Family Functioning, Maternal Depression, and Adolescent Cognitive Flexibility and Its Associations with Adolescent Depression: A Cross-Sectional Study
Abstract
:1. Introduction
Aim of This Study
2. Materials and Methods
2.1. Participants
2.2. Procedure
2.3. Measures
2.3.1. Family Functioning
2.3.2. Adolescents’ DepressionS
2.3.3. Maternal Depression
2.3.4. General Intellectual Function
2.3.5. Adolescents’ Cognitive Flexibility
2.4. Statistical Analysis
3. Results
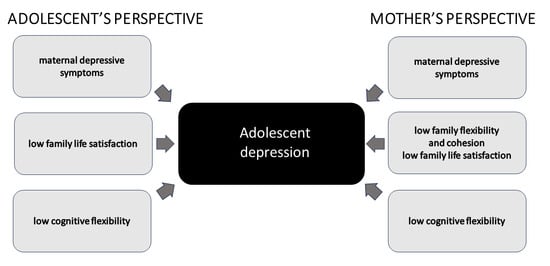
Factors Associated with Depression in Adolescents
4. Discussion
Limitations of This Study and Future Research
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Mullen, S. Major Depressive Disorder in Children and Adolescents. Ment. Health Clin. 2018, 8, 275. [Google Scholar] [CrossRef]
- Guerrera, C.S.; Platania, G.A.; Boccaccio, F.M.; Sarti, P.; Varrasi, S.; Colliva, C.; Grasso, M.; De Vivo, S.; Cavallaro, D.; Tascedda, F.; et al. The Dynamic Interaction between Symptoms and Pharmacological Treatment in Patients with Major Depressive Disorder: The Role of Network Intervention Analysis. BMC Psychiatry 2023, 23, 885. [Google Scholar] [CrossRef]
- Hawes, M.T.; Szenczy, A.K.; Klein, D.N.; Hajcak, G.; Nelson, B.D. Increases in Depression and Anxiety Symptoms in Adolescents and Young Adults during the COVID-19 Pandemic. Psychol. Med. 2022, 52, 3222–3230. [Google Scholar] [CrossRef]
- Shorey, S.; Ng, E.D.; Wong, C.H.J. Global Prevalence of Depression and Elevated Depressive Symptoms among Adolescents: A Systematic Review and Meta-Analysis. Br. J. Clin. Psychol. 2022, 61, 287–305. [Google Scholar] [CrossRef]
- Courtney, D.; Watson, P.; Battaglia, M.; Mulsant, B.H.; Szatmari, P. COVID-19 Impacts on Child and Youth Anxiety and Depression: Challenges and Opportunities. Can. J. Psychiatry 2020, 65, 688–691. [Google Scholar] [CrossRef] [PubMed]
- Johnson, D.; Dupuis, G.; Piche, J.; Clayborne, Z.; Colman, I. Adult Mental Health Outcomes of Adolescent Depression: A Systematic Review. Depress. Anxiety 2018, 35, 700–716. [Google Scholar] [CrossRef]
- Garber, J.; Cole, D.A. Intergenerational Transmission of Depression: A Launch and Grow Model of Change across Adolescence. Dev. Psychopathol. 2010, 22, 819–830. [Google Scholar] [CrossRef] [PubMed]
- Malhotra, S.; Sahoo, S. Antecedents of Depression in Children and Adolescents. Ind. Psychiatry J. 2018, 27, 11. [Google Scholar] [CrossRef]
- Shore, L.; Toumbourou, J.W.; Lewis, A.J.; Kremer, P. Review: Longitudinal Trajectories of Child and Adolescent Depressive Symptoms and Their Predictors—A Systematic Review and Meta-Analysis. Child Adolesc. Ment. Health 2018, 23, 107–120. [Google Scholar] [CrossRef] [PubMed]
- Fiorilli, C.; Capitello, T.G.; Barni, D.; Buonomo, I.; Gentile, S. Predicting Adolescent Depression: The Interrelated Roles of Self-Esteem and Interpersonal Stressors. Front. Psychol. 2019, 10, 565. [Google Scholar] [CrossRef]
