Ageing 2019. United Nations: Department of Economic and Social Affairs. Available online: https://www.un.org/en/development/desa/population/publications/pdf/ageing/WorldPopulationAgeing2019-Report.pdf (accessed on 15 November 2023).
- Salonia, A.; Bettocchi, C.; Capogrosso, P.; Carvalho, J.; Corona, G.; Hatzichristodoulou, G.; Jones, T.H.; Kadioglu, A.; Martinez-Salamanca, J.I.; Minhas, S.; et al. EAU Guidelines on Sexual and Reproductive Health. European Association of Urology. Available online: https://d56bochluxqnz.cloudfront.net/documents/full-guideline/EAU-Guidelines-on-Sexual-and-Reproductive-Health-2023.pdf (accessed on 25 October 2023).
- Cho, Y.G.; Song, H.J.; Lee, S.K.; Jang, S.N.; Jeong, J.Y.; Choi, Y.H.; Hong, K.S.; Choi, M.G.; Kang, S.H.; Kang, J.H.; et al. The relationship between body fat mass and erectile dysfunction in Korean men: Hallym Aging Study. Int. J. Impot. Res. 2009, 21, 179–186. [Google Scholar] [CrossRef]
- Waist Circumference and Waist-Hip Ratio—Report of a WHO Expert Consultation. World Health Organization. Available online: https://iris.who.int/bitstream/handle/10665/44583/9789241501491_eng.pdf?sequence=1 (accessed on 26 March 2024).
- Balkau, B.; Charles, M.A. Comment on the provisional report from the WHO consultation. European Group for the Study of Insulin Resistance (EGIR). Diabet. Med. 1999, 16, 442–443. [Google Scholar] [CrossRef]
- Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults. Executive Summary of the Third Report of the National Cholesterol Education Program (NCEP) Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults (Adult Treatment Panel III). JAMA 2001, 285, 2486–2497. [Google Scholar] [CrossRef]
- Cao, S.; Hu, X.; Shao, Y.; Wang, Y.; Tang, Y.; Ren, S.; Li, X. Relationship between weight-adjusted-waist index and erectile dysfunction in the United State: Results from NHANES 2001–2004. Front. Endocrinol. 2023, 14, 1128076. [Google Scholar] [CrossRef]
- Kessler, A.; Sollie, S.; Challacombe, B.; Briggs, K.; Van Hemelrijck, M. The global prevalence of erectile dysfunction: A review. BJU Int. 2019, 124, 587–599. [Google Scholar] [CrossRef] [PubMed]
- Ross, R.; Neeland, I.J.; Yamashita, S.; Shai, I.; Seidell, J.; Magni, P.; Santos, R.D.; Arsenault, B.; Cuevas, A.; Hu, F.B.; et al. Waist circumference as a vital sign in clinical practice: A Consensus Statement from the IAS and ICCR Working Group on Visceral Obesity. Nat. Rev. Endocrinol. 2020, 16, 177–189. [Google Scholar] [CrossRef] [PubMed]
- Buch, A.; Marcus, Y.; Shefer, G.; Zimmet, P.; Stern, N. Approach to Obesity in the Older Population. J. Clin. Endocrinol. Metab. 2021, 106, 2788–2805. [Google Scholar] [CrossRef]
- McKee, A.M.; Morley, J.E. Obesity in the Elderly. Available online: https://www.ncbi.nlm.nih.gov/books/NBK532533/ (accessed on 29 February 2024).
