The Role of Continuous Glucose Monitoring, Diabetes Smartphone Applications, and Self-Care Behavior in Glycemic Control: Results of a Multi-National Online Survey
Abstract
:1. Introduction
2. Materials and Methods
2.1. Ethics Approval and Consent to Participate
2.2. Study Design, Questionnaire and Source of Respondents
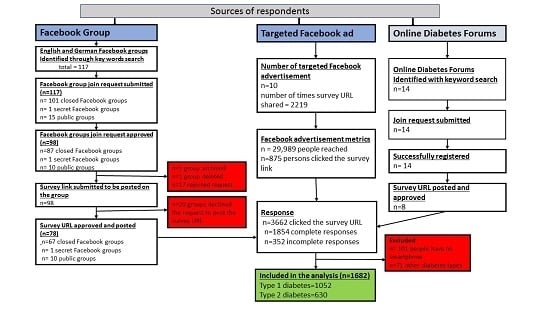
2.3. Recruitment of Survey Participants
2.3.1. Recruitment via Facebook Groups
2.3.2. Recruitment via Targeted Facebook Ads
2.3.3. Recruitment Using Diabetes Online Patient Forums
2.4. Quality of Data
2.5. Data Analysis
3. Results
3.1. Data Source and Characteristics of the Survey Participants
3.2. Diabetes Clinical and Self-Management Characteristics of Respondents
3.3. Self-Care Behavior of the Respondents
3.4. Factors Associated with Hyperglycemia and Hypoglycemia amongst Respondents with Type 1 Diabetes
3.5. Factors Associated with Hyperglycemia and Hypoglycemia Among Respondents with Type 2 DM
4. Discussion
Limitations
5. Conclusions
Supplementary Materials
Author Contributions
Acknowledgments
Availability of Data and Materials
Conflicts of Interest
References
- International Diabetes Federation (IDF). IDF Diabetes Atlas, 8th ed.; International Diabetes Federation: Brussels, Belgium, 2017. [Google Scholar]
- Brown, M.T.; Bussell, J.K. Medication adherence: WHO cares? Mayo Clin. Proc. 2011, 86, 304–314. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization (WHO). Global Report on Diabetes; World Health Organization: Geneva, Switzerland, 2016. [Google Scholar]
- Tuomi, T.; Santoro, N.; Caprio, S.; Cai, M.; Weng, J.; Groop, L. The many faces of diabetes: A disease with increasing heterogeneity. Lancet 2014, 383, 1084–1094. [Google Scholar] [CrossRef]
- International Diabetes Federation (IDF). Diabetes Atlas, 6th ed.; International Diabetes Federation: Brussels, Belgium, 2013. [Google Scholar]
- American Diabetes Association. Standards of medical care in diabetes—2013. Diabetes Care 2013, 36, S11–S66. [Google Scholar]
- Evert, A.B.; Boucher, J.L.; Cypress, M.; Dunbar, S.A.; Franz, M.J.; Mayer-Davis, E.J.; Neumiller, J.J.; Nwankwo, R.; Verdi, C.L.; Urbanski, P.; et al. Nutrition Therapy Recommendations for the Management of Adults with Diabetes. Diabetes Care 2014, 37, S120–S143. [Google Scholar] [CrossRef] [PubMed]
- Strom, J.L.; Egede, L.E. The impact of social support on outcomes in adult patients with type 2 diabetes: A systematic review. Curr. Diabetes Rep. 2012, 12, 769–781. [Google Scholar] [CrossRef]
- Labate, C. The influence of social media on diabetes treatment and self-care. Diabetes Voice 2013, 58, 14–15. [Google Scholar]
- White, K.; Gebremariam, A.; Lewis, D.; Nordgren, W.; Wedding, J.; Pasek, J.; Garrity, A.; Hirschfeld, E.; Lee, J.M. Motivations for Participation in an Online Social Media Community for Diabetes. J. Diabetes Sci. Technol. 2018, 12, 712–718. [Google Scholar] [CrossRef]
- Petrovski, G.; Zivkovic, M.; Stratrova, S.S. Social media and diabetes: Can Facebook and Skype improve glucose control in patients with type 1 diabetes on pump therapy? One-year experience. Diabetes Care 2015, 38, e51–e52. [Google Scholar] [PubMed]
- Nowak, M.; Spiller, G. Two Billion People Coming Together on Facebook. Available online: https://newsroom.fb.com/news/2017/06/two-billion-people-coming-together-on-facebook/ (accessed on 13 February 2017).
- Partridge, S.R.; Gallagher, P.; Freeman, B.; Gallagher, R. Facebook Groups for the Management of Chronic Diseases. J. Med. Internet Res. 2018, 20, e21. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- NHS. Guidance on the Use of Social Media to Actively Involve People in Research. Available online: http://www.invo.org.uk/wp-content/uploads/2017/07/Social-Media-Guide-web-2017.pdf (accessed on 13 February 2017).