- Pedersen, G.A.; Lam, C.; Hoffmann, M.; Zajkowska, Z.; Walsh, A.; Kieling, C.; Mondelli, V.; Fisher, H.L.; Gautam, K.; Kohrt, B.A. Psychological and Contextual Risk Factors for First-Onset Depression among Adolescents and Young People around the Globe: A Systematic Review and Meta-Analysis. Early Interv. Psychiatry 2023, 17, 5–20. [Google Scholar] [CrossRef]
- Şırelı, Ö.; Aysev Soykan, A. Depresyonu Olan Ergenlerin Anne-Baba Kabul-Red Algıları ve Aile Işlevleri Açısından Incelenmesi. Anadolu Psikiyatr. Derg. 2016, 17, 403–410. [Google Scholar] [CrossRef]
- Guerrero-Muñoz, D.; Salazar, D.; Constain, V.; Perez, A.; Pineda-Cañar, C.A.; García-Perdomo, H.A. Association between Family Functionality and Depression: A Systematic Review and Meta-Analysis. Korean J. Fam. Med. 2021, 42, 172–180. [Google Scholar] [CrossRef] [PubMed]
- Huang, X.; Hu, N.; Yao, Z.; Peng, B. Family Functioning and Adolescent Depression: A Moderated Mediation Model of Self-Esteem and Peer Relationships. Front. Psychol. 2022, 13, 962147. [Google Scholar] [CrossRef] [PubMed]
- Stevens, E.S.; Funkhouser, C.J.; Auerbach, R.P.; Talati, A.; Gameroff, M.G.; Posner, J.E.; Weissman, M.M.; Shankman, S.A. Inhibition Predicts the Course of Depression and Anxiety Symptoms Among Adolescents: The Moderating Role of Familial Risk. J. Nerv. Ment. Dis. 2023, 211, 100–107. [Google Scholar] [CrossRef]
- Becvar, R.J.; Stroh-Becvar, D.; Reif, L.V. Systems Theory and Family Therapy, 4th ed.; Rowman & Littlefield: Lanham, MD, USA, 2023. [Google Scholar]
- Cox, M.J.; Paley, B. Families as systems. Annu. Rev. Psychol. 1997, 48, 243–267. [Google Scholar] [CrossRef] [PubMed]
- Haefner, J. An Application of Bowen Family Systems Theory. Issues Ment. Health Nurs. 2014, 35, 835–841. [Google Scholar] [CrossRef] [PubMed]
- Beavers, R.; Hampson, R.B. The Beavers Systems Model of Family Functioning. J. Fam. Ther. 2000, 22, 128–143. [Google Scholar] [CrossRef]
- Olson, D.H.; Waldvogel, L.; Schlieff, M. Circumplex Model of Marital and Family Systems: An Update. J. Fam. Theory Rev. 2019, 11, 199–211. [Google Scholar] [CrossRef]
- Reinherz, H.Z.; Paradis, A.D.; Giaconia, R.M.; Stashwick, C.K.; Fitzmaurice, G. Childhood and Adolescent Predictors of Major Depression in the Transition to Adulthood. Am. J. Psychiatry 2003, 160, 2141–2147. [Google Scholar] [CrossRef]
- Roley, M.E.; Kawakami, R.; Baker, J.; Hurtado, G.; Chin, A.; Hovey, J.D. Family Cohesion Moderates the Relationship between Acculturative Stress and Depression in Japanese Adolescent Temporary Residents. J. Immigr. Minor. Health 2014, 16, 1299–1302. [Google Scholar] [CrossRef] [PubMed]
- Jhang, F.H. Economically Disadvantaged Adolescents’ Self-Concept and Academic Achievement as Mediators between Family Cohesion and Mental Health in Taiwan. Int. J. Ment. Health Addict. 2017, 15, 407–422. [Google Scholar] [CrossRef]
- Láng, A. Family Structure, Family Functioning, and Well-Being in Adolescence: A Multidimensional Approach. Int. J. Humanit. Soc. Sci. 2018, 8, 24–31. [Google Scholar] [CrossRef]
- Zahra, S.T.; Saleem, S. Family Cohesion and Depression in Adolescents: A Mediating Role of Self-Confidence. J. Pak. Med. Assoc. 2021, 71, 677–680. [Google Scholar] [CrossRef] [PubMed]
