1. Introduction
Clinical pharmacy training is novel concept in Pakistan, a developing country where the practice of pharmacy is in embryonic stages. In 2004, the higher authorities upgraded the pharmacy curriculum from a 4 year degree of Bachelor of Pharmacy
(B.Pharm) to 5 year degree of Doctor of Pharmacy
(Pharm.D) [
1]. The purpose of uprgrading the curriculum was to address the health care related issues and to empower the pharmacists in the field of health care. For this purpose, patient oriented courses such as clinical pharmacy along with real time practice based clinical pharmacy clerkship training in hospital were added. It was aimed at empowering the undergraduate students in pharmacy to learn the issues arising in the health care system and to promote clinical pharmacy practice in a real time clinical setting. In this regard, the pharmacy educational institutes took the first step in Pakistan, starting the clinical pharmacy clerkships training for the students [
2,
3].
The novel concept gave an opportunity for the students to learn and acquaint the practice of pharmacy and improve their clinical skills however, there were few occasions where it was observed that the clerkship led to some undesirable outcomes such as workplace intrusion, ethical issues and behavioral misconduct.
The underlying problem was the fact that the health care environment of Pakistan is urban-based curative care model where the physicians are generally viewed as having the authority and decision making [
4]. In addition, previous studies have reported the threat perception exists in the mind of health care professionals HCPs especially physicians that clinical pharmacists are intruding in the health related activities of allied health professionals.
The problem with the clerkship was identified as inadequate knowledge of the pharmacy students related to workplace ethics, responsibilities and practice. Moreover, they were also observed to be struggling to communicate with the HCPs.
The deficiency in the practiced based curriculum was identified as lack of knowledge related to clinical pharmacy ethics, practice, therapeutics and research informatics. For this purpose a series of modules were included in the present curriculum. The idea was derived from the clinical pharmacy practice in United Kingdom [
5]. Each module targeted a specific area of the course.
2. Design
The design of the updated curriculum included four modules of clinical pharmacy practice knowledge related to workplace communication with HCPs, allied health professionals, patients and their caregivers were included followed by a general account of good health practices in hospitals. The therapeutics and evidence base knowledge was taught along with a research-oriented insight to the health care issues. An account of each module is given in
Table 1.
The rationale behind the sequencing of each modules in such order was the fact that when, the students exposed for the first time to the practice of clinical pharmacy in a health care setting, they appear perplexed and in need of knowledge of work ethics. It is at that this time that they specifically need knowledge about the work ethics. EBI started with ethics module to minimize the chance of any mismanagement and unethical conduct. Moreover, they also need to know the practice based protocols that are followed in the health care setting and for this purpose; the pharmacy practice module was added in second session in the EBI program tabulated in
Table 1. The advance evidence based knowledge related to therapeutics and pharmacotherapy is taught after the aforesaid when the student has developed a firm grip on the working environment and basic concepts of pharmacy practice. Addition of therapeutics component at this point would complement the theoretical knowledge with practical one. Finally, the placement of research informatics as the last module was aimed at objectively galvanizing a research culture among the students. The rationale behind placing research informatics in the end was the fact that that it was most suitable to incite them to critically evaluate their knowledge in order to investigate various issues in the health care system.
Table 1.
Modules for clinical pharmacy clerkships Evidence Based Improvement (EBI) Program.
Table 1.
Modules for clinical pharmacy clerkships Evidence Based Improvement (EBI) Program.
