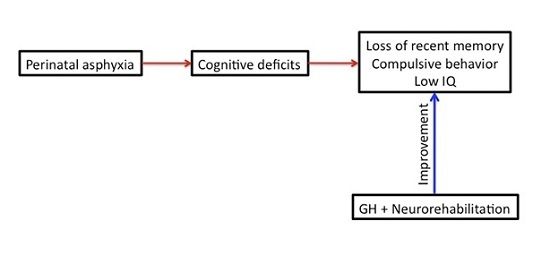
Learning and Memory Recoveries in a Young Girl Treated with Growth Hormone and Neurorehabilitation
Abstract
:1. Introduction
2. Experimental Section
2.1. Patient
2.2. Treatments
3. Results
3.1. Clinical Assessments
| WISC-IV | Pre- | Post- |
| VC | 13 | 18 |
| PR | 14 | 23 |
| WM | 12 | 21 |
| PS | 12 | 18 |
| IQ | 51 | 80 |
| Peabody | Pre- | Post- |
| EA | 6.0 | 8.11 |
| IQ | 55 | 75 |
| p | 0.1 | 2 |
| Boston | Pre- | Post- |
| Aphasia | 40.1 | 55 |
| WeeFIM | Pre- | Post- |
| PC | 50 | 55 |
| Mo | 35 | 35 |
| Me | 1 | 5 |
| SP | 2 | 6 |
3.2. Neurostimulation
3.3. Speech Therapy
3.4. Occupational Therapy
3.5. Auditive Stimulation

3.6. Blood Analysis
4. Discussion
5. Conclusions
Acknowledgments
Author Contributions
Conflicts of Interest
References
- Morales, P.; Bustamante, D.; Espina-Marchant, P.; Neira-Peña, A.; Gutiérrez-Hernández, M.A.; Allende-Castro, C.; Rojas-Mancilla, E. Pathophysiology of perinatal asphyxia: Can we predict and improve individual outcomes? EPMA J. 2011, 2, 211–230. [Google Scholar] [CrossRef] [PubMed]
- Kurinczuk, J.J.; White-Koning, M.; Badavi, N. Epidemiology of neonatal encephalopathy and hypoxic-ischaemic encephalopathy. Early Hum. Dev. 2010, 86, 329–338. [Google Scholar] [CrossRef] [PubMed]
- Volpe, J.J. Perinatal injury: From pathogenesis to neuroprotection. Ment. Retard. Dev. Disabil. Res. Rev. 2001, 7, 56–64. [Google Scholar] [CrossRef]
- Handel, M.; Swaab, H.; Vries, L.S.; Jongmans, M.J. Long-term cognitive and behavioral consequences of neonatal encephalopathy following perinatal asphyxia: A review. Eur. J. Pediatr. 2007, 166, 645–654. [Google Scholar] [CrossRef] [PubMed]
- Bjorkman, S.T.; Miller, S.M.; Rose, S.E.; Burke, C.; Colditz, P.B. Seizures are associated with brain injury severity in a neonatal model of hypoxia-ischemia. Neuroscience 2010, 166, 157–167. [Google Scholar] [CrossRef] [PubMed]
- Maneru, C.; Junque, C.; Salgado-Pineda, P.; Serra-Grabulosa, J.M.; Bartrés-Faz, D.; Ramirez-Ruiz, B.; Bargalló, N.; Tallada, M.; Botet, F. Corpus callossum atrophy in adolescents with antecedents of moderate perinatal asphyxia. Brain Inj. 2003, 17, 1003–1009. [Google Scholar] [CrossRef] [PubMed]
- Maneru, C.; Junque, C.; Botet, F.; Tallada, M.; Guardia, J. Neuropsychological long-term sequelae of perinatal asphyxia. Brain Inj. 2001, 15, 1029–1039. [Google Scholar] [CrossRef] [PubMed]
- Odd, D.E.; Lewis, G.; Whitelaw, A.; Gunnell, D. Resuscitation at birth and cognition at 8 years of age: A cohort study. Lancet 2009, 373, 1615–1622. [Google Scholar] [CrossRef]
- Basovich, S.N. The role of hypoxia in mental development and in the treatment of mental disorders: A review. Biosci. Trends 2010, 4, 288–296. [Google Scholar] [PubMed]
- Cannon, T.D.; Yolken, R.; Buka, S.; Torrey, E.F. Decreased neurotrophic response to birth hypoxia in the etiology of schizophrenia. Biol. Psychiatry 2008, 64, 797–802. [Google Scholar] [CrossRef] [PubMed]