- Al Mamun, M.; Ibrahim, H.M.; Turin, T.C. Social media in communicating health information: An analysis of Facebook groups related to hypertension. Prev. Chronic Dis. 2015, 12, E11. [Google Scholar] [CrossRef] [PubMed]
- Abedin, T.; Al Mamun, M.; Lasker, M.A.A.; Ahmed, S.W.; Shommu, N.; Rumana, N.; Turin, T.C. Social Media as a Platform for Information About Diabetes Foot Care: A Study of Facebook Groups. Can. J. Diabetes 2017, 41, 97–101. [Google Scholar] [CrossRef] [PubMed]
- Greene, J.A.; Choudhry, N.K.; Kilabuk, E.; Shrank, W.H. Online social networking by patients with diabetes: A qualitative evaluation of communication with Facebook. J. Gen. Intern. Med. 2011, 26, 287–292. [Google Scholar] [CrossRef] [PubMed]
- Alanzi, T. Role of Social Media in Diabetes Management in the Middle East Region: Systematic Review. J. Med. Internet Res. 2018, 20, e58. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- El-Gayar, O.; Timsina, P.; Nawar, N.; Eid, W. Mobile applications for diabetes self-management: Status and potential. J. Diabetes Sci. Technol. 2013, 7, 247–262. [Google Scholar] [CrossRef]
- American Diabetes Association. Standards of medical care in diabetes—2012. Diabetes Care 2012, 35 (Suppl. 1), S11–S63. [Google Scholar] [CrossRef] [PubMed]
- Kirwan, M.; Vandelanotte, C.; Fenning, A.; Duncan, M.J. Diabetes self-management smartphone application for adults with type 1 diabetes: Randomized controlled trial. J. Med. Internet Res. 2013, 15, e235. [Google Scholar] [CrossRef] [PubMed]
- Williams, J.P.; Schroeder, D. Popular Glucose Tracking Apps and Use of mHealth by Latinos with Diabetes: Review. JMIR mHealth uHealth 2015, 3, e84. [Google Scholar] [CrossRef] [PubMed]
- Ryan, E.A.; Holland, J.; Stroulia, E.; Bazelli, B.; Babwik, S.A.; Li, H.; Senior, P.; Greiner, R. Improved A1C Levels in Type 1 Diabetes with Smartphone App Use. Can. J. Diabetes 2017, 41, 33–40. [Google Scholar] [CrossRef]
- Demidowich, A.P.; Lu, K.; Tamler, R.; Bloomgarden, Z. An evaluation of diabetes self-management applications for Android smartphones. J. Telemed. Telecare 2012, 18, 235–238. [Google Scholar] [CrossRef]
- Muralidharan, S.; Ranjani, H.; Anjana, R.M.; Allender, S.; Mohan, V. Mobile Health Technology in the Prevention and Management of Type 2 Diabetes. Indian J. Endocrinol. Metab. 2017, 21, 334–340. [Google Scholar]
- Hamine, S.; Gerth-Guyette, E.; Faulx, D.; Green, B.B.; Ginsburg, A.S. Impact of mHealth chronic disease management on treatment adherence and patient outcomes: A systematic review. J. Med. Internet Res. 2015, 17, e52. [Google Scholar] [CrossRef]
- Hou, C.; Carter, B.; Hewitt, J.; Francisa, T.; Mayor, S. Do Mobile Phone Applications Improve Glycemic Control (HbA1c) in the Self-management of Diabetes? A Systematic Review, Meta-analysis, and GRADE of 14 Randomized Trials. Diabetes Care 2016, 39, 2089–2095. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kebede, M.M.; Liedtke, T.P.; Möllers, T.; Pischke, C.R. Characterizing Active Ingredients of eHealth Interventions Targeting Persons with Poorly Controlled Type 2 Diabetes Mellitus Using the Behavioral Change Technique Taxonomy. J. Med. Internet Res. 2017, 19, e348. [Google Scholar] [CrossRef] [PubMed]
- Kebede, M.M.; Zeeb, H.; Peters, M.; Heise, T.L.; Pischke, C.R. Effectiveness of Digital Interventions for Improving Glycemic Control in Persons with Poorly Controlled Type 2 Diabetes: A Systematic Review, Meta-analysis, and Meta-regression Analysis. Diabetes Technol. 2018, 20, 767–782. [Google Scholar] [CrossRef] [PubMed]
- Kebede, M.M.; Peters, M.; Heise, T.L.; Pischke, C.R. Comparison of three meta-analytic methods using data from digital interventions on type 2 diabetes. Diabetes Metab. Syndr. Obes. 2019, 12, 59–73. [Google Scholar] [CrossRef] [PubMed]
- Research2Guidance. Diabetes App Market Report 2016–2021. Available online: https://research2guidance.com/product/diabetes-app-market-report-2016-2021/ (accessed on 30 October 2017).
- Research2Guidance. mHealth App Developer Economics 2016. Available online: https://research2guidance.com/product/mhealth-app-developer-economics-2016/ (accessed on 30 October 2017).
- Lanzola, G.; Capozzi, D.; D’Annunzio, G.; Ferrari, P.; Bellazzi, R.; Larizza, C. Going mobile with a multiaccess service for the management of diabetic patients. J. Diabetes Sci. Technol. 2007, 1, 730–737. [Google Scholar] [CrossRef] [PubMed]
- Rao, A.; Hou, P.; Golnik, T.; Flaherty, J.; Vu, S. Evolution of data management tools for managing self-monitoring of blood glucose results: A survey of iPhone applications. J. Diabetes Sci. Technol. 2010, 4, 949–957. [Google Scholar] [CrossRef]
- Eng, D.S.; Lee, J.M. The promise and peril of mobile health applications for diabetes and endocrinology. Pediatr. Diabetes 2013, 14, 231–238. [Google Scholar] [CrossRef]
- R2G. mHealth Economics 2017—Current Status and Future Trends in Mobile Health; Research 2 Guideance: Berlin, Germany, 2017. [Google Scholar]
- Jacques Rose, K.; Petrut, C.; L’Heveder, R.; de Sabata, S. IDF Europe position on mobile applications in diabetes. Diabetes Res. Clin. Pract. 2017. [Google Scholar] [CrossRef]
- Internation Diabetes Federation (IDF). IDF Europe Position on Mobile Applications in Diabetes; Internation Diabetes Federation: Brussels, Belgium, 2017. [Google Scholar]
- Chomutare, T.; Fernandez-Luque, L.; Arsand, E.; Hartvigsen, G. Features of mobile diabetes applications: Review of the literature and analysis of current applications compared against evidence-based guidelines. J. Med. Internet Res. 2011, 13, e65. [Google Scholar] [CrossRef]
- Center for Devices and Radiological Health. Mobile Medical Applications—Guidance for Industry and Food and Drug Administration Staff. Available online: http://www.fda.gov/downloads/MedicalDevices/.../UCM263366.pdf (accessed on 2 November 2017).
- Dolan, B. FDA Clears WellDoc for Diabetes Management. Available online: http://mobihealthnews.com/8539/fda-clears-welldoc-for-diabetes-management (accessed on 19 November 2018).