| Session Number | Module Name | Objective | Learning Strategy | Evaluation Method |
|---|
| 1 | Ethics | To help the student get acquainted to the work place environment | Taught lecture given on the responsibilities of pharmacists and ethics of health care system | Practical observation of students during clerkship and marking their progress |
| 2 | Pharmacy Practice | To help the students to follow the protocols in healthcare environment | Taught lecture on clinical pharmacy, disease state management and pharmaceutical care plan and practical exercise by using FARM notes | Weekly evaluation of students‘ ability to formulate a care plan for a random patient in a health care setting based on FARM note |
| 3 | Therapeutics | Empowering students in applied clinical knowledge | Additional lectures were given regarding drugs‘ pharmacology, Adverse drugs reactions (ADRs), interactions and their use in pharmacotherapy of various diseases coupled with weekly case discussions with each student on a random clinical scenario of any patient in health care setting | Structured questions were asked from each student weekly based on a random clinical case in health care setting. Viva and quizzes were conducted every two months |
| 4 | Research Informatics | Galvanizing a research culture | Lectures on basic concept of research, types and terminologies, scientific writing and how to write manuscripts were taught followed by personal review of students’ manuscripts and individualized guidance | Manuscripts genuinely written and relevant were evaluated for their suitability and were given a go ahead for submission to related scientific journal in the field |
3. Expected Outcomes and Learning Objectives
It was expected that by improved curriculum the student will learn about the ethical issues arising from such practices and be better equipped to understand the protocols. Moreover, prevent any untoward incident of intrusion in routine activity and indulging in any misconduct in the field. The students would be better learners. Over the long run it can help to produce professional clinical pharmacists which will in turn dispel the wrong perception of the clinical pharmacists as intruders and as a professional threat.
4. Educational Environment
The educational environment for the practice of the clinical pharmacy training program comprised of large tertiary care hospitals which served as excellent spot for practicing pharmacy skills related to clinical and hospital background and was found suitable to execute the EBI initiative.
5. Contents
Since the curriculum did not include lessons in ethics therefore a module on ethics was incorporated to help the undergraduates get acquainted to the work place atmosphere. The lessons consisted of small tutorials and lectures on work place ethics and the roles of HCPs. A routine unit exercise included the practical observation of behavior of students during their clerkship. The module of practice was added to empower the students in clinical activities with respect to patient health care. Taught lectures coupled with practical demonstration were given to the students followed by weekly evaluation in a practice-based scenario in hospital by a FARM note [
6]. At this point the targets of incorporating and facilitating the students in the health care settings were hypothesized to be achieved.
The next step is to empower the students to actively participate in the clinical related discussions with the consultants and the GPs as well as galvanizing a research culture among them. The module of therapeutics is added to supplement the practical clinical knowledge of the students. Structured lectures and problem based learning session form the core of this module. The research informatics is focused on galvanizing a research culture among students and lectures related to research are given and clinical research projects are given to the students. The projects were based on pharmacotherapy and disease state management of a random patient whose condition was subjected to critical investigation by the student for a period of 2 weeks (after taking patient consent) and written in the form of a case study, after which it was evaluated by clinical pharmacist and if recommended, a manuscript was then written by students. The details of materials and methods are available upon request.
6. Evaluation and Assessment Data
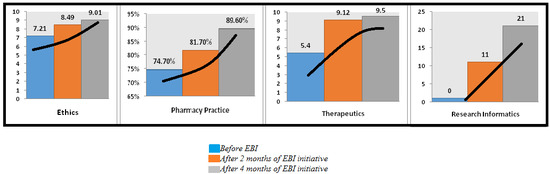
An evaluation was conducted before the initiation of the EBI initiative to set a baseline and to note down the prospective benefits of the program. A total of N = 42 students were available after consent. The maximum score for ethics and therapeutics was 10; however pharmacy practice encompassed 100. The students obtained marks which were also moderated by external moderator to eliminate bias. The marking criterion for research informatics was based on number of publications. The marks of the students were entered in to SPSS (Statistical package for social sciences) version 19 and mean scores and standard deviations were obtained.
Table 2 presents the results of students before and after initiation of the EBI program.
Table 2.
Summary of Students’ performance.
Table 2.
Summary of Students’ performance.
