Untargeted Plasma Metabolomic Profiling in Patients with Major Depressive Disorder Using Ultra-High Performance Liquid Chromatography Coupled with Mass Spectrometry
Abstract
:1. Introduction
2. Results
2.1. Metabolites identiFication
2.2. Metabolomic Profiles of Controls and Patients before Treatment (C vs. MDD1)
2.3. Metabolomic Profiles of Patients, before and after Treatment (MDD1 vs. MDD2)
3. Discussion
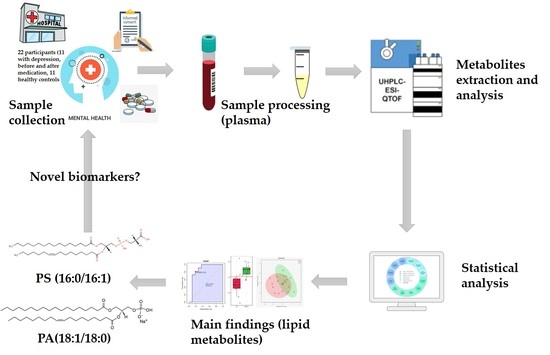
4. Materials and Methods
4.1. Study Population and Specimen Collection
4.2. Metabolites Extraction from Plasma
4.3. UHPLC-QTOF-(ESI+)-MS Analysis
4.4. Data Processing and Statistical Analysis
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Möller, H.J.; Seemüller, F.H.; Riedel, M. Time course of response and remission during antidepressant treatment. Medicographia 2009, 31, 118–125. [Google Scholar]
- Chiriţă, A.L.; Gheorman, V.; Bondari, D.; Rogoveanu, I. Current understanding of the neurobiology of major depressive disorder. Rom. J. Morphol. Embryol. 2015, 56, 651–658. [Google Scholar]
- Hays, R.D.; Wells, K.B.; Sherbourne, C.D.; Rogers, W.; Spritzer, K. Functioning and well-being outcomes of patients with depression compared with chronic general medical illnesses. Arc. Gen. Psych. 1995, 52, 11–19. [Google Scholar] [CrossRef]
- Mitchell, A.J.; Vaze, A.; Rao, S. Clinical diagnosis of depression in primary care: A meta-analysis. Lancet 2009, 374, 609–619. [Google Scholar] [CrossRef]
- Setoyama, D.; Kato, T.A.; Hashimoto, R.; Kunugi, H.; Hattori, K.; Hayakawa, K.; Kanba, S. Plasma Metabolites Predict Severity of Depression and Suicidal Ideation in Psychiatric Patients-A Multicenter Pilot Analysis. PLoS ONE 2016, 11, e0165267. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Belmaker, R.H.; Agam, G. Major depressive disorder. N. Engl. J. Med. 2000, 358, 55–68. [Google Scholar] [CrossRef] [Green Version]
- Sullivan, P.F.; Neale, M.C.; Kendler, K.S. Genetic epidemiology of major depression: Reviews and metaanalysis. Am. J. Psychiatry 2000, 157, 1552–1562. [Google Scholar] [CrossRef]
- Caspi, A.; Sugden, K.; Moffitt, T.E.; Taylor, A.; Craig, I.W.; Harrington, H.; Poulton, R. Influence of life stress on depression: Moderation by a polymorphism in the 5-HTT gene. Science 2003, 301, 386–389. [Google Scholar] [CrossRef] [PubMed]
- Roy, B.; Dunbar, M.; Shelton, R.C.; Dwivedi, Y. Identification of MicroRNA-124-3p as a Putative Epigenetic Signature of Major Depressive Disorder. Neuropsychopharmacology 2017, 42, 864–875. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Videbech, P.; Ravnkilde, B. Hippocampal volume and depression: A meta-analysis of MRI studies. Am. J. Psychiatry 2004, 161, 1957–1966. [Google Scholar] [CrossRef] [PubMed]