- Al-Hunayan, A.; Al-Mutar, M.; Kehinde, E.O.; Thalib, L.; Al-Ghorory, M. The prevalence and predictors of erectile dysfunction in men with newly diagnosed with type 2 diabetes mellitus. BJU Int. 2007, 99, 130–134. [Google Scholar] [CrossRef] [PubMed]
- Traish, A.M.; Feeley, R.J.; Guay, A. Mechanisms of obesity and related pathologies: Androgen deficiency and endothelial dysfunction may be the link between obesity and erectile dysfunction. FEBS J. 2009, 276, 5755–5767. [Google Scholar] [CrossRef] [PubMed]
- Kałka, D.; Karpiński, Ł.; Gebala, J.; Rusiecki, L.; Biełous-Wilk, A.; Krauz, E.S.; Piłot, M.; Womperski, K.; Rusiecka, M.; Pilecki, W. Sexual health of male cardiac patients—Present status and expectations of patients with coronary heart disease. Arch. Med. Sci. 2017, 13, 302–310. [Google Scholar] [CrossRef] [PubMed]
- Yassin, A.A.; Nettleship, J.E.; Salman, M.; Almehmadi, Y. Waist circumference is superior to weight and BMI in predicting sexual symptoms, voiding symptoms and psychosomatic symptoms in men with hypogonadism and erectile dysfunction. Andrologia 2017, 49, e12634. [Google Scholar] [CrossRef]


| Variable | Total | 18.5 ≤ BMI < 25 | 25≤ BMI < 30 | BMI ≥ 30 | p Value |
|---|---|---|---|---|---|
| No of patients, n (%) | 661 | 143 (21.6%) | 344 (52.0%) | 174 (26.3%) | |
| Age, years | |||||
| Mean ± SD | 67.3 ± 5.57 | 68.7 ± 5.52 | 67.1 ± 5.20 | 67.6 ± 5.26 | 0.32 |
| Median | 66.0 | 67.0 | 66.0 | 66.00 | |
| IQR | 63.0–71.0 | 64.0–73.0 | 63.0–70.0 | 62.0–70.0 | |
| Range | 60.0–90.0 | 60.0–90.0 | 60.0–85.0 | 60.0–84.0 | |
| Education, n (%) | |||||
| Higher | 127 (19.2%) | 118 (19.6%) | 68 (19.8%) | 31 (17.8% | 0.05 |
| Secondary | 211 (31.9%) | 46 (32.2%) | 120 (34.9%) | 45 (25.9%) | |
| Vocational | 191 (28.9%) | 32 (22.4%) | 96 (27.9%) | 63 (36.2%) | |
| Primary | 46 (7.0%) | 12 (8.4%) | 17 (4.9%) | 17 (9.8%) | |
| Missing data | 86 (13.0) | 25 (17.5%) | 43 (12.5%) | 18(10.3%) | |
| Erectile dysfunction *, n (%) | |||||
| Severe | 142 (21.5%) | 29 (20.3%) | 75 (21.8%) | 38 (21.8%) | 0.96 |
| Moderate-to-severe | 95 (14.4%) | 21 (14.7%) | 44 (12.8%) | 30 (17.2%) | |
| Moderate | 208 (31.5%) | 46 (32.2%) | 112 (32.6%) | 50 (28.7%) | |
| Mild | 154 (23.3%) | 34 (23.8%) | 81 (23.5%) | 39 (22.4%) | |
| No dysfunction | 62 (9.4%) | 13 (9.1%) | 32 (9.3%) | 17 (9.8%) | |
| Hypertension, n (%) | |||||
| Yes | 382 (57.8%) | 66 (46.2%) | 194 (56.4%) | 122 (70.1%) | 0.004 |
| No | 89 (13.5%) | 29 (20.3%) | 39 (11.3%) | 21 (12.1%) | |
| Missing data | 190 (28.7%) | 48 (33.6%) | 111 (32.3%) | 31 (17.8%) | |
| Type 2 diabetes, n (%) | |||||
| Yes | 157 (23.8%) | 21 (14.7%) | 75 (21.8%) | 61 (35.1%) | 0.003 |
| No | 281 (42.5%) | 68 (47.6%) | 141 (41.0%) | 72(41.4%) | |
| Missing data | 223 (33.7%) | 54 (37.8%) | 128 (37.2%) | 41 (23.6%) | |
| Dyslipidemia, n (%) | |||||
| Yes | 273 (41.3%) | 58 (40.6%) | 125 (36.3%) | 90 (51.7%) | 0.15 |
| No | 165 (25.0%) | 31 (21.7%) | 91 (26.5%) | 43 (24.7%) | |
| Missing data | 223 33.7%) | 54 (37.8%) | 128 (37.2%) | 41 (23.6%) | |
| Smoking, n (%) | |||||
| Yes | 336 (50.8%) | 69 (48.3%) | 165 (48.0%) | 102 (58.6%) | 0.97 |
| No | 103 (15.6%) | 20 (14.0%) | 51 (14.8%) | 32 (18.4%) | |
| Missing data | 222 (33.6%) | 54 (37.8%) | 128 (37.2%) | 40 (23.0%) | |
| Sedentary lifestyle ** | |||||
| Yes | 539 (81.5%) | 115 (80.4%) | 280 (81.45%) | 144 (82.8%) | 0.81 |
| No | 85 (12.9%) | 19 (13.3%) | 41 (11.9%) | 25 (14.4%0 | |
| Missing data | 37 (5.6%) | 9 (6.3%) | 23 (6.7%) | 5 (2.9%) | |