- Huckvale, K.; Adomaviciute, S.; Prieto, J.T.; Leow, M.K.; Car, J. Smartphone apps for calculating insulin dose: A systematic assessment. BMC Med. 2015, 13, 106. [Google Scholar] [CrossRef]
- Veazie, S.; Winchell, K.; Gilbert, J.; Paynter, R.; Ivlev, I.; Eden, K.; Nussbaum, K.; Weiskopf, N.; Guise, J.M.; Helfand, M. Mobile Applications for Self-Management of Diabetes; Agency for Healthcare Research and Quality: Rockville, MD, USA, 2018. [Google Scholar]
- Shuren, J.; Patel, B.; Gottlieb, S. FDA Regulation of Mobile Medical Apps. JAMA 2018, 320, 337–338. [Google Scholar] [CrossRef] [PubMed]
- Trawley, S.; Browne, J.L.; Hagger, V.L.; Hendrieckx, C.; Holmes-Truscott, E.; Pouwer, F.; Skinner, T.C.; Speight, J. The Use of Mobile Applications Among Adolescents with Type 1 Diabetes: Results from Diabetes MILES Youth—Australia. Diabetes Technol. Ther. 2016, 18, 813–819. [Google Scholar] [CrossRef] [PubMed]
- Boyle, L.; Grainger, R.; Hall, R.M.; Krebs, J.D. Use of and Beliefs About Mobile Phone Apps for Diabetes Self-Management: Surveys of People in a Hospital Diabetes Clinic and Diabetes Health Professionals in New Zealand. JMIR mHealth uHealth 2017, 5, e85. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kramer, U.; Zehner, F. Diabetes-Management mit APPs: Derzeitige & zukünftige Nutzung, Einstellungen, Erfahrungen und Erwartungen von Betroffenen. Online-Befragung von Diabetikern. Aktuelle Ernährungsmedizin 2016, 41, V07. [Google Scholar]
- Brooke, M.J.; Thompson, B.M. Food and Drug Administration regulation of diabetes-related mHealth technologies. J. Diabetes Sci. Technol. 2013, 7, 296–301. [Google Scholar] [CrossRef] [PubMed]
- Schmitz, C.; LimeSurvey Project Team. LimeSurvey: An Open Source Survey Tool; LimeSurvey Project: Hamburg, Germany, 2012. [Google Scholar]
- Toobert, D.J.; Hampson, S.E.; Glasgow, R.E. The summary of diabetes self-care activities measure: Results from 7 studies and a revised scale. Diabetes Care 2000, 23, 943–950. [Google Scholar] [CrossRef] [PubMed]
- Kamradt, M.; Bozorgmehr, K.; Krisam, J.; Freund, T.; Kiel, M.; Qreini, M.; Flum, E.; Berger, S.; Besier, W.; Szecsenyi, J.; et al. Assessing self-management in patients with diabetes mellitus type 2 in Germany: Validation of a German version of the Summary of Diabetes Self-Care Activities measure (SDSCA-G). Health Qual. Life Outcomes 2014, 12, 185. [Google Scholar] [CrossRef] [PubMed]
- American Diabetes Association. Standards of Medical Care in Diabetes—2014. Diabetes Care 2014, 37 (Suppl. 1), S14–S80. [Google Scholar] [CrossRef]
- American Diabetes Association. Glycemic Targets. Diabetes Care 2017, 40, S48–S56. [Google Scholar] [CrossRef]
- Beck, R.W.; Connor, C.G.; Mullen, D.M.; Wesley, D.M.; Bergenstal, R.M. The Fallacy of Average: How Using HbA1c Alone to Assess Glycemic Control Can Be Misleading. Diabetes Care 2017, 40, 994–999. [Google Scholar] [CrossRef]
- Langer, W. The Assessment of Fit in the Class of Logistic Regression Models: A Pathway out of the Jungle of Pseudo-R2s Using Stata. In Proceedings of the Meeting of the German Stata User Group at GESIS, Cologne, Germany, 10 June 2016. [Google Scholar]
- World Bank. World Bank Country and Lending Groups: Country Classification. Available online: https://datahelpdesk.worldbank.org/knowledgebase/articles/906519-world-bank-country-and-lending-groups (accessed on 19 September 2018).
- Trawley, S.; Baptista, S.; Browne, J.L.; Pouwer, F.; Speight, J. The Use of Mobile Applications Among Adults with Type 1 and Type 2 Diabetes: Results from the Second MILES-Australia (MILES-2) Study. Diabetes Technol. 2017, 19, 730–738. [Google Scholar] [CrossRef] [PubMed]
- Conway, N.; Campbell, I.; Forbes, P.; Cunningham, S.; Wake, D. mHealth applications for diabetes: User preference and implications for app development. Health Inform. J. 2016, 22, 1111–1120. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Mathiesen, A.S.; Thomsen, T.; Jensen, T.; Schiotz, C.; Langberg, H.; Egerod, I. The influence of diabetes distress on digital interventions for diabetes management in vulnerable people with type 2 diabetes: A qualitative study of patient perspectives. J. Clin. Transl. Endocrinol. 2017, 9, 41–47. [Google Scholar] [CrossRef] [PubMed]
- Rodriguez, J.A.; Singh, K. The Spanish Availability and Readability of Diabetes Apps. J. Diabetes Sci. Technol. 2018, 12, 719–724. [Google Scholar] [CrossRef] [PubMed]
- Schramm, W. Digital Diabetes Self-Management: A Trilateral Serial. J. Diabetes Sci. Technol. 2018, 12, 709–711. [Google Scholar] [CrossRef] [PubMed]
- Ernsting, C.; Dombrowski, S.U.; Oedekoven, M.; O’Sullivan, J.L.; Kanzler, M.; Kuhlmey, A.; Gellert, P. Using Smartphones and Health Apps to Change and Manage Health Behaviors: A Population-Based Survey. J. Med. Internet Res. 2017, 19, e101. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Krebs, P.; Duncan, D.T. Health App Use Among US Mobile Phone Owners: A National Survey. JMIR mHealth uHealth 2015, 3, e101. [Google Scholar] [CrossRef] [Green Version]