- Díez-Goñi, N.; Rodríguez-Díez, M.C. Why Teaching Empathy Is Important for the Medical Degree. Rev. Clin. Esp. 2017, 217, 332–335. [Google Scholar] [CrossRef] [PubMed]
- Li, M.; Li, L.; Wu, F.; Cao, Y.; Zhang, H.; Li, X.; Zou, J.; Guo, Z.; Kong, L. Perceived Family Adaptability and Cohesion and Depressive Symptoms: A Comparison of Adolescents and Parents during COVID-19 Pandemic. J. Affect. Disord. 2021, 287, 255–260. [Google Scholar] [CrossRef] [PubMed]
- Collishaw, S.; Hammerton, G.; Mahedy, L.; Sellers, R.; Owen, M.J.; Craddock, N.; Thapar, A.K.; Harold, G.T.; Rice, F.; Thapar, A. Mental Health Resilience in the Adolescent Offspring of Parents with Depression: A Prospective Longitudinal Study. Lancet Psychiatry 2016, 3, 49–57. [Google Scholar] [CrossRef] [PubMed]
- Yeh, Z.T.; Huang, Y.H.; Liu, S.I. Maternal Depression and Adolescent Emotions: The Role of Family Functioning. J. Child Fam. Stud. 2016, 25, 2189–2200. [Google Scholar] [CrossRef]
- Weissman, M.M. Children of Depressed Parents—A Public Health Opportunity. JAMA Psychiatry 2016, 73, 197–198. [Google Scholar] [CrossRef]
- Ayano, G.; Betts, K.; Lin, A.; Tait, R.; Alati, R. Maternal and Paternal Mental Health Problems and the Risk of Offspring Depression in Late Adolescence: Findings from the Raine Study. J. Ment. Health 2021, 30, 349–357. [Google Scholar] [CrossRef]
- Griffith, J.M.; Young, J.F.; Hankin, B.L. Longitudinal Coupling of Depression in Parent-Adolescent Dyads: Within- and Between-Dyad Effects over Time. Clin. Psychol. Sci. J. Assoc. Psychol. Sci. 2021, 9, 1059. [Google Scholar] [CrossRef]
- McAdams, T.A.; Rijsdijk, F.V.; Neiderhiser, J.M.; Narusyte, J.; Shaw, D.S.; Natsuaki, M.N.; Spotts, E.L.; Ganiban, J.M.; Reiss, D.; Leve, L.D.; et al. The Relationship between Parental Depressive Symptoms and Offspring: Evidence from a Children-of-Twins Study and an Adoption Study. Psychol. Med. 2015, 45, 2583. [Google Scholar] [CrossRef] [PubMed]
- Coles, D.C.; Cage, J. Mothers and Their Children: An Exploration of the Relationship Between Maternal Mental Health and Child Well-Being. Matern. Child Health J. 2022, 26, 1015–1021. [Google Scholar] [CrossRef] [PubMed]
- Agnafors, S.; Sydsjö, G.; Svedin, C.G.; Bladh, M. Symptoms of Depression and Internalizing Problems in Early Adulthood–Associated Factors from Birth to Adolescence. Nord. J. Psychiatry 2023, 77, 799–810. [Google Scholar] [CrossRef] [PubMed]
- Daches, S.; Vine, V.; Layendecker, K.M.; George, C.J.; Kovacs, M. Family Functioning as Perceived by Parents and Young Offspring at High and Low Risk for Depression. J. Affect. Disord. 2018, 226, 355–360. [Google Scholar] [CrossRef] [PubMed]
- Elsayed, N.M.; Fields, K.M.; Olvera, R.L.; Williamson, D.E. The Role of Familial Risk, Parental Psychopathology, and Stress for First-Onset Depression during Adolescence. J. Affect. Disord. 2019, 253, 232–239. [Google Scholar] [CrossRef]