- Devesa, J.; Casteleiro, N.; Rodicio, C.; López, N.; Reimunde, P. Growth hormone deficiency and cerebral palsy. Ther. Clin. Risk Manag. 2010, 6, 413–418. [Google Scholar] [CrossRef] [PubMed]
- Krageloh-Mann, I.; Cans, C. Cerebral palsy update. Brain Dev. 2009, 31, 537–544. [Google Scholar] [CrossRef] [PubMed]
- Johansson, B.B. Current trends in stroke rehabilitation. A review with focus on brain plasticity. Acta Neurol. Scand. 2011, 123, 147–159. [Google Scholar] [CrossRef] [PubMed]
- Coniglio, S.J.; Stevenson, R.D.; Rogol, A.D. Apparent growth hormone deficiency in children with cerebral palsy. Dev. Med. Child Neurol. 1996, 38, 797–804. [Google Scholar] [CrossRef] [PubMed]
- Hamza, R.T.; Ismail, M.A.; Hamed, A.I. Growth hormone deficiency in children and adolescents with cerebral palsy: Relation to gross motor function and degree of spasticity. Pak. J. Biol. Sci. 2011, 14, 433–440. [Google Scholar] [CrossRef] [PubMed]
- Reimunde, P.; Rodicio, C.; López, N.; Alonso, A.; Devesa, P.; Devesa, J. Effects of recombinant growth hormone replacement and physical rehabilitation in recovery of gross motor function in children with cerebral palsy. Ther. Clin. Risk Manag. 2010, 6, 585–592. [Google Scholar] [PubMed]
- Devesa, J.; Alonso, B.; Casteleiro, N.; Couto, P.; Castañón, B.; Zas, E.; Reimunde, P. Effects of recombinant growth hormone (GH) replacement and psychomotor and cognitive stimulation in the neurodevelopment of GH-deficient (GHD) children with cerebral palsy: A pilot study. Ther. Clin. Risk Manag. 2011, 7, 199–206. [Google Scholar] [CrossRef] [PubMed]
- Devesa, J.; Reimunde, P.; Devesa, P.; Barberá, M.; Arce, V.M. Growth hormone (GH) and brain trauma. Horm. Behav. 2013, 63, 331–344. [Google Scholar] [CrossRef] [PubMed]
- Devesa, J.; Díaz-Getino, G.; Rey, P.; García-Cancela, J.; Loures, I.; Nogueiras, S.; de Mendoza, A.H.; Salgado, L.; González, M.; Pablos, T.; et al. Brain recovery after a plane crash: Treatment with growth hormone (GH) and neurorehabilitation: A case report. Int. J. Mol. Sci. 2015, 16, 30470–30482. [Google Scholar] [CrossRef] [PubMed]
- García-Aragón, J.; Lobie, P.E.; Muscat, G.E.; Gobius, K.S.; Norstedt, G.; Waters, M.J. Prenatal expression of the growth hormone (GH) receptor/binding protein in the rat: A role for GH in embryonic and fetal development? Development 1992, 114, 869–876. [Google Scholar] [PubMed]
- Turnley, A.M.; Faux, C.H.; Rietze, R.L.; Coonan, J.R.; Bartlett, J.F. Suppressor of cytokine signaling 2 regulates neuronal differentiation by inhibiting growth hormone signaling. Nat. Neurosci. 2002, 5, 1155–1162. [Google Scholar] [CrossRef] [PubMed]
- Lobie, P.E.; Garcia-Aragon, J.; Lincoln, D.T.; Barnard, R.; Wilcox, J.N.; Waters, M.J. Localization and ontogeny of growth hormone receptor gene expression in the central nervous system. Dev. Brain Res. 1993, 74, 225–233. [Google Scholar] [CrossRef]
- Donahue, C.P.; Jensen, R.V.; Ochiishi, T.; Eisenstein, I.; Zhao, M.; Shors, T.; Kosik, K.S. Transcriptional profiling reveals regulated genes in the hippocampus during memory formation. Hippocampus 2002, 12, 821–833. [Google Scholar] [CrossRef] [PubMed]