- Tang, T.S.; Brown, M.B.; Funnell, M.M.; Anderson, R.M. Social Support, Quality of Life, and Self-Care Behaviors Among African Americans With Type 2 Diabetes. Diabetes Educ. 2008, 34, 266–276. [Google Scholar] [CrossRef]
- Andrade, C.S.; Ribeiro, G.S.; Santos, C.; Neves, R.C.S.; Moreira, E.D., Jr. Factors associated with high levels of glycated haemoglobin in patients with type 1 diabetes: A multicentre study in Brazil. BMJ Open 2017, 7, e018094. [Google Scholar] [CrossRef]
- Sastre, J.; Pines, P.J.; Moreno, J.; Aguirre, M.; Blanco, B.; Calderon, D.; Herranz, S.; Roa, C.; Lopez, J.; Grupo de estudio, D. Metabolic control and treatment patterns in patients with type 1 diabetes in Castilla-La Mancha: The DIAbetes tipo 1 in Castilla La Mancha study. Endocrinol. Nutr. 2012, 59, 539–546. [Google Scholar] [CrossRef]
- Grohmann, B.; Espin, S.; Gucciardi, E. Patients’ experiences of diabetes education teams integrated into primary care. Can. Fam. Physician 2017, 63, e128–e136. [Google Scholar] [PubMed]
- Castro, C.M.; Wilson, C.; Wang, F.; Schillinger, D. Babel babble: Physicians’ use of unclarified medical jargon with patients. Am. J. Health Behav. 2007, 31 (Suppl. 1), S85–S95. [Google Scholar] [CrossRef]
- Williams, M.V.; Davis, T.; Parker, R.M.; Weiss, B.D. The role of health literacy in patient-physician communication. Fam. Med. 2002, 34, 383–389. [Google Scholar] [PubMed]
- Schillinger, D.; Barton, L.R.; Karter, A.J.; Wang, F.; Adler, N. Does literacy mediate the relationship between education and health outcomes? A study of a low-income population with diabetes. Public Health Rep. 2006, 121, 245–254. [Google Scholar] [CrossRef] [PubMed]
- Bornemisza, P.; Suciu, I. Effect of cigarette smoking on the blood glucose level in normals and diabetics. Med. Interne 1980, 18, 353–356. [Google Scholar] [PubMed]
- Gerber, P.A.; Locher, R.; Schmid, B.; Spinas, G.A.; Lehmann, R. Smoking is associated with impaired long-term glucose metabolism in patients with type 1 diabetes mellitus. Nutr. Metab. Cardiovasc. Dis. 2013, 23, 102–108. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Scott, L.J.; Warram, J.H.; Hanna, L.S.; Laffel, L.M.; Ryan, L.; Krolewski, A.S. A nonlinear effect of hyperglycemia and current cigarette smoking are major determinants of the onset of microalbuminuria in type 1 diabetes. Diabetes 2001, 50, 2842–2849. [Google Scholar] [CrossRef]
- Gunton, J.E.; Davies, L.; Wilmshurst, E.; Fulcher, G.; McElduff, A. Cigarette smoking affects glycemic control in diabetes. Diabetes Care 2002, 25, 796–797. [Google Scholar] [CrossRef]
- Vu, C.U.; Siddiqui, J.A.; Wadensweiler, P.; Gayen, J.R.; Avolio, E.; Bandyopadhyay, G.K.; Biswas, N.; Chi, N.W.; O’Connor, D.T.; Mahata, S.K. Nicotinic acetylcholine receptors in glucose homeostasis: The acute hyperglycemic and chronic insulin-sensitive effects of nicotine suggest dual opposing roles of the receptors in male mice. Endocrinology 2014, 155, 3793–3805. [Google Scholar] [CrossRef]
- Attvall, S.; Fowelin, J.; Lager, I.; Von Schenck, H.; Smith, U. Smoking induces insulin resistance—A potential link with the insulin resistance syndrome. J. Intern. Med. 1993, 233, 327–332. [Google Scholar] [CrossRef]
- Schmitt, A.; Gahr, A.; Hermanns, N.; Kulzer, B.; Huber, J.; Haak, T. The Diabetes Self-Management Questionnaire (DSMQ): Development and evaluation of an instrument to assess diabetes self-care activities associated with glycaemic control. Health Qual. Life Outcomes 2013, 11, 138. [Google Scholar] [CrossRef] [PubMed]
- Ryan, D.B.; Swift, C.S. The Mealtime Challenge: Nutrition and Glycemic Control in the Hospital. Diabetes Spectr. 2014, 27, 163–168. [Google Scholar] [CrossRef] [PubMed]
- Sheikh, K.; Bartz, S.K.; Lyons, S.K.; DeSalvo, D.J. Diabetes Device Use and Glycemic Control among Youth with Type 1 Diabetes: A Single-Center, Cross-Sectional Study. J. Diabetes Res. 2018, 2018, 1–6. [Google Scholar] [CrossRef] [PubMed]
- Canadian Diabetes Association Clinical Practice Guidelines Expert Committee; Berard, L.D.; Siemens, R.; Woo, V. Monitoring Glycemic Control. Can. J. Diabetes 2018, 42 (Suppl. 1), S47–S53. [Google Scholar] [CrossRef] [PubMed]
- Wallia, A.; Umpierrez, G.E.; Nasraway, S.A.; Klonoff, D.C. Round Table Discussion on Inpatient Use of Continuous Glucose Monitoring at the International Hospital Diabetes Meeting. J. Diabetes Sci. Technol. 2016, 10, 1174–1181. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Klonoff, D.C.; Ahn, D.; Drincic, A. Continuous glucose monitoring: A review of the technology and clinical use. Diabetes Res. Clin. Pract. 2017, 133, 178–192. [Google Scholar] [CrossRef] [PubMed]
- Wang, J.; Zgibor, J.; Matthews, J.T.; Charron-Prochownik, D.; Sereika, S.M.; Siminerio, L. Self-monitoring of blood glucose is associated with problem-solving skills in hyperglycemia and hypoglycemia. Diabetes Educ. 2012, 38, 207–218. [Google Scholar] [CrossRef] [PubMed]
- Ward, J.E.; Stetson, B.A.; Mokshagundam, S.P. Patient perspectives on self-monitoring of blood glucose: Perceived recommendations, behaviors and barriers in a clinic sample of adults with type 2 diabetes. J. Diabetes Metab. Disord. 2015, 14, 43. [Google Scholar] [CrossRef]
