Neurodevelopmental Disorders: Past, Present, and Future
Abstract
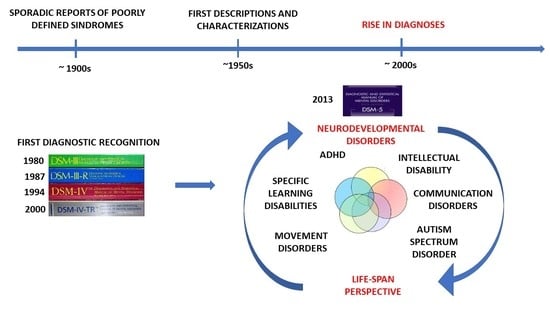
:1. Introduction: The Shift in Perspective
2. Historical Background
3. Neurodevelopmental Disorders Today
Comorbidities
4. Future Perspectives
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Atladóttir, H.Ó.; Parner, E.T.; Schendel, D.; Dalsgaard, S.; Thomsen, P.H.; Thorsen, P. Time Trends in Reported Diagnoses of Childhood Neuropsychiatric Disorders: A Danish Cohort Study. Available online: http://archpedi.jamanetwork.com/article.aspx?doi=10.1001/archpedi.161.2.193 (accessed on 1 November 2018).
- Etzwiler, D.D. Chronic Care: A Need in Search of a System. Diabetes Educ. 1997, 23, 569–573. [Google Scholar] [CrossRef] [PubMed]
- Cainelli, E.; Vedovelli, L. Over-specialization versus synergy in neuroscience: Professionals’ integration is more than the sum of its parts. Neural Regen. Res. 2021, 16, 2232–2233. [Google Scholar] [CrossRef] [PubMed]
- Leutz, W.N. Five Laws for Integrating Medical and Social Services: Lessons from the United States and the United Kingdom. Milbank Q. 1999, 77, 77–110. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Faa, G.; Manchia, M.; Pintus, R.; Gerosa, C.; Marcialis, M.A.; Fanos, V. Fetal programming of neuropsychiatric disorders. Birth Defects Res. Part C—Embryo Today Rev. 2016, 108, 207–223. [Google Scholar] [CrossRef]
- Godoy, L.D.; Umeoka, E.H.L.; Ribeiro, D.E.; Santos, V.R.; Antunes-Rodrigues, J.; Joca, S.R.L.; Garcia-Cairasco, N. Multimodal early-life stress induces biological changes associated to psychopathologies. Horm. Behav. 2018, 100, 69–80. [Google Scholar] [CrossRef] [PubMed]
- von Baes, C.W.; Martins, C.M.S.; de Carvalho Tofoli, S.M.; Juruena, M.F. Early life stress in depressive patients: HPA axis response to GR and MR agonist. Front. Psychiatry 2014, 5, 2. [Google Scholar] [CrossRef] [Green Version]
- Eapen, V.; Črnčec, R. DSM 5 and child psychiatric disorders: What is new? What has changed? Asian J. Psychiatr. 2014, 11, 114–118. [Google Scholar] [CrossRef]
- Doernberg, E.; Hollander, E. Neurodevelopmental Disorders (ASD and ADHD): DSM-5, ICD-10, and ICD-11. CNS Spectr. 2016, 21, 295–299. [Google Scholar] [CrossRef] [Green Version]
- Polanczyk, G.; De Lima, M.S.; Horta, B.L.; Biederman, J.; Rohde, L.A. The worldwide prevalence of ADHD: A systematic review and metaregression analysis. Am. J. Psychiatry 2007, 164, 942–948. [Google Scholar] [CrossRef]
- GBD 2019 Mental Disorders Collaborators. Global, regional, and national burden of 12 mental disorders in 204 countries and territories, 1990–2019: A systematic analysis for the Global Burden of Disease Study 2019. Lancet Psychiatry 2022, 9, 137–150. [Google Scholar] [CrossRef]
- Matthews, M.; Nigg, J.; Fair, D. Attention Deficit Hyperactivity Disorder. Curr. Top Behav. Neurosci. 2014, 16, 235–266. [Google Scholar] [PubMed] [Green Version]
- Hinshelwood, J. Word-Blindness and Visual Memory. Lancet 1896, 147, 196. [Google Scholar] [CrossRef]
- Kirk, S.A.; Bateman, B. Diagnosis and Remediation of Learning Disabilities. Except. Child. 1962, 29, 73–78. [Google Scholar] [CrossRef]
- McArthur, G.; Eve, P.M.; Jones, K.; Banales, E.; Kohnen, S.; Anandakumar, T.; Larsen, L.; Marinus, E.; Wang, H.-C.; Castles, A. Phonics training for English-speaking poor readers. Cochrane Database Syst. Rev. 2012, 12, CD009115. [Google Scholar] [CrossRef] [PubMed]