- Donahue, C.P.; Kosik, K.S.; Shors, T.J. Growth hormone is produced within the hippocampus where it responds to age, sex, and stress. Proc. Natl. Acad. Sci. USA 2006, 103, 6031–6036. [Google Scholar] [CrossRef] [PubMed]
- Nyberg, F.; Hallberg, M. Growth hormone and cognitive function. Nat. Rev. Endocrinol. 2013, 9, 357–365. [Google Scholar] [CrossRef] [PubMed]
- Heredia, M.; Fuente, A.; Criado, J.; Yajeya, J.; Devesa, J.; Riolobos, A.S. Early growth hormone (GH) treatment promotes relevant motor functional improvement after severe frontal cortex lesion in adult rats. Behav. Brain Res. 2013, 247, 48–58. [Google Scholar] [CrossRef] [PubMed]
- Devesa, J.; Lima, L.; Tresguerres, J.A. Neuroendocrine control of growth hormone secretion in humans. Trends Endocrinol. Metab. 1992, 3, 175–183. [Google Scholar] [CrossRef]
- Arce, V.M.; Devesa, P.; Devesa, J. Role of growth hormone (GH) in the treatment of neural diseases: From neuroprotection to neual repair. Neurosci. Res. 2013, 76, 179–186. [Google Scholar] [CrossRef] [PubMed]
- Tomatis, A. El oído y la voz. In Foniatría, 1st ed.; Paidotribo: Badalona, Spain, 2010. [Google Scholar]
- Devesa, J.; Devesa, P.; Reimunde, P. Growth hormone revisited. Med. Clin. 2010, 135, 665–670. [Google Scholar] [CrossRef] [PubMed]
- Costoya, J.A.; Finidori, J.; Moutoussamy, S.; Señarís, R.; Devesa, J.; Arce, V.M. Activation of growth hormone receptor delivers an antiapoptotic signal: Evidence for a role of Akt in this pathway. Endocrinology 1999, 140, 5937–5943. [Google Scholar] [CrossRef] [PubMed]
- Sanders, E.J.; Baudet, M.L.; Parker, E.; Harvey, S. Signaling mechanisms mediating local GH action in the neural retina of the chick embryo. Gen. Comp. Endocrinol. 2009, 163, 63–69. [Google Scholar] [CrossRef] [PubMed]
- McLenachan, S.; Lum, M.G.; Waters, M.J.; Turnley, A.M. Growth hormone promotes proliferation of adult neurosphere cultures. Growth Horm. IGF Res. 2009, 19, 212–218. [Google Scholar] [CrossRef] [PubMed]
- Aberg, N.D.; Johansson, I.; Aberg, M.A.; Lind, J.; Johansson, U.E.; Cooper-Kuhn, C.M.; Kuhn, H.G.; Isgaard, J. Peripheral administration of GH induces cell proliferation in the brain of adult hypophysectomized rats. J. Endocrinol. 2009, 201, 141–150. [Google Scholar] [CrossRef] [PubMed]
- Christophidis, L.J.; Gorba, T.; Gustavsson, M.; Williams, C.E.; Werther, G.A.; Russo, V.C.; Scheepens, A. Growth hormone receptor immunoreactivity is increased in the subventricular zone of juvenile rat brain after focal ischemia: A potential role for growth hormone in injury-induced neurogenesis. Growth Horm. IGF Res. 2009, 19, 497–506. [Google Scholar] [CrossRef] [PubMed]
- Svensson, A.L.; Bucht, N.; Hallberg, M.; Nyberg, F. Reversal of opiate-induced apoptosis by human recombinant growth hormone in murine foetus primary hippocampal neuronal cell cultures. Proc. Natl. Acad. Sci. USA 2008, 105, 7304–7308. [Google Scholar] [CrossRef] [PubMed]