- Simmons, J.H.; Chen, V.; Miller, K.M.; McGill, J.B.; Bergenstal, R.M.; Goland, R.S.; Harlan, D.M.; Largay, J.F.; Massaro, E.M.; Beck, R.W. Differences in the Management of Type 1 Diabetes Among Adults Under Excellent Control Compared with Those Under Poor Control in the T1D Exchange Clinic Registry. Diabetes Care 2013, 36, 3573–3577. [Google Scholar] [CrossRef]
- Snow, R.; Humphrey, C.; Sandall, J. What happens when patients know more than their doctors? Experiences of health interactions after diabetes patient education: A qualitative patient-led study. BMJ Open 2013, 3. [Google Scholar] [CrossRef]
- Reddy, M.; Rilstone, S.; Cooper, P.; Oliver, N.S. Type 1 diabetes in adults: Supporting self management. BMJ 2016, 352, i998. [Google Scholar] [CrossRef] [PubMed]
- Offringa, R.; Sheng, T.; Parks, L.; Clements, M.; Kerr, D.; Greenfield, M.S. Digital Diabetes Management Application Improves Glycemic Outcomes in People with Type 1 and Type 2 Diabetes. J. Diabetes Sci. Technol. 2018, 12, 701–708. [Google Scholar] [CrossRef] [PubMed]
- Orsama, A.L.; Lahteenmaki, J.; Harno, K.; Kulju, M.; Wintergerst, E.; Schachner, H.; Stenger, P.; Leppanen, J.; Kaijanranta, H.; Salaspuro, V.; et al. Active assistance technology reduces glycosylated hemoglobin and weight in individuals with type 2 diabetes: Results of a theory-based randomized trial. Diabetes Technol. 2013, 15, 662–669. [Google Scholar] [CrossRef] [PubMed]
- Waki, K.; Fujita, H.; Uchimura, Y.; Omae, K.; Aramaki, E.; Kato, S.; Lee, H.; Kobayashi, H.; Kadowaki, T.; Ohe, K. DialBetics: A Novel Smartphone-based Self-management Support System for Type 2 Diabetes Patients. J. Diabetes Sci. Technol. 2014, 8, 209–215. [Google Scholar] [CrossRef] [PubMed]
- Kumar, S.; Moseson, H.; Uppal, J.; Juusola, J.L. A Diabetes Mobile App with In-App Coaching From a Certified Diabetes Educator Reduces A1C for Individuals With Type 2 Diabetes. Diabetes Educ. 2018, 44, 226–236. [Google Scholar] [CrossRef] [PubMed]
- Froisland, D.H.; Arsand, E.; Skarderud, F. Improving diabetes care for young people with type 1 diabetes through visual learning on mobile phones: Mixed-methods study. J. Med. Internet Res. 2012, 14, e111. [Google Scholar] [CrossRef] [PubMed]
- Sayed, M.H.; Hegazi, M.A.; Abdulwahed, K.; Moussa, K.; El-Deek, B.S.; Gabel, H.; Ragheb, R. Risk factors and predictors of uncontrolled hyperglycemia and diabetic ketoacidosis in children and adolescents with type 1 diabetes mellitus in Jeddah, western Saudi Arabia. J. Diabetes 2017, 9, 190–199. [Google Scholar] [CrossRef]
- Tan, S.L.; Juliana, S.; Sakinah, H. Dietary compliance and its association with glycemic control among poorly controlled type 2 diabetic outpatients in Hospital Universiti Sains Malaysia. Malays. J. Nutr. 2011, 17, 287–299. [Google Scholar]
- Zhang, Y.; Ting, R.Z.W.; Yang, W.; Jia, W.; Li, W.; Ji, L.; Guo, X.; Kong, A.P.S.; Wing, Y.K.; Luk, A.O.Y.; et al. Depression in Chinese patients with type 2 diabetes: Associations with hyperglycemia, hypoglycemia, and poor treatment adherence. J. Diabetes 2015, 7, 800–808. [Google Scholar] [CrossRef]
- Barnard, N.D.; Cohen, J.; Jenkins, D.J.; Turner-McGrievy, G.; Gloede, L.; Jaster, B.; Seidl, K.; Green, A.A.; Talpers, S. A low-fat vegan diet improves glycemic control and cardiovascular risk factors in a randomized clinical trial in individuals with type 2 diabetes. Diabetes Care 2006, 29, 1777–1783. [Google Scholar] [CrossRef]
- Davis, N.J.; Tomuta, N.; Schechter, C.; Isasi, C.R.; Segal-Isaacson, C.J.; Stein, D.; Zonszein, J.; Wylie-Rosett, J. Comparative Study of the Effects of a 1-Year Dietary Intervention of a Low-Carbohydrate Diet Versus a Low-Fat Diet on Weight and Glycemic Control in Type 2 Diabetes. Diabetes Care 2009, 32, 1147–1152. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Jonsson, T.; Granfeldt, Y.; Ahren, B.; Branell, U.C.; Palsson, G.; Hansson, A.; Soderstrom, M.; Lindeberg, S. Beneficial effects of a Paleolithic diet on cardiovascular risk factors in type 2 diabetes: A randomized cross-over pilot study. Cardiovasc. Diabetol. 2009, 8, 35. [Google Scholar] [CrossRef] [PubMed]
- Khoo, J.; Piantadosi, C.; Duncan, R.; Worthley, S.G.; Jenkins, A.; Noakes, M.; Worthley, M.I.; Lange, K.; Wittert, G.A. Comparing effects of a low-energy diet and a high-protein low-fat diet on sexual and endothelial function, urinary tract symptoms, and inflammation in obese diabetic men. J. Sex. Med. 2011, 8, 2868–2875. [Google Scholar] [CrossRef] [PubMed]
- Wolever, T.M.; Gibbs, A.L.; Mehling, C.; Chiasson, J.L.; Connelly, P.W.; Josse, R.G.; Leiter, L.A.; Maheux, P.; Rabasa-Lhoret, R.; Rodger, N.W.; et al. The Canadian Trial of Carbohydrates in Diabetes (CCD), a 1-y controlled trial of low-glycemic-index dietary carbohydrate in type 2 diabetes: No effect on glycated hemoglobin but reduction in C-reactive protein. Am. J. Clin. Nutr. 2008, 87, 114–125. [Google Scholar] [CrossRef] [PubMed]