- Van Dijk, M.T.; Murphy, E.; Posner, J.E.; Talati, A.; Weissman, M.M. Association of Multigenerational Family History of Depression With Lifetime Depressive and Other Psychiatric Disorders in Children: Results from the Adolescent Brain Cognitive Development (ABCD) Study. JAMA Psychiatry 2021, 78, 1. [Google Scholar] [CrossRef] [PubMed]
- Mennen, F.E.; Negriff, S.; Schneiderman, J.U.; Trickett, P.K. Longitudinal Associations of Maternal Depression and Adolescents’ Depression and Behaviors: Moderation by Maltreatment and Sex. J. Fam. Psychol. 2018, 32, 240–250. [Google Scholar] [CrossRef]
- Xerxa, Y.; Rescorla, L.A.; van der Ende, J.; Hillegers, M.H.J.; Verhulst, F.C.; Tiemeier, H. From Parent to Child to Parent: Associations Between Parent and Offspring Psychopathology. Child Dev. 2021, 92, 291. [Google Scholar] [CrossRef]
- Chithiramohan, T.; Eslick, G.D. Association Between Maternal Postnatal Depression and Offspring Anxiety and Depression in Adolescence and Young Adulthood: A Meta-Analysis. J. Dev. Behav. Pediatr. 2023, 44, E231–E238. [Google Scholar] [CrossRef]
- Sanger, C.; Iles, J.E.; Andrew, C.S.; Ramchandani, P.G. Associations between Postnatal Maternal Depression and Psychological Outcomes in Adolescent Offspring: A Systematic Review. Arch. Womens Ment. Health 2015, 18, 147–162. [Google Scholar] [CrossRef] [PubMed]
- Kwong, A.S.F.; López-López, J.A.; Hammerton, G.; Manley, D.; Timpson, N.J.; Leckie, G.; Pearson, R.M. Genetic and Environmental Risk Factors Associated With Trajectories of Depression Symptoms From Adolescence to Young Adulthood. JAMA Netw. Open 2019, 2, e196587. [Google Scholar] [CrossRef] [PubMed]
- Pearson, R.M.; Evans, J.; Kounali, D.; Lewis, G.; Heron, J.; Ramchandani, P.G.; O’Connor, T.G.; Stein, A. Maternal Depression during Pregnancy and the Postnatal Period: Risks and Possible Mechanisms for Offspring Depression at 18 Years. JAMA Psychiatry 2013, 70, 1312. [Google Scholar] [CrossRef] [PubMed]
- Betts, K.S.; Williams, G.M.; Najman, J.M.; Alati, R. The Relationship between Maternal Depressive, Anxious, and Stress Symptoms during Pregnancy and Adult Offspring Behavioral and Emotional Problems. Depress. Anxiety 2015, 32, 82–90. [Google Scholar] [CrossRef] [PubMed]
- Waters, C.S.; Hay, D.F.; Simmonds, J.R.; van Goozen, S.H.M. Antenatal Depression and Children’s Developmental Outcomes: Potential Mechanisms and Treatment Options. Eur. Child Adolesc. Psychiatry 2014, 23, 957–971. [Google Scholar] [CrossRef] [PubMed]
- Tirumalaraju, V.; Suchting, R.; Evans, J.; Goetzl, L.; Refuerzo, J.; Neumann, A.; Anand, D.; Ravikumar, R.; Green, C.E.; Cowen, P.J.; et al. Risk of Depression in the Adolescent and Adult Offspring of Mothers With Perinatal Depression: A Systematic Review and Meta-Analysis. JAMA Netw. Open 2020, 3, E208783. [Google Scholar] [CrossRef] [PubMed]
- Chen, J.; Zhao, J.; Chen, X.; Zou, Z.; Zhao, N.; Chen, C.X. Paternal Perinatal Depression: A Concept Analysis. Nurs. Open 2023, 10, 4995–5007. [Google Scholar] [CrossRef]
- Lew, D.; Xian, H.; Loux, T.; Shacham, E.; Scharff, D. The Longitudinal Impact of Maternal Depression and Neighborhood Social Context on Adolescent Mental Health. Front. Pediatr. 2022, 10, 854418. [Google Scholar] [CrossRef]