- Devesa, P.; Reimunde, P.; Gallego, R.; Devesa, J.; Arce, V.M. Growth hormone (GH) treatment may cooperate with locally-produced GH in increasing the proliferative response of hippocampal progenitors to kainate-induced injury. Brain Inj. 2011, 25, 503–510. [Google Scholar] [CrossRef] [PubMed]
- High, W.M.; Briones-Galang, M.; Clark, J.A.; Gilkison, C.; Mossberg, K.A.; Zgaljardic, D.J.; Masel, B.E.; Urban, R.J. Effect of growth hormone replacement therapy on cognition after traumatic brain injury. J. Neurotrauma 2010, 27, 1565–1575. [Google Scholar] [CrossRef] [PubMed]
- Reimunde, P.; Quintana, A.; Castañón, B.; Casteleiro, N.; Vilarnovo, Z.; Otero, A.; Devesa, A.; Otero-Cepeda, X.L.; Devesa, J. Effects of growth hormone (GH) replacement and cognitive rehabilitation in patients with cognitive disorders after traumatic brain injury. Brain Inj. 2011, 25, 65–73. [Google Scholar] [CrossRef] [PubMed]
- Devesa, P.; Agasse, F.; Xapelli, S.; Almengló, C.; Devesa, J.; Malva, J.O.; Arce, V.M. Growth hormone pathways signaling for cell proliferation and survival in hippocampal neural precursors from postnatal mice. BMC Neurosci. 2014, 15, 100–112. [Google Scholar] [CrossRef] [PubMed]
- Pathipati, P.; Gorba, T.; Scheepens, A.; Goffin, V.; Sun, Y.; Fraser, M. Growth hormone and prolactin regulate human neural stem cell regenerative activity. Neuroscience 2011, 190, 409–427. [Google Scholar] [CrossRef] [PubMed]
- Aberg, D.N.; Lind, J.; Isgaard, J.; Georg Kuhn, H. Peripheral growth hormone induces cell proliferation in the intact adult rat brain. Growth Horm. IGF Res. 2010, 20, 264–269. [Google Scholar] [CrossRef] [PubMed]
- Waters, M.J.; Blackmore, D.G. Growth hormone (GH), brain development and neural stem cells. Pediatr. Endocrinol. Rev. 2011, 9, 549–553. [Google Scholar] [PubMed]
- Zhang, H.; Han, M.; Zhang, X.; Sun, X.; Ling, F. The effect and mechanism of growth hormone replacement on cognitive function in rats with traumatic brain injury. PLoS ONE 2014, 9. [Google Scholar] [CrossRef] [PubMed]
© 2016 by the authors; licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons by Attribution (CC-BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Devesa, J.; Lema, H.; Zas, E.; Munín, B.; Taboada, P.; Devesa, P. Learning and Memory Recoveries in a Young Girl Treated with Growth Hormone and Neurorehabilitation. J. Clin. Med. 2016, 5, 14. https://doi.org/10.3390/jcm5020014
Devesa J, Lema H, Zas E, Munín B, Taboada P, Devesa P. Learning and Memory Recoveries in a Young Girl Treated with Growth Hormone and Neurorehabilitation. Journal of Clinical Medicine. 2016; 5(2):14. https://doi.org/10.3390/jcm5020014
Chicago/Turabian StyleDevesa, Jesús, Hortensia Lema, Eva Zas, Borja Munín, Pilar Taboada, and Pablo Devesa. 2016. "Learning and Memory Recoveries in a Young Girl Treated with Growth Hormone and Neurorehabilitation" Journal of Clinical Medicine 5, no. 2: 14. https://doi.org/10.3390/jcm5020014
APA StyleDevesa, J., Lema, H., Zas, E., Munín, B., Taboada, P., & Devesa, P. (2016). Learning and Memory Recoveries in a Young Girl Treated with Growth Hormone and Neurorehabilitation. Journal of Clinical Medicine, 5(2), 14. https://doi.org/10.3390/jcm5020014