- Selvin, E.; Parrinello, C.M. Age-related differences in glycaemic control in diabetes. Diabetologia 2013, 56, 2549–2551. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Crandall, J.; Barzilai, N. Treatment of diabetes mellitus in older people: Oral therapy options. J. Am. Geriatr. Soc. 2003, 51, 272–274. [Google Scholar] [CrossRef] [PubMed]
- Knowler, W.C.; Barrett-Connor, E.; Fowler, S.E.; Hamman, R.F.; Lachin, J.M.; Walker, E.A.; Nathan, D.M. Reduction in the incidence of type 2 diabetes with lifestyle intervention or metformin. N. Engl. J. Med. 2002, 346, 393–403. [Google Scholar] [PubMed]
- Pani, L.N.; Korenda, L.; Meigs, J.B.; Driver, C.; Chamany, S.; Fox, C.S.; Sullivan, L.; D’Agostino, R.B.; Nathan, D.M. Effect of aging on A1C levels in individuals without diabetes: Evidence from the Framingham Offspring Study and the National Health and Nutrition Examination Survey 2001–2004. Diabetes Care 2008, 31, 1991–1996. [Google Scholar] [CrossRef]
- Tong, W.T.; Vethakkan, S.R.; Ng, C.J. Why do some people with type 2 diabetes who are using insulin have poor glycaemic control? A qualitative study. BMJ Open 2015, 5, e006407. [Google Scholar] [CrossRef]
- Whittemore, R.; D’Eramo Melkus, G.; Grey, M. Metabolic control, self-management and psychosocial adjustment in women with type 2 diabetes. J. Clin. Nurs. 2005, 14, 195–203. [Google Scholar] [CrossRef]


| Variable | Respondents with Type 1 DM Glycemic Control Levels N (%) | Respondents with Type 2 DM Glycemic Control Levels N (%) | ||||||
|---|---|---|---|---|---|---|---|---|
| Good | Hyper | Hypo | Total | Good | Hyper | Hypo | Total | |
| Age, Mean (SD) | 40 (12.9) | 36.7 (12.5) | 36 (13.2) | 39 (12.9) | 52.8 (11.4) | 52.8 (11.1) | 61.5 (14.1) | 52.9 (11.4) |
| ≤40 | 379 (52.8) | 178 (64) | 34 (60.7) | 591 (56.2) | 70 (17.8) | 29 (12.8) | 0 (0) | 99 (15.7) |
| 40–60 | 294 (40.9) | 86 (31) | 20 (35.7) | 400 (38) | 203 (51.7) | 137 (60.6) | 6 (54.6) | 346 (54.9) |
| 60+ | 45 (6.3) | 14 (5) | 2 (3.6) | 61 (5.8) | 120 (30.5) | 60 (26.6) | 5 (45.4) | 185 (29.4) |
| Sex | ||||||||
| Female | 509 (70.9) | 215 (77.3) | 39 (69.6) | 763 (72.5) | 255 (64.9) | 156 (69) | 9 (81.8) | 420 (66.7) |
| Male | 209 (29.1) | 63 (22.3) | 17 (30.4) | 289 (27.5) | 138 (35.1) | 70 (31) | 2 (18.2) | 210 (33.3) |
| Educational Status | ||||||||
| Primary to secondary | 252 (35.1) | 141 (50.7) | 17 (30.4) | 410 (39) | 156 (39.7) | 116 (51.3) | 6 (54.5) | 278 (44.1) |
| Polytechnic diploma | 121 (16.9) | 51 (18.4) | 12 (21.4) | 184 (17.5) | 76 (19.3) | 37 (16.4) | 4 (36.4) | 117 (18.6) |
| Bachelor degree and above | 345 (48) | 86 (30.9) | 27 (48.2) | 458 (43.5) | 161 (40.1) | 73 (32.3) | 1 (9.1) | 235 (37.3) |
| Continent | ||||||||
| USA/Canada/Central America | 237 (33) | 96 (34.5) | 20 (35.7) | 353 (33.6) | 181 (46.1) | 93 (41.2) | 2 (43.8) | 276 (43.8) |
| Europe | 418 (58.2) | 161 (58) | 28 (50) | 607 (55.7) | 143 (36.4) | 90 (39.8) | 6 (55) | 239 (38) |
| Oceania | 49 (5.4) | 8 (2.9) | 5 (8.9) | 52 (4.9) | 18 (4.6) | 4 (1.8) | 2 (18.1) | 24 (3.8) |
| Asia | 10 (1.4) | 4 (1.4) | 1 (1.8) | 15 (1.4) | 41 (10.4) | 25 (11) | 1 (9.1) | 67 (10.6) |
| Africa and Latin America | 14 (2) | 9 (3.2) | 2 (3.6) | 25 (2.4) | 10 (2.5) | 14 (6.2) | 0 (0) | 24 (3.8) |
| Country income levels * | ||||||||
| Low to lower-middle income | 8 (1.1) | 2 (0.7) | 0 (0) | 19 (1) | 41 (10.4) | 26 (11.5) | 1 (9.1) | 68 (10.7) |
| Upper-middle income | 16 (2.2) | 12 (4.3) | 2 (3.6) | 30 (3) | 9 (2.3) | 13 (5.8) | 0 (0) | 22 (3.6) |
| High income | 694 (96.7) | 264 (95) | 54 (96.4) | 1012 (96) | 343 (87.3) | 187 (82.7) | 10 (90.9) | 540 (85.7) |
| Total | 718 (68.2) | 278 (26.4) | 56 (5.3) | 1052 (100) | 393 (62.4) | 226 (35.8) | 11 (1.8) | 630 (100) |
| Respondents with Type 1 DM Glycemic Control Levels N (%) | Respondents with Type 2 DM Glycemic Control Levels N (%) | |||||||
|---|---|---|---|---|---|---|---|---|
| Good | Hyper | Hypo | Total | Good | Hyper | Hypo | Total | |
| On glucose lowering medication | ||||||||
| Yes | 684 (95.3) | 266 (95.7) | 54 (96.4) | 1004 (95.4) | 332 (84.5) | 202 (89.4) | 7 (63.6) | 541 (85.9) |
| No | 34 (4.7) | 12 (4.3) | 2 (3.6) | 48 (4.6) | 61 (15.5) | 24 (10.6) | 4 (36.4) | 89 (14.1) |
| If you have concerns regarding your diabetes management where do you go first for assistance? | ||||||||
| Diabetes specialist team/healthcare provider | 445 (62) | 180 (64.8) | 35 (62.5) | 660 (62.7) | 265 (67.4) | 156 (69) | 10 (90.9) | 431 (68.4) |
| Facebook group/Internet/Smartphone App | 214 (29.8) | 85 (30.6) | 17 (30.4) | 316 (30) | 98 (24.9) | 54 (23.9) | 1 (9.1) | 153 (24.3) |
| Support group/Friends/Family | 50 (7) | 12 (4.3) | 4 (7.1) | 66 (6.3) | 24 (6.1) | 14 (6.2) | 0 (0) | 38 (6) |
| Other | 9 (1.25) | 1 (0.36) | 0 (0) | 10 (1) | 6 (1.5) | 2 (0.9) | 0 (0) | 8 (1.3) |
| Problems with Diabetes Self-Management | ||||||||
| Feeling Symptomatic Low Blood Sugar | ||||||||
| Yes | 443 (61.7) | 182 (65.5) | 38 (67.9) | 663 (63) | 87 (22.1) | 33 (14.6) | 1 (9.1) | 121 (19.2) |
| No | 275 (38.3) | 96 (34.5) | 18 (32.1) | 389 (37) | 306 (77.9) | 193 (85.4) | 10 (90.9) | 509 (80.8) |
| Feeling Symptomatic High Blood Sugar | ||||||||
| Yes | 321 (44.7) | 180 (64.8) | 31 (55.4) | 532 (50.6) | 87 (22.1) | 109 (48.2) | 4 (36.4) | 200 (31.8) |