- Yuzaidey, N.A.M.; Din, N.C.; Ahmad, M.; Ibrahim, N.; Razak, R.A.; Harun, D. Interventions for children with dyslexia: A review on current intervention methods. Med. J. Malaysia 2018, 73, 311–320. [Google Scholar] [CrossRef]
- Franceschini, S.; Bertoni, S.; Gianesini, T.; Gori, S.; Facoetti, A. A different vision of dyslexia: Local precedence on global perception. Sci. Rep. 2017, 7, 17462. [Google Scholar] [CrossRef] [Green Version]
- Fletcher, J.M.; Grigorenko, E.L. Neuropsychology of learning disabilities: The past and the future. J. Int. Neuropsychol. Soc. 2017, 23, 930–940. [Google Scholar] [CrossRef]
- Griffiths, Y.; Stuart, M. Reviewing evidence-based practice for pupils with dyslexia and literacy difficulties. J. Res. Read. 2013, 36, 96–116. [Google Scholar] [CrossRef]
- Barkley, R.A.; Peters, H. The Earliest Reference to ADHD in the Medical Literature? Melchior Adam Weikard’s Description in 1775 of “Attention Deficit” (Mangel der Aufmerksamkeit, Attentio Volubilis). J. Atten. Disord. 2012, 16, 623–630. [Google Scholar] [CrossRef]
- Fay, T. Psychopathology and Education of the Brain-Injured Child Volume II; Grune and Stratton: New York, NY, USA, 1956; Volume 113. [Google Scholar]
- Del Barrio, V. Diagnostic and Statistical Manual of Mental Disorders; American Psychiatric Association, Ed.; Elsevier: Washington DC, USA, 2016; ISBN 9780128093245. [Google Scholar]
- Thapar, A.; Cooper, M. Attention deficit hyperactivity disorder. Lancet 2016, 387, 1240–1250. [Google Scholar] [CrossRef]
- Kena, G.; Hussar, W.; McFarland, J.; de Brey, C.; Musu-Gillette, L.; Wang, X.; Zhang, J.; Rathbun, A.; Wilkinson-Flicker, S.; Diliberti, M.; et al. The Condition of Education 2016; NCES 2016–144; United States Department of Education: Washington, DC, USA, 2016; p. 347. [CrossRef]
- Sansavini, A.; Simion, F. Aumento delle diagnosi di Disturbi Specifici dell’Apprendimento in Italia: Quali fattori concorrono nel determinare tale aumento? Psicol. Clin. dello Svilupp. 2019, 23, 265–281. [Google Scholar] [CrossRef]
- Cainelli, E.; Bisiacchi, P.S. Diagnosis and Treatment of Developmental Dyslexia and Specific Learning Disabilities: Primum Non Nocere. J. Dev. Behav. Pediatr. 2019, 40, 558–562. [Google Scholar] [CrossRef] [PubMed]
- Lucangeli, D.; Perini, N. Aumento di diagnosi di Disturbi Specifici dell’Apprendimento in Italia: Tra maggiore consapevolezza e attenzione ai falsi positivi. Psicol. Clin. dello Svilupp. 2020, 24, 97–100. [Google Scholar] [CrossRef]
- Angela, E.; Germinario, P.; Arcieri, R.; Marzi, M.; Panei, P.; Vella, S. Registro Nazionale dell’ADHD Dati dal 2007 al 2016; ISS: Rome, Italy, 2016. [Google Scholar]
- Novara, D. L’immaturità infantile non può diventare una diagnosi. Psicol. Clin. dello Svilupp. 2020, 24, 91–96. [Google Scholar] [CrossRef]
- Epstein, J.N.; Kelleher, K.J.; Baum, R.; Brinkman, W.B.; Peugh, J.; Gardner, W.; Lichtenstein, P.; Langberg, J. Variability in ADHD care in community-based pediatrics. Pediatrics 2014, 134, 1136–1143. [Google Scholar] [CrossRef] [Green Version]
- Evans, W.N.; Morrill, M.S.; Parente, S.T. Measuring inappropriate medical diagnosis and treatment in survey data: The case of ADHD among school-age children. J. Health Econ. 2010, 29, 657–673. [Google Scholar] [CrossRef]
- Office for Standards in Education (Ofsted) The special educational needs and disability review. Ofsted 2010, 090221, 1–94.