- Mahedy, L.; Hammerton, G.; Teyhan, A.; Edwards, A.C.; Kendler, K.S.; Moore, S.C.; Hickman, M.; MacLeod, J.; Heron, J. Parental Alcohol Use and Risk of Behavioral and Emotional Problems in Offspring. PLoS ONE 2017, 12, e0178862. [Google Scholar] [CrossRef]
- Tullius, J.M.; De Kroon, M.L.A.; Almansa, J.; Reijneveld, S.A. Adolescents’ Mental Health Problems Increase after Parental Divorce, Not before, and Persist until Adulthood: A Longitudinal TRAILS Study. Eur. Child Adolesc. Psychiatry 2022, 31, 969. [Google Scholar] [CrossRef]
- McHugh, C.M.; Iorfino, F.; Crouse, J.J.; Tickell, A.; Nichles, A.; Zmicerevska, N.; Ho, N.; Lee, R.; Hermens, D.F.; Scott, E.; et al. Neurocognitive Functioning Predicts Suicidal Behaviour in Young People with Affective Disorders. J. Affect. Disord. 2021, 281, 289–296. [Google Scholar] [CrossRef]
- Vilgis, V.; Silk, T.J.; Vance, A. Executive Function and Attention in Children and Adolescents with Depressive Disorders: A Systematic Review. Eur. Child Adolesc. Psychiatry 2015, 24, 365–384. [Google Scholar] [CrossRef] [PubMed]
- Wagner, S.; Müller, C.; Helmreich, I.; Huss, M.; Tadić, A. A Meta-Analysis of Cognitive Functions in Children and Adolescents with Major Depressive Disorder. Eur. Child Adolesc. Psychiatry 2015, 24, 5–19. [Google Scholar] [CrossRef] [PubMed]
- Oliver, A.; Pile, V.; Elm, D.; Lau, J.Y.F. The Cognitive Neuropsychology of Depression in Adolescents. Curr. Behav. Neurosci. Rep. 2019, 6, 227–235. [Google Scholar] [CrossRef]
- Gillespie, M.L.; Rao, U. Relationships between Depression and Executive Functioning in Adolescents: The Moderating Role of Unpredictable Home Environment. J. Child Fam. Stud. 2022, 31, 2518–2534. [Google Scholar] [CrossRef] [PubMed]
- Urbańska-Grosz, J.; Walkiewicz, M.; Sitek, E.J. Is There Sufficient Evidence for the Association between Executive Dysfunction and Academic Performance in Adolescents with Major Depressive Disorder?: A Systematic Review. Eur. Child Adolesc. Psychiatry 2023, 1, 1–12. [Google Scholar] [CrossRef] [PubMed]
- de Lissnyder, E.; Koster, E.H.W.; Derakshan, N.; de Raedt, R. The Association between Depressive Symptoms and Executive Control Impairments in Response to Emotional and Non-Emotional Information. Cogn. Emot. 2010, 24, 264–280. [Google Scholar] [CrossRef]
- Roiser, J.P.; Elliott, R.; Sahakian, B.J. Cognitive Mechanisms of Treatment in Depression. Neuropsychopharmacology 2011, 37, 117–136. [Google Scholar] [CrossRef]
- Stange, J.P.; Connolly, S.L.; Burke, T.A.; Hamilton, J.L.; Hamlat, E.J.; Abramson, L.Y.; Alloy, L.B. Inflexible Cognition Predicts First Onset of Major Depressive Episodes in Adolescence. Depress. Anxiety 2016, 33, 1005. [Google Scholar] [CrossRef]
- Stange, J.P.; Alloy, L.B.; Fresco, D.M. Inflexibility as a Vulnerability to Depression: A Systematic Qualitative Review. Clin. Psychol. Sci. Pract. 2017, 24, 245–276. [Google Scholar] [CrossRef]