| Waist circumference | |||||
| Mean ± SD | 98.9 ± 10.23 | 92.1 ± 8.60 | 97.6 ± 7.83 | 107.0 ± 10.42 | <0.001 |
| Median | 98.0 | 90.0 | 97.0 | 105.0 | |
| IQR | 92.0–104.0 | 86.0–98.0 | 93.0–102.0 | 100.0–104.0 | |
| Range | 70.0–160.0 | 70.0–116.0 | 76.0–160.0 | 85.0–154.0 | |
| 18.5 ≤ BMI < 25 | 25 ≤ BMI < 30 | BMI ≥ 30 | |
|---|---|---|---|
| Moderate-to-severe ED | 96 (67.1%) | 231 (67.2%) | 118 (67.8%) |
| No ED and mild ED | 47 (32.9%) | 113 (32.8%) | 56 (32.2%) |
| WC Q1 | WC Q2 | WC Q3 | WC Q4 | |
|---|---|---|---|---|
| Moderate-to-severe ED | 89 (69.5%) | 96 (64.4%) | 117 (66.1%) | 141 (75.8%) |
| No ED and mild ED | 58 (39.5%) | 53 (35.6%) | 60 (33.9%) | 45 (24.2%) |
| Variable | Normal Weight, No ED (BMI < 25 and IIEF-5 * > 21) | Obesity, Overweight, ED (BMI ≥ 25 and IIEF-5 * ≤ 21) | p Value |
|---|---|---|---|
| Number of patients, n | 13 (2.7%) | 469 (97.3%) | |
| Age, years | |||
| Mean ± SD | 65.3 ± 4.35 | 67.1 ± 5.29 | 0.23 |
| Median (IQR) | 65.0 (62.0–67.0) | 66.0 (63.0–70.0) | |
| Range | 60.0–75.0 | 60.0–84.0 | |
| Education, n (%) | |||
| Higher | 3 (25.0%) | 81 (19.8%) | 0.77 |
| Secondary | 5 (41.7%) | 154 (37.7%) | |
| Vocational | 4 (33.3%) | 144 (35.2%) | |
| Primary | 0 (0.0%) | 30 (7.3%) | |
| Hypertension, n (%) | |||
| Yes | 9 (90.0%) | 285 (96.9%) | 0.62 |
| No | 1 (22.0%) | 53 (15.7%) | |
| Type 2 diabetes, n (%) | |||
| Yes | 4 (44.4%) | 126 (40.3%) | 0.80 |
| No | 5 (55.6%) | 187 (97.4%) | |
| Dyslipidemia, n (%) | |||
| Yes | 6 (66.7%) | 192 (61.3%) | 0.75 |
| No | 3 (33.3%) | 121 (38.7%) | |
| Smoking, n (%) | |||
| Yes | 6 (66.7%) | 243 (77.4%) | 0.45 |
| No | 3 (33.3%) | 71 (22.6%) | |
| Sedentary lifestyle ** | |||
| Yes | 9 (75.00%) | 381 (86.2%) | 0.27 |
| No | 3 (25.00%) | 61 (13.8%) | |
| Waist circumference | |||
| Mean ± SD | 91.6 ± 8.88 | 101.1 ± 9.91 | <0.001 |
| Median (IQR) | 89.0 (86.0–95.0) | 100.0 (95.0–105.0) | |
| Range | 83.0–112.0 | 76.0–160.0 | |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Biernikiewicz, M.; Sobieszczańska, M.; Szuster, E.; Pawlikowska-Gorzelańczyk, A.; Janocha, A.; Rożek-Piechura, K.; Rusiecka, A.; Gebala, J.; Okrzymowska, P.; Kałka, D. Erectile Dysfunction as an Obesity-Related Condition in Elderly Men with Coronary Artery Disease. J. Clin. Med. 2024, 13, 2087. https://doi.org/10.3390/jcm13072087
Biernikiewicz M, Sobieszczańska M, Szuster E, Pawlikowska-Gorzelańczyk A, Janocha A, Rożek-Piechura K, Rusiecka A, Gebala J, Okrzymowska P, Kałka D. Erectile Dysfunction as an Obesity-Related Condition in Elderly Men with Coronary Artery Disease. Journal of Clinical Medicine. 2024; 13(7):2087. https://doi.org/10.3390/jcm13072087
Chicago/Turabian StyleBiernikiewicz, Małgorzata, Małgorzata Sobieszczańska, Ewa Szuster, Anna Pawlikowska-Gorzelańczyk, Anna Janocha, Krystyna Rożek-Piechura, Agnieszka Rusiecka, Jana Gebala, Paulina Okrzymowska, and Dariusz Kałka. 2024. "Erectile Dysfunction as an Obesity-Related Condition in Elderly Men with Coronary Artery Disease" Journal of Clinical Medicine 13, no. 7: 2087. https://doi.org/10.3390/jcm13072087
APA StyleBiernikiewicz, M., Sobieszczańska, M., Szuster, E., Pawlikowska-Gorzelańczyk, A., Janocha, A., Rożek-Piechura, K., Rusiecka, A., Gebala, J., Okrzymowska, P., & Kałka, D. (2024). Erectile Dysfunction as an Obesity-Related Condition in Elderly Men with Coronary Artery Disease. Journal of Clinical Medicine, 13(7), 2087. https://doi.org/10.3390/jcm13072087