- Amato, M.P.; Goretti, B.; Ghezzi, A.; Hakiki, B.; Niccolai, C.; Lori, S.; Moiola, L.; Falautano, M.; Viterbo, R.G.; Patti, F.; et al. Neuropsychological features in childhood and juvenile multiple sclerosis: Five-year follow-up. Neurology 2014, 83, 1432–1438. [Google Scholar] [CrossRef]
- Suppiej, A.; Cainelli, E. Cognitive dysfunction in pediatric multiple sclerosis. Neuropsychiatr. Dis. Treat. 2014, 10, 1385–1392. [Google Scholar] [CrossRef] [Green Version]
- Cainelli, E.; Vedovelli, L.; Wigley, I.L.C.M.; Bisiacchi, P.S.; Suppiej, A. Neonatal spectral EEG is prognostic of cognitive abilities at school age in premature infants without overt brain damage. Eur. J. Pediatr. 2021, 180, 909–918. [Google Scholar] [CrossRef]
- Cainelli, E.; Bisiacchi, P.S.; Cogo, P.; Padalino, M.; Simonato, M.; Vergine, M.; Lanera, C.; Vedovelli, L. Detecting neurodevelopmental trajectories in congenital heart diseases with a machine-learning approach. Sci. Rep. 2021, 11, 2574. [Google Scholar] [CrossRef] [PubMed]
- Vedovelli, L.; Cogo, P.; Cainelli, E.; Suppiej, A.; Padalino, M.; Tassini, M.; Simonato, M.; Stellin, G.; Carnielli, V.P.; Buonocore, G.; et al. Pre-surgery urine metabolomics may predict late neurodevelopmental outcome in children with congenital heart disease. Heliyon 2019, 5, e02547. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Cainelli, E.; Nosadini, M.; Sartori, S.; Suppiej, A. Neuropsychological and Psychopathological Profile of Anti-NMDAR Encephalitis: A Possible Pathophysiological Model for Pediatric Neuropsychiatric Disorders. Arch. Clin. Neuropsychol. 2019, 34, 1309–1319. [Google Scholar] [CrossRef] [PubMed]
- Cainelli, E.; Arrigoni, F.; Vedovelli, L. White matter injury and neurodevelopmental disabilities: A cross-disease (dis)connection. Prog. Neurobiol. 2020, 193, 101845. [Google Scholar] [CrossRef] [PubMed]
- Cainelli, E.; Vedovelli, L.; Gregori, D.; Suppiej, A.; Padalino, M.; Cogo, P.; Bisiacchi, P. Embrace the Complexity: Agnostic Evaluation of Children’s Neuropsychological Performances Reveals Hidden Neurodevelopment Patterns. Children 2022, 9, 775. [Google Scholar] [CrossRef] [PubMed]
- Piper, B.J.; Ogden, C.L.; Simoyan, O.M.; Chung, D.Y.; Caggiano, J.F.; Nichols, S.D.; McCall, K.L. Trends in use of prescription stimulants in the United States and territories, 2006 to 2016. PLoS ONE 2018, 13, e0206100. [Google Scholar] [CrossRef] [Green Version]
- Visser, S.N.; Danielson, M.L.; Bitsko, R.H.; Holbrook, J.R.; Kogan, M.D.; Ghandour, R.M.; Perou, R.; Blumberg, S.J. Trends in the parent-report of health care provider-diagnosed and medicated attention-deficit/hyperactivity disorder: United States, 2003–2011. J. Am. Acad. Child Adolesc. Psychiatry 2014, 53, 34–46.e2. [Google Scholar] [CrossRef] [Green Version]
- Bachhuber, M.A.; Hennessy, S.; Cunningham, C.O.; Starrels, J.L. Increasing benzodiazepine prescriptions and overdose mortality in the United States, 1996–2013. Am. J. Public Health 2016, 106, 686–688. [Google Scholar] [CrossRef]
- Cumming, J.M. Integrated Care in New Zealand. Int. J. Integr. Care 2011, 21, 17. [Google Scholar] [CrossRef]
- Gabrieli, J.D.E. Dyslexia: A new synergy between education and cognitive neuroscience. Science 2009, 325, 280–283. [Google Scholar] [CrossRef]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Cainelli, E.; Bisiacchi, P. Neurodevelopmental Disorders: Past, Present, and Future. Children 2023, 10, 31. https://doi.org/10.3390/children10010031
Cainelli E, Bisiacchi P. Neurodevelopmental Disorders: Past, Present, and Future. Children. 2023; 10(1):31. https://doi.org/10.3390/children10010031
Chicago/Turabian StyleCainelli, Elisa, and Patrizia Bisiacchi. 2023. "Neurodevelopmental Disorders: Past, Present, and Future" Children 10, no. 1: 31. https://doi.org/10.3390/children10010031
APA StyleCainelli, E., & Bisiacchi, P. (2023). Neurodevelopmental Disorders: Past, Present, and Future. Children, 10(1), 31. https://doi.org/10.3390/children10010031