- Davidovich, S.; Collishaw, S.; Thapar, A.K.; Harold, G.; Thapar, A.; Rice, F. Do Better Executive Functions Buffer the Effect of Current Parental Depression on Adolescent Depressive Symptoms? J. Affect. Disord. 2016, 199, 54. [Google Scholar] [CrossRef] [PubMed]
- Craun, E.; Lachance, K.; Williams, C.; Wong, M.M. Parent Depressive Symptoms and Offspring Executive Functioning. J. Clin. Exp. Neuropsychol. 2019, 41, 147–157. [Google Scholar] [CrossRef] [PubMed]
- Roman, G.D.; Ensor, R.; Hughes, C. Does Executive Function Mediate the Path from Mothers’ Depressive Symptoms to Young Children’s Problem Behaviors? J. Exp. Child Psychol. 2016, 142, 158–170. [Google Scholar] [CrossRef] [PubMed]
- Hughes, C.; Roman, G.; Hart, M.J.; Ensor, R. Does Maternal Depression Predict Young Children’s Executive Function?—A 4-Year Longitudinal Study. J. Child Psychol. Psychiatry 2013, 54, 169–177. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization. International Classification of Diseases, 10th ed.; World Health Organization: Geneva, Switzerland, 2010. [Google Scholar]
- Margasiński, A. The Polish Adaptation of FACES IV-SOR. Polish J. Appl. Psychol. 2015, 13, 43–66. [Google Scholar] [CrossRef]
- Zawadzki, B.; Popiel, A.; Praglowska, E. Psychometric Properties of the Polish Version of the Aaron T. Beck’s Depression Inventory BDI-II (Charakterystyka Psychometryczna Polskiej Adaptacji Kwestionariusza Depresji BDI-II Aarona T. Becka). Psychologia-Etologia-Genetyka 2009, 19, 71–95. [Google Scholar]
- Matczak, A.; Jaworowska, A.; Martowska, K. Test Rozumienia Słów: Wersja Standard TRS-S Wersja Dla Zaawansowanych TRS-Z; Pracownia Testów Psychologicznych Polskiego Towarzystwa Psychologicznego: Warsaw, Poland, 2012; ISBN 9788360733998. [Google Scholar]
- Burgess, P.W.; Alderman, N.; Evans, J.; Emslie, H.; Wilson, B.A. The Ecological Validity of Tests of Executive Function. J. Int. Neuropsychol. Soc. 1998, 4, 547–558. [Google Scholar] [CrossRef]
- Tchanturia, K.; Harrison, A.; Davies, H.; Roberts, M.; Oldershaw, A.; Nakazato, M.; Stahl, D.; Morris, R.; Schmidt, U.; Treasure, J. Cognitive Flexibility and Clinical Severity in Eating Disorders. PLoS ONE 2011, 6, e20462. [Google Scholar] [CrossRef]
- Olson, D.H.; Sprenkle, D.H.; Russell, C.S. Circumplex Model of Marital and Family System: I. Cohesion and Adaptability Dimensions, Family Types, and Clinical Applications. Fam. Process 1979, 18, 3–28. [Google Scholar] [CrossRef]
- Olson, D. FACES IV and the Circumplex Model: Validation Study. J. Marital Fam. Ther. 2011, 37, 64–80. [Google Scholar] [CrossRef]
- Kovacs, M. Children’s Depression Inventory (CDI and CDI 2). In The Encyclopedia of Clinical Psychology; Cautin, R.L., Lilienfeld, S.O., Eds.; Wiley: Hoboken, NJ, USA, 2015. [Google Scholar] [CrossRef]
- Kovacs, M.; Wrocławska-Warchala, E.; Wujcik, R. Zestaw Kwestionariuszy Do Diagnozy Depresji u Dzieci i Młodzieży CDI 2TM Maria Kovacs i Zespół MHS: Podręcznik; Pracownia Testów Psychologicznych Polskiego Towarzystwa Psychologicznego: Warszawa, Poland, 2017; ISBN 9788363545406. [Google Scholar]