- Sheline, Y.I.; Gado, M.H.; Kraemer, H.C. Untreated depression and hippocampal volume loss. Am. J. Psychiatry 2003, 160, 1516–1518. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Anand, A.; Li, Y.; Wang, Y.; Wu, J.; Gao, S.; Bukhari, L.; Lowe, M.J. Activity and connectivity of brain mood regulating circuit in depression: A functional magnetic resonance study. Biol. Psychiatry 2003, 57, 1079–1088. [Google Scholar] [CrossRef] [PubMed]
- Sen, S.; Duman, R.; Sanacora, G. Serum brain-derived neurotrophic factor, depression, and antidepressant medications: Meta-analyses and implications. Biol. Psychiatry 2008, 64, 527–532. [Google Scholar] [CrossRef] [Green Version]
- Raison, C.L.; Miller, A.H. When not enough is too much: The role of insufficient glucocorticoid signaling in the pathophysiology of stress-related disorders. Am. J. Psychiatry 2003, 160, 1554–1565. [Google Scholar] [CrossRef] [PubMed]
- Zajecka, J.M. Treating depression to remission. J. Clin. Psychiatry 2003, 64, 7–12. [Google Scholar] [PubMed]
- Schmidt, H.D.; Shelton, R.C.; Duman, R.S. Functional biomarkers of depression: Diagnosis, treatment, and pathophysiology. Neuropsychopharmacology 2011, 36, 2375–2394. [Google Scholar] [CrossRef]
- First, M.B.; Gibbon, M. The Structured Clinical Interview for DSM-IV Axis I Disorders (SCID-I) and the Structured Clinical Interview for DSM-IV Axis II Disorders (SCID-II). In Comprehensive Handbook of Psychological Assessment; Personality assessment; Hilsenroth, M.J., Segal, D.L., Eds.; 2004; Volume 2, pp. 134–143. [Google Scholar]
- German, J.B.; Hammock, B.D.; Watkins, S.M. Metabolomics: Building on a century of biochemistry to guide human health. Metabolomics 2005, 1, 3–9. [Google Scholar] [CrossRef]
- Dettmer, K.; Aronov, P.A.; Hammock, B.D. Mass spectrometry-based metabolomics. Mass. Spectrom. Rev. 2007, 26, 51–78. [Google Scholar] [CrossRef]
- Quinones, M.P.; Kaddurah-Daouk, R. Metabolomics tools for identifying biomarkers for neuropsychiatric diseases. Neurobiol. Dis. 2009, 35, 165–176. [Google Scholar] [CrossRef]
- Pu, J.; Liu, Y.; Zhang, H.; Tian, L.; Gui, S.; Yu, Y.; Xie, P. An integrated meta-analysis of peripheral blood metabolites and biological functions in major depressive disorder. Mol. Psychiatry 2020, 10, 1–12. [Google Scholar] [CrossRef] [Green Version]
- Knowles, E.E.; Huynh, K.; Meikle, P.J.; Göring, H.H.H.; Olvera, R.L.; Mathias, S.R.; Glahn, D.C. The lipidome in major depressive disorder: Shared genetic influence for ether-phosphatidylcholines, a plasma-based phenotype related to inflammation, and disease risk. Eur. Psychiatry 2017, 43, 44–50. [Google Scholar] [CrossRef]
- Faria, R.; Santana, M.M.; Aveleira, C.A.; Simões, C.; Maciel, E.; Melo, T.; Domingues, M.R.M. Alterations in phospholipidomic profile in the brain of mouse model of depression induced by chronic unpredictable stress. Neuroscience 2014, 273, 1–11. [Google Scholar] [CrossRef]
- Liu, X.; Li, J.; Zheng, P.; Zhao, X.; Zhou, C.; Hu, C.; Xu, G. Plasma lipidomics reveals potential lipid markers of major depressive disorder. Anal. Bioanal. Chem. 2016, 408, 6497–6507. [Google Scholar] [CrossRef] [PubMed]