| No | 397 (35.3) | 98 (35.3) | 25 (44.6) | 520 (49.4) | 306 (77.9) | 117 (51.8) | 7 (65.6) | 430 (68.2) |
| Forgetting to Measure Blood Sugar Levels | ||||||||
| Yes | 121 (16.9) | 113 (40.7) | 13 (23.2) | 247 (23.4) | 82 (20.9) | 92 (40.7) | 1 (9.1) | 175 (22.8) |
| No | 597 (83.2) | 165 (59.4) | 43 (76.8) | 805 (76.5) | 311 (79) | 134 (59.3) | 10 (90.1) | 455(72.2) |
| Forgetting to Take Medication or Insulin | ||||||||
| Yes | 106 (14.8) | 70 (25.2) | 10 (17.9) | 186 (17.7) | 49 (12.5) | 58 (25.7) | 2 (18.2) | 109 (17.3 |
| No | 612 (85.2) | 208 (74.8) | 46 (82.1) | 866 (82.3) | 344 (87.5) | 168 (74.3) | 9 (81.8) | 521 (82.7) |
| Not knowing how to identify high or low blood sugars | ||||||||
| Yes | 37 (5.2) | 15 (5.4) | 5 (8.9) | 57 (5.4) | 34 (8.7) | 31 (13.7) | 0 (0) | 65 (10.3) |
| No | 681 (94.9) | 263 (94.6) | 51 (91.1) | 995 (94.6) | 359 ((91.4) | 195 (86.3) | 11 (100) | 565 (89.7) |
| Not Knowing whom to Contact when in Need of Assistance | ||||||||
| Yes | 29 (4) | 11 (4) | 1 (1.8) | 41 (3.9) | 26 (6.6) | 24 (10.6) | 0 (0) | 50 (7.9) |
| No | 689 (96) | 267 (96) | 55 (98.2) | 1011 (96.1) | 367 (93.4) | 302 (89.4) | 11 (100) | 580 (92.1) |
| Being Left without Medication/Supplies | ||||||||
| Yes | 64 (8.9) | 36 (13) | 5 (9) | 105 (10) | 25 (6.4) | 19 (8.4) | 0 (0) | 44 (7) |
| No | 624 (91.1) | 242 (87) | 51 (91) | 947 (90) | 368 (93.6) | 207 (91.6) | 11 (100) | 586 (93) |
| Felt Unsure about How to Calculate Your Insulin/Glucose lowering Medication Dose | ||||||||
| Yes | 105 (14.6) | 64 (23) | 18 (32.1) | 187 (17.8) | 14 (3.6) | 16 (8.4) | 1 (9.1) | 34 (5.4) |
| No | 613 (85.4) | 214 (77) | 38 (79.9) | 865 (82.2) | 379 (96.4) | 207 (91.6) | 10 (90.9) | 596 (94.6) |
| Diabetes App Use | ||||||||
| Yes | 401 (55.9) | 122 (43.9) | 26 (46.4) | 549 (52.2) | 156 (39.7) | 53 (23.5) | 1 (9.1) | 210 (33.3) |
| No | 317 (44.2) | 156 (56.1) | 30 (53.4) | 503 (47.8) | 237 (60.3) | 173 (76.6) | 10 (90.9) | 420 (66.7) |
| Use CGM | ||||||||
| Yes | 234 (32.6) | 56 (20.1) | 6 (10.7) | 296 (28.1) | 17 (4.3) | 4 (1.8) | 0 (0) | 218 (3.3) |
| NO | 484 (67.4) | 222 (79.9) | 50 (89.3) | 756 (71.9) | 376 (95.7) | 222 (98.2) | 11 (100) | 609 (96.7) |
| Self-Reported Rating of Blood Glucose Control | ||||||||
| Well controlled | 521 (72.8) | 107 (38.5) | 27 (48) | 655 (62.4) | 264 (67.5) | 52 (23) | 7 (63.6) | 323 (51) |
| Neutral | 149 (20.8) | 96 (34.5) | 11 (20) | 256 (24.4) | 88 (22.5) | 63 (27.9) | 3 (27.3) | 154 (25) |
| Poorly controlled | 46 (6.4) | 75 (27) | 18 (32) | 139 (13.2) | 39 (10) | 111 (49.1) | 1 (9.1) | 151 (24) |
| Self-Reported Confidence on Diabetes Self-Management | ||||||||
| Very confident | 533 (74.3) | 140 (50.5) | 33 (58.9) | 706 (67.2) | 221 (56) | 55 (24.3) | 6 (54.6) | 282(44.8) |
| Neutral | 66 (9.2) | 48 (17.3) | 8(14.3) | 122 (11.6) | 54(14) | 41 (18.1) | 2 (18.2) | 97(15.4) |
| Not confident at all | 118 (26.5) | 89 (32.1) | 15 (26.8) | 222 (21.1) | 118 (36) | 130 (57.5) | 3 (27.3) | 251(39.8) |
| Smoking | ||||||||
| Yes | 120 (16.7) | 90 (32.4) | 15 (32.4) | 225 (21.4) | 60 (15.3) | 48 (21.2) | 1 (9.1) | 109 (17.3) |
| No | 598 (83.3) | 188 (67.6) | 41 (73.2) | 827 (78.6) | 333 (84.7) | 178 (78.8) | 10 (90.9) | 521 (82.7) |
| Total | 718 (100) | 278 (100) | 56 (100) | 1052 (100) | 393 (100) | 226 (100) | 11 (100) | 630 (100) |
| Self-Care Behavior | Type 1 Diabetes Mean (SD) | Type 2 Diabetes Mean (SD) | Difference (p value) |
|---|---|---|---|
| Diet | |||
| How many of the last SEVEN DAYS have you followed a healthful eating plan? | 4.5 (2.13) | 4.6 (2.11) | 0.412 |
| On average, over the past month, how many DAYS PER WEEK have you followed your eating plan? | 4.6 (2.07) | 4.8 (1.97) | 0.067 |
| On how many of the last SEVEN DAYS did you eat five or more servings of fruits and vegetables | 3.7 (2.51) | 3.6 (2.54) | 0.345 |
| On how many of the last SEVEN DAYS did you eat high fat foods such as red meat or full-fat dairy products? | 3.7 (2.3) | 3.4 (2.41) | 0.070 |
| General diet (aggregate) | 4.5 (2.01) | 4.7 (1.92) | 0.153 |
| Specific diet(aggregate) | 3.5 (1.78) | 3.6 (1.81) | 0.608 |
| Physical activity | |||
| On how many of the last SEVEN DAYS did you participate in at least 30 min of physical activity? (Total minutes of continuous activity, including walking). | 4.0 (2.35) | 3.7 (2.48) | 0.022 * |
| On how many of the last SEVEN DAYS did you participate in a specific exercise session (such as swimming, walking, biking) other than what you do around the house or as part of your work? | 2.4 (2.34) | 2.5 (2.56) | 0.524 |
| Physical activity (aggregate) | 3.2 (2.09) | 3.1 (2.26) | 0.356 |
| Blood Glucose Monitoring | |||
| On how many of the last SEVEN DAYS did you test your blood sugar? | 6.7 (1.15) | 5.0 (2.63) | <0.001 * |
| On how many of the last SEVEN DAYS did you test your blood sugar the number of times recommended by your health care provider? | 6.0 (2.09) | 4.2 (2.95) | <0.001 * |
| Blood glucose monitoring (aggregate) | 6.3 (1.47) | 4.6 (2.58) | <0.001 * |
| Foot Care | |||