- Steer, R.A.; Ball, R.; Ranieri, W.F.; Beck, A.T. Dimensions of the Beck Depression Inventory-II in Clinically Depressed Outpatients. J. Clin. Psychol. 1999, 55, 117–128. [Google Scholar] [CrossRef]
- Kluczniok, D.; Boedeker, K.; Fuchs, A.; Hindi Attar, C.; Fydrich, T.; Fuehrer, D.; Dittrich, K.; Reck, C.; Winter, S.; Heinz, A.; et al. Emotional Availability in Mother-Child Interaction: The Effects of Maternal Depression in Remission and Additional History of Childhood Abuse. Depress. Anxiety 2016, 33, 648–657. [Google Scholar] [CrossRef] [PubMed]
- Trussell, T.M.; Ward, W.L.; Conners Edge, N.A. The Impact of Maternal Depression on Children: A Call for Maternal Depression Screening. Clin. Pediatr. 2018, 57, 1137–1147. [Google Scholar] [CrossRef] [PubMed]
- Goodman, S.H.; Simon, H.F.M.; Shamblaw, A.L.; Kim, C.Y. Parenting as a Mediator of Associations between Depression in Mothers and Children’s Functioning: A Systematic Review and Meta-Analysis. Clin. Child Fam. Psychol. Rev. 2020, 23, 427–460. [Google Scholar] [CrossRef] [PubMed]
- Ohannessian, C.M.C.; Laird, R.; De Los Reyes, A. Discrepancies in Adolescents’ and Mothers’ Perceptions of the Family and Mothers’ Psychological Symptomatology. J. Youth Adolesc. 2016, 45, 2011–2021. [Google Scholar] [CrossRef] [PubMed]
- Laird, R.D.; De Los Reyes, A. Testing Informant Discrepancies as Predictors of Early Adolescent Psychopathology: Why Difference Scores Cannot Tell You What You Want to Know and How Polynomial Regression May. J. Abnorm. Child Psychol. 2013, 41, 1–14. [Google Scholar] [CrossRef] [PubMed]
- Steinberg, L.; Morris, A.S. Adolescent Development. Annu. Rev. Psychol. 2003, 52, 83–110. [Google Scholar] [CrossRef] [PubMed]
- Pérez, J.C.; Coo, S.; Irarrázaval, M. Is Maternal Depression Related to Mother and Adolescent Reports of Family Functioning?☆. J. Adolesc. 2018, 63, 129–141. [Google Scholar] [CrossRef]
- Nam, B.; Kim, J.Y.; DeVylder, J.E.; Song, A. Family Functioning, Resilience, and Depression among North Korean Refugees. Psychiatry Res. 2016, 245, 451–457. [Google Scholar] [CrossRef]
- Gä, K.; Id, A.; Bøe, T.; Breivik, K.; Greca, A.M.L.; Sivertsen, B.; Hysing, M. Life Events and Adolescent Depressive Symptoms: Protective Factors Associated with Resilience. PLoS ONE 2020, 15, e0234109. [Google Scholar] [CrossRef]
- Olson, D.H.; Gorall, D. Circumplex Model of Marital and Family Systems. In Normal Family Processes; Walsh, F., Ed.; The Guilford Press: New York, NY, USA, 2003; pp. 514–517. [Google Scholar]
- Zhang, S.; Baams, L.; van de Bongardt, D.; Dubas, J.S. Intra- and Inter-Individual Differences in Adolescent Depressive Mood: The Role of Relationships with Parents and Friends. J. Abnorm. Child Psychol. 2018, 46, 811–824. [Google Scholar] [CrossRef] [PubMed]
- Asarnow, J.R.; Tompson, M.C.; Klomhaus, A.M.; Babeva, K.; Langer, D.A.; Sugar, C.A. Randomized Controlled Trial of Family-Focused Treatment for Child Depression Compared to Individual Psychotherapy: One-Year Outcomes. J. Child Psychol. Psychiatry 2020, 61, 662–671. [Google Scholar] [CrossRef] [PubMed]