- Walther, A.; Cannistraci, C.V.; Simons, K.; Durán, C.; Gerl, M.J.; Wehrli, S.; Kirschbaum, C. Lipidomics in Major Depressive Disorder. Front. Psychiatry 2018, 9, 459. [Google Scholar] [CrossRef] [PubMed]
- Bandu, R.; Lee, H.J.; Lee, H.M.; Ha, T.H.; Lee, H.J.; Kim, S.J.; Kim, K.P. Liquid chromatography/mass spectrometry-based plasma metabolic profiling study of escitalopram in subjects with major depressive disorder. J. Mass. Spectrom. 2018, 53, 385–399. [Google Scholar] [CrossRef] [PubMed]
- Hashimoto, K. Metabolomics of Major Depressive Disorder and Bipolar Disorder: Overview and Future Perspective. Adv. Clin. Chem. 2018, 84, 81–99. [Google Scholar] [PubMed]
- Sussulini, A.; Prando, A.; Maretto, D.A.; Poppi, R.J.; Tasic, L.; Banzato, C.E.M.; Arruda, M.A.Z. Metabolic profiling of human blood serum from treated patients with bipolar disorder employing 1H NMR spectroscopy and chemometrics. Anal. Chem. 2009, 81, 9755–9763. [Google Scholar] [CrossRef]
- Van Meer, G.; Voelker, D.R.; Feigenson, G.W. Membrane lipids: Where they are and how they behave. Nat. Rev. Mol. Cell. Biol. 2008, 9, 112–124. [Google Scholar] [CrossRef] [PubMed]
- Quehenberger, O.; Dennis, E.A. The human plasma lipidome. N. Engl. J. Med. 2011, 365, 1812–1823. [Google Scholar] [CrossRef]
- Sud, M.; Fahy, E.; Cotter, D.; Brown, A.; Dennis, E.A.; Glass, C.K.; Subramaniam, S. LMSD: LIPID MAPS structure database. Nucleic. Acids. Res. 2007, 35, D527–D532. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Mondelli, V.; Vernon, A.C.; Turkheimer, F.; Dazzan, P.; Pariante, C.M. Brain microglia in psychiatric disorders. Lancet Psychiatry 2017, 4, 563–572. [Google Scholar] [CrossRef] [Green Version]
- Demirkan, A.; Isaacs, A.; Ugocsai, P.; Liebisch, G.; Struchalin, M.; Rudan, I.; van Duijn, C.M. Plasma phosphatidylcholine and sphingomyelin concentrations are associated with depression and anxiety symptoms in a Dutch family-based lipidomics study. Ays. J. Psychiatr. Res. 2013, 47, 357–362. [Google Scholar] [CrossRef] [PubMed]
- Olguner Eker, Ö.; Özsoy, S.; Eker, B.; Doğan, H. Metabolic Effects of Antidepressant Treatment. Noro. Psikiyatr. Ars. 2017, 54, 49–56. [Google Scholar] [CrossRef] [Green Version]
- Mahmoudian Dehkordi, S.; Ahmed, A.T.; Bhattacharyya, S.; Han, X.; Baillie, R.A.; Arnold, M.; Kaddurah-Daouk, R. Alterations in Acylcarnitines, amines, and lipids inform about mechanism of action of citalopram/escitalopram in major depression. bioRxiv 2020, 1–14. [Google Scholar] [CrossRef] [Green Version]
- Enatescu, V.R.; Papava, I.; Enatescu, I.; Antonescu, M.; Anghel, A.; Seclaman, E.; Marian, C. Circulating Plasma Miro RNAs in Patients with Major Deppresive Disorder Treated with Antidepressants: A Pilot Study. Psychiatry Investig. 2016, 13, 549–557. [Google Scholar] [CrossRef] [Green Version]




| No. | m/z [M+H]+ | Metabolites Identification |
|---|---|---|
| 1 | 256.275 | Palmitamide |
| 2 | 301.154 | Andrenosterone |