| On how many of the last SEVEN DAYS did you check your feet? | 2.6 (2.76) | 3.6 (2.89) | <0.001 * |
| On how many of the last SEVEN DAYS did you inspect the inside of your shoes? | 0.9 (1.96) | 1.6 (2.56) | <0.001 * |
| Foot care (aggregate) | 1.8 (2.04) | 2.6 (2.38) | <0.001 * |
| Self-Care Behavior | Respondents with Type 1 DM Glycemic Control Levels N (%) | Respondents with Type 2 DM Glycemic Control Levels N (%) | ||||||
|---|---|---|---|---|---|---|---|---|
| Good | Hyper | Hypo | Total | Good | Hyper | Hypo | Total | |
| General Diet (Mean(SD)) | 4.8 (1.9) | 3.8 (2.1) | 4.5 (2.1) | 4.6 (2.0) | 5.1 (1.8) | 3.9 (2.0) | 4.8 (1.2) | 4.7 (1.9) |
| Specific Diet (Mean(SD)) | 3.6 (1.8) | 3.3 (1.7) | 3.6 (1.9) | 3.5 (1.8) | 3.7 (1.8) | 3.4 (1.8) | 4 (1.9) | 3.6 (1.8) |
| Physical Activity (Mean(SD)) | 3.4 (2.1) | 2.7 (2.0) | 3.5 (2.3) | 3.2 (2.1) | 3.4 (2.2) | 2.5 (2.2) | 3.5 (2.2) | 3.1 (2.3) |
| Blood Glucose Monitoring (Mean(SD)) | 6.5 (1.3) | 5.9 (1.8) | 6.2 (1.8) | 6.3 (1.5) | 4.9 (2.5) | 4.1 (2.6) | 5.5 (2.1) | 4.6 (2.6) |
| Foot Care (Mean(SD)) | 1.8 (2.1) | 1.6 (1.9) | 1.9 (2.2) | 1.8 (2.0) | 2.7 (2.4) | 2.4 (2.4) | 3.5 (2.5) | 2.6 (2.4) |
| Type 1 Diabetes (n = 1052) | Type 2 Diabetes (n = 630) | |||
|---|---|---|---|---|
| Variables | Hyperglycemia vs. Good Glycemic Control | Hypoglycemia vs. Good Glycemic Control | Hyperglycemia vs. Good Glycemic Control | Hypoglycemia vs. Good Glycemic Control |
| AOR (95% CI) | AOR (95% CI) | AOR (95% CI) | AOR (95% CI) | |
| Age group | ||||
| ≤40 | 1 (reference) | 1 (reference) | ||
| 40–60 | 0.78 (0.56–1.10) | 0.80 (0.43–1.48) | ||
| 60+ | 1.09 (0.54–2.18) | 0.62 (0.14–2.81) | ||
| Age (continuous) | 1.02 (1.00–1.04) * | 1.07 (1.01–1.14) * | ||
| Sex | ||||
| Female | 1 (reference) | 1 (reference) | 1 (reference) | 1 (reference) |
| Male | 0.80 (0.56–1.15) | 1.17 (0.63–2.19) | 1.12 (0.74–1.67) | 0.24 (0.04–1.34) |
| Education | ||||
| Primary to secondary school | 1.70 (1.21–2.39) ** | 0.69 (0.36–1.34) | 1.30 (0.85–1.98) | 8.56 (0.88–83.31) |
| Poly technique diploma | 1.47 (0.95–2.27) | 1.07 (0.51–2.23) | 0.84 (0.49–1.44) | 11 (1.06–113.9) * |
| Bachelor degree and above | 1 (reference) | 1 (reference) | 1 (reference) | 1 (reference) |
| Diabetes app use | ||||
| Yes | 0.98 (0.69–1.39) | 1.19 (0.65–2.20) | 0.63 (0.41– 0.96) * | 0.13 (0.01–1.14) |
| No | 1 (reference) | 1 (reference) | 1 (reference) | 1 (reference) |
| Self-care behavior | ||||
| General diet | 0.86 (0.79–0.94) ** | 0.93 (0.79–1.09) | 0.84 (0.75–0.94) ** | 0.80 (0.51–1.23) |
| Specific diet | 1.00 (0.91–1.10) | 1.01 (0.85–1.20) | 1.02 (0.91–1.14) | 1.13 (0.75–1.70) |
| Physical activity | 0.93 (0.86–1.01) | 1.09 (0.95–1.26) | 0.96 (0.87–1.05) | 1.12 (0.80–1.58) |
| Blood glucose monitoring | 0.88 (0.80–0.97) * | 0.91 (0.76–1.10) | 0.96 (0.88–1.03) | 1.26 (0.92–1.72) |
| Foot care | 1.00 (0.92–1.08) | 1.03 (0.90–1.19) | 0.97 (0.89–1.05) | 1.11 (0.84–1.47) |
| Smoking | ||||
| Yes | 1.63 (1.15–2.32) ** | 1.67 (0.86–3.25) | 1.16 (0.70–1.90) | 0.57 (0.06–5.09) |
| No | 1 (reference) | 1 (reference) | 1 (reference) | 1 (reference) |
| Glucose lowering medication | ||||
| Yes | 1.25 (0.61–2.54) | 1.45 (0.33–6.36) | 0.93 (0.52–1.68) | 0.27 (0.06–1.22) |
| No | 1 (reference) | 1 (reference) | 1 (reference) | 1 (reference) |
| Diabetes self-management concern | ||||
| High concern | 2.09 (1.50–2.92) ** | 1.94 (1.04–3.61) * | 2.59 (1.74–3.84) ** | 0.83 (0.16–4.39) |
| Low concern | 1 (reference) | 1(reference) | 1 (reference) | 1 (reference) |
| Use CGM | ||||
| Yes | 0.66 (0.44–1.00) * | 0.24 (0.09–0.60) ** | ||
| No | 1 | 1 | ||
| Self-reported confidence on diabetes self-management | ||||
| Very confident | 1 (reference) | 1 (reference) | 1 (reference) | 1 (reference) |
| Neutral | 2.13 (1.23–3.72) ** | 1.53 (0.24–10.00) | ||
| Not confident at all | 3.22 (2.07–5.00) ** | 1.12 (0.21–6.01) | ||
© 2019 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kebede, M.M.; Schuett, C.; Pischke, C.R. The Role of Continuous Glucose Monitoring, Diabetes Smartphone Applications, and Self-Care Behavior in Glycemic Control: Results of a Multi-National Online Survey. J. Clin. Med. 2019, 8, 109. https://doi.org/10.3390/jcm8010109
Kebede MM, Schuett C, Pischke CR. The Role of Continuous Glucose Monitoring, Diabetes Smartphone Applications, and Self-Care Behavior in Glycemic Control: Results of a Multi-National Online Survey. Journal of Clinical Medicine. 2019; 8(1):109. https://doi.org/10.3390/jcm8010109
Chicago/Turabian StyleKebede, Mihiretu M., Cora Schuett, and Claudia R. Pischke. 2019. "The Role of Continuous Glucose Monitoring, Diabetes Smartphone Applications, and Self-Care Behavior in Glycemic Control: Results of a Multi-National Online Survey" Journal of Clinical Medicine 8, no. 1: 109. https://doi.org/10.3390/jcm8010109
APA StyleKebede, M. M., Schuett, C., & Pischke, C. R. (2019). The Role of Continuous Glucose Monitoring, Diabetes Smartphone Applications, and Self-Care Behavior in Glycemic Control: Results of a Multi-National Online Survey. Journal of Clinical Medicine, 8(1), 109. https://doi.org/10.3390/jcm8010109