- Donald, M.; Dower, J.; Correa-Velez, I.; Jones, M. Risk and Protective Factors for Medically Serious Suicide Attempts: A Comparison of Hospital-Based with Population-Based Samples of Young Adults. Aust. N. Z. J. Psychiatry 2006, 40, 87–96. [Google Scholar] [CrossRef] [PubMed]
- D’Onofrio, B.; Emery, R. Parental Divorce or Separation and Children’s Mental Health. World Psychiatry 2019, 18, 100–101. [Google Scholar] [CrossRef] [PubMed]
- Vidal, S.I.; Vandeleur, C.; Rothen, S.; Gholam-Rezaee, M.; Castelao, E.; Halfon, O.; Aubry, J.M.; Ferrero, F.; Preisig, M. Risk of Mental Disorders in Children of Parents with Alcohol or Heroin Dependence: A Controlled High-Risk Study. Eur. Addict. Res. 2012, 18, 253–264. [Google Scholar] [CrossRef] [PubMed]
- Bountress, K.; Chassin, L. Risk for Behavior Problems in Children of Parents with Substance Use Disorders. Am. J. Orthopsychiatry 2015, 85, 275. [Google Scholar] [CrossRef] [PubMed]
- Jafry, Z.; Chui, K.; Stopka, T.J.; Corlin, L. Residence with a Person Who Used Substances and Childhood Anxiety and Depression: A Cross-Sectional Analysis of the 2019 National Health Interview Survey. Children 2022, 9, 1296. [Google Scholar] [CrossRef] [PubMed]
- Harter, S.L. Psychosocial Adjustment of Adult Children of Alcoholics: A Review of the Recent Empirical Literature. Clin. Psychol. Rev. 2000, 20, 311–337. [Google Scholar] [CrossRef]
- Rolf, J.E.; Johnson, J.L.; Israel, E.; Baldwin, J.; Chandra, A. Depressive Affect in School-Aged Children of Alcoholics. Br. J. Addict. 1988, 83, 841–848. [Google Scholar] [CrossRef]
- Jones, B.; Durtschi, J.; Keilholtz, B. Maternal Engagement, Relational Closeness, and Adolescent Internalizing Symptoms: The Association of Engaged Mothering with Adolescent Depression and Anxiety. J. Marital Fam. Ther. 2023, 49, 861–878. [Google Scholar] [CrossRef]
- Shi, J.; Tao, Y.; Yan, C.; Zhao, X.; Wu, X.; Zhang, T.; Zhong, C.; Sun, J.; Hu, M. A Study on the Correlation between Family Dynamic Factors and Depression in Adolescents. Front. Psychiatry 2023, 13, 1025168. [Google Scholar] [CrossRef] [PubMed]
- Korelitz, K.E.; Garber, J. Congruence of Parents’ and Children’s Perceptions of Parenting: A Meta-Analysis. J. Youth Adolesc. 2016, 45, 1973. [Google Scholar] [CrossRef] [PubMed]
- Nelemans, S.A.; Branje, S.J.T.; Hale, W.W.; Goossens, L.; Koot, H.M.; Oldehinkel, A.J.; Meeus, W.H.J. Discrepancies Between Perceptions of the Parent–Adolescent Relationship and Early Adolescent Depressive Symptoms: An Illustration of Polynomial Regression Analysis. J. Youth Adolesc. 2016, 45, 2049–2063. [Google Scholar] [CrossRef] [PubMed]
- Edwards, J.R. Alternatives to Difference Scores: Polynomial Regression Analysis and Response Surface Methodology. In Measuring and Analyzing Behavior in Organizations: Advances in Measurement and Data Analysis; Drasgow, F., Schmitt, N., Eds.; Jossey-Bass: Hoboken, NJ, USA, 2002; pp. 350–400. [Google Scholar]
- De Los Reyes, A.; Ohannessian, C.M.C. Introduction to the Special Issue: Discrepancies in Adolescent–Parent Perceptions of the Family and Adolescent Adjustment. J. Youth Adolesc. 2016, 45