| 3 | 304.274 | Arachidonyl alanine, Palmitoyl ethanolamine |
| 4 | 313.288 | Eicosanoic (arachidic) acid |
| 5 | 318.255 | Leucyl-Tryptophan |
| 6 | 331.296 | Deoxycorticosterone |
| 7 | 339.316 | 11,12-DiHETrE |
| 8 | 341.321 | 9-Hexadecenoylcholine |
| 9 | 347.141 | Corticosterone |
| 10 | 348.326 | Adenosine monophosphate |
| 11 | 353.282 | Prostaglandin E2/D2 |
| 12 | 357.327 | Prostaglandin F1a |
| 13 | 359.33 | Tetracosapentaenoic acid |
| 14 | 369.368 | Thromboxane B3 |
| 15 | 381.315 | Sphinganine -1 Phosphate |
| 16 | 467.405 | Cholesterol sulfate |
| 17 | 483.402 | 11-beta-Hydroxyandrosterone-3-glucuronide |
| 18 | 496.365 | LPC (16:0) |
| 19 | 518.347 | LPC (18:3) |
| 20 | 520.366 | LPC (18:2) |
| 21 | 522.381 | LPC (18:1) |
| 22 | 524.397 | LPC (18:0) |
| 23 | 542.349 | LPC (20:5) |
| 24 | 544.366 | LPC (20:4) |
| 25 | 563.578 | DG( 18:2/14:1/0:0) |
| 26 | 609.549 | DG (17:1/18:0/0:0) [iso2] |
| 27 | 623.529 | Ceramide (d18:1/22:0) |
| 28 | 625.545 | Ceramide (d18:0/22:0) |
| 29 | 626.48 | Leukotriene C4 |
| 30 | 639.526 | PA(32:5) |
| 31 | 641.541 | DG (18:1/20:5/0:0) |
| 32 | 663.488 | PG (14:1/14:1) |
| 33 | 677.021 | SM (d18:0/14:0) |
| 34 | 679.019 | Cer (d18:1/26:0) |
| 35 | 679.547 | 20:1 Cholesterol ester |
| 36 | 701.529 | PA (18:1/18:1) |
| 37 | 703.611 | PA (18:1/18:0) |
| 38 | 712.521 | PE (16:0/18:4) |
| 39 | 732.591 | SM (d18:1/18:0) |
| 40 | 734.504 | SM (d18:0/18:0) |
| 41 | 734.607 | PS (16:0/16:1) |
| 42 | 739.57 | PA (21:0/18:4) |
| 43 | 756.593 | PS (16:1/18:3) |
| 44 | 758.61 | PS (16:1/18:2) |
| 45 | 760.624 | PS (16:1/18:1) |
| 46 | 761.553 | TG (13:0/16:1/16:1) [iso3] |
| 47 | 768.629 | PC (18:2/17:2) |
| 48 | 772.624 | PG (18:1/18:3) |
| 49 | 780.593 | PC (18:3/18:2) |
| 50 | 782.611 | PC (18:2/18:2) |
| 51 | 784.625 | PC (18:1/18:2) |
| 52 | 786.642 | PC (18:1/18:1) |
| 53 | 792.636 | PS (18:0/18:0) |
| 54 | 806.612 | PS (18:3/20:4) |
| 55 | 808.626 | PS (18:2/20:4) |
| 56 | 810.643 | PS (18:1/20:4) |
| 57 | 814.62 | PS (18:1/20:4) |
| 58 | 825.61 | TG (16:0/16:0/18:2 (9Z,12Z)) [iso3] |
| 59 | 834.644 | PC (18:0/22:6) |
| 60 | 905.726 | TG (16:0/18:0/21:0) [iso6] |
| 61 | 927.71 | TG (18:1/19:0/20:2) [iso6] |
| No. | Metabolite Identification [M+H]+ | RT (min) | m/z | VIP | p-value | FC | FDR |
|---|---|---|---|---|---|---|---|
| 1 | PS (16:0/16:1) | 10.5 | 734.607 | 2.813 | <0.001 | 1.699 | 0.009 |
| 2 | PS (18:1/20:4) | 10.39 | 810.643 | 1.887 | 0.133 | 1.283 | 0.888 |
| 3 | PC (18:2/18:2) | 10.24 | 782.611 | 1.884 | 0.065 | 1.272 | 0.717 |
| 4 | PA (18:1/18:0) | 8.93 | 703.611 | 1.859 | 0.005 | 2.508 | 0.086 |
| 5 | Deoxycorticosterone | 8.11 | 331.296 | 1.406 | 0.401 | 0.826 | 0.888 |
| 6 | LPC (18:2) | 9.33 | 520.366 | 1.358 | 0.217 | 0.842 | 0.888 |
| 7 | PG (18:1/18:3) | 10.37 | 772.624 | 1.308 | 0.332 | 1.218 | 0.888 |
| 8 | LPC (20:4) | 9.37 | 544.366 | 1.158 | 0.401 | 1.231 | 0.888 |
| Molecule | AUC |
|---|---|
| PS (16:0/16:1) | 0.876 |
| PA (18:1/18:0) | 0.777 |