| Session No. | Module | Outcomes | Before EBI | 1st Observation (2 Months) | 2nd Observation (4 Months) |
|---|
| Mean Score | SD | Mean Score | SD | Mean Score | SD |
|---|
| 1 | Ethics | Observation Score out of 10 | 7.21 | 1.4 | 8.49 | 0.7 | 9.01 | 0.4 |
| 2 | Pharmacy Practice | Examination out of 100% | 74.7% | 13.7 | 81.7% | 8.9 | 89.6% | 3.6 |
| 3 | Therapeutics | Clinical Evaluation out of 10 | 5.4 | 0.9 | 9.12 | 0.7 | 9.5 | 0.5 |
| 4 | Research informatics | Research Publications | 0 | - | 11 | - | 21 | - |
7. Discussion
Clinical pharmacy training program is an innovative concept of practice based learning of clinical pharmacy and a novel concept in developing countries such as Pakistan. It was recently experimented and launched with an objective of harmonizing a pharmacy undergraduate with the actual healthcare setting protocols. However, few things that were not realized at the time of instigation were the issues of behavior and ethics arising from the maiden exposure of the students and the assessment of theoretical and practical knowledge gap. The educational authorities took the first step to incorporate the undergraduate students in the process however, did not pay attention on the aftermath. Although the trend is changing, initially the perception of the health care professionals towards pharmacists were not that much welcoming in the regional context [
7,
8].
However, the issues were investigated and the shortcomings, deficiencies and limitations were carefully studied and assessed. The abovementioned improvement plan was then formulated by the author and subjected to the evaluation of the higher authorities which when given the go ahead was implemented in the current clinical pharmacy curriculum. The idea inspiration was the clinical pharmacy programs that are offered in the UK. However, a regional model such as clinical pharmacy education development model of China was also considered [
5,
9]. The first review of the outcomes anticipated after the EBI is due in 6 months time.
8. Conclusions
This concept paper highlights the areas for improvement in the pharmacy curriculum of a developing country like Pakistan. It also provides a solution to address the issues and has the potential to serve as an evidence base for the other developing countries which are in transition in context of evolving pharmacy education.
Supporting Information
This concept paper is based on the evidence based improvement EBI plan initiated by the author at a pharmacy education institute and currently is in practice. The improvement plan details, module details, evaluation methods and materials are exempted from the review and are approved by the official body to be implemented in the present curriculum and expected outcomes are awaited.
Acknowledgement
The author acknowledges and extends his gratitude to the students of Pharm.D Batch 07 of the Faculty of Pharmacy, Ziauddin University for their support.
Conflicts of Interest
The author declares no conflict of interest.
References
- B Pharmacy Course to be upgraded. Available online: http://www.dawn.com/news/346644/b-pharmacy-course-to-be-upgraded (accessed on 10 April 2014).
- Aslam, N.; Ahmed, K.Z. Clinical pharmacy clerkship in Pakistan: A leap from paper to practice. Innov. pharm. 2011, 2, 1–4. [Google Scholar]
- Khan, M.U. A new paradigm in clinical pharmacy teaching in Pakistan. Am. J. Pharm. Educ. 2011, 75, 166. [Google Scholar] [CrossRef] [PubMed]
- Gera, N. Pakistan’s health care system under structural adjustment. Lahore J. Econ. 2003, 8, 65–81. [Google Scholar]
- Medicines Management MSc. Available online: http://www.sunderland.ac.uk/courses/appliedsciences/postgraduate/medicines-management/ (accessed on 10 April 2014).
- Ives, T.J.; Canaday, B.R.; Yarborough, P.C. Chapter 5. Documentation of pharmacists interventions. Instructor’s Guide to Accompany Pharmacotherapy Case Book, 5th ed. Available online: http://facpub.stjohns.edu/~sees/FMRotation/CarePlans.pdf (accessed on 05 May 2014).
- Adnan, S.; Tanwir, S.; Abbas, A.; Beg, A.E.; Sabah, A.; Safdar, H.; Maria Moin, M.; Fatima, R.; Mobeen, K.; Shams, M. Perception of physicians regarding patient counselling by pharmacist: A blend of quantitative and qualitative insight. Int. J. Pharm. Ther. 2014, 5, 117–121. [Google Scholar]
- Abbas, A. The catch-22 of pharmacy practice in Pakistan’s pharmacy education. Pharmacy 2014, 2, 202–204. [Google Scholar] [CrossRef]
- Ryan, M.; Shao, H.; Yang, L.; Nie, X.Y.; Zhai, S.D.; Shi, L.W.; Lubawy, W.C. Clinical Pharmacy Education in China. Am. J. Pharm. Educ. 2008, 72, 129. [Google Scholar] [CrossRef] [PubMed]
© 2014 by the authors; licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution license (http://creativecommons.org/licenses/by/4.0/).