| PS (18:1/20:4) | 0.678 |
| No. | Metabolite Identification [M+H]+ | RT (min) | m/z | VIP | p-Value | FC | FDR |
|---|---|---|---|---|---|---|---|
| 1 | PS(18:3/20:4) | 10.12 | 806.612 | 2.376 | 0.028 | 0.720 | 0.926 |
| 2 | Deoxycorticosterone | 8.11 | 331.296 | 1.782 | 0.365 | 1.272 | 0.964 |
| 3 | PC (18:1/18:1) | 10.45 | 786.642 | 1.761 | 0.171 | 1.174 | 0.964 |
| 4 | PC (18:2/17:2) | 10.85 | 768.629 | 1.656 | 1.000 | 1.011 | 0.964 |
| 5 | PG (18:1/18:3)/ PG (18:2/18:2) | 10.37 | 772.624 | 1.573 | 0.438 | 0.804 | 0.964 |
| 6 | Sphinganine 1-phosphate | 8.27 | 381.315 | 1.546 | 0.171 | 1.169 | 0.964 |
| 7 | PC (18:1/18:3)/ PC (18:2/18:2) | 10.24 | 782.611 | 1.431 | 0.193 | 0.853 | 0.964 |
| 8 | LPC (20:4) | 9.37 | 544.366 | 1.232 | 0.748 | 0.824 | 0.964 |
| 9 | Adenosine monophosphate | 8.10 | 348.326 | 1.063 | 0.964 | ||
| 10 | LPC (20:5) | 9.33 | 542.349 | 0.988 | 0.438 | 0.847 | 0.964 |
| 11 | LPC (18:2) | 9.33 | 520.366 | 0.919 | 0.964 |
| Name | AUC | Changes MDD2 vs. MDD1 |
|---|---|---|
| PS (18:3/20:4) | 0.785 | Decrease |
| Sphinganine 1-phosphate | 0.678 | Decrease |
| PC (18:1/18:1) | 0.678 | Increase |
| PC (18:1/18:3) or PC (18:2/18:2) | 0.669 | Decrease |
| PC (18:1/18:2) | 0.669 | Increase |
| PS (16:1/18:1) | 0.669 | Decrease |
| Variables | MDD Patients (n = 11) | Healthy Controls (n = 11) |
|---|---|---|
| Age in years (median) | 43.81 | 45 |
| Gender | ||
| Male | 3 | 3 |
| Female | 8 | 8 |
| HDRS-17 (median score) | ||
| Before treatment | 23.27 | |
| After treatment | 5.81 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Homorogan, C.; Nitusca, D.; Enatescu, V.; Schubart, P.; Moraru, C.; Socaciu, C.; Marian, C. Untargeted Plasma Metabolomic Profiling in Patients with Major Depressive Disorder Using Ultra-High Performance Liquid Chromatography Coupled with Mass Spectrometry. Metabolites 2021, 11, 466. https://doi.org/10.3390/metabo11070466
Homorogan C, Nitusca D, Enatescu V, Schubart P, Moraru C, Socaciu C, Marian C. Untargeted Plasma Metabolomic Profiling in Patients with Major Depressive Disorder Using Ultra-High Performance Liquid Chromatography Coupled with Mass Spectrometry. Metabolites. 2021; 11(7):466. https://doi.org/10.3390/metabo11070466
Chicago/Turabian StyleHomorogan, Claudia, Diana Nitusca, Virgil Enatescu, Philip Schubart, Corina Moraru, Carmen Socaciu, and Catalin Marian. 2021. "Untargeted Plasma Metabolomic Profiling in Patients with Major Depressive Disorder Using Ultra-High Performance Liquid Chromatography Coupled with Mass Spectrometry" Metabolites 11, no. 7: 466. https://doi.org/10.3390/metabo11070466
APA StyleHomorogan, C., Nitusca, D., Enatescu, V., Schubart, P., Moraru, C., Socaciu, C., & Marian, C. (2021). Untargeted Plasma Metabolomic Profiling in Patients with Major Depressive Disorder Using Ultra-High Performance Liquid Chromatography Coupled with Mass Spectrometry. Metabolites, 11(7), 466. https://doi.org/10.3390/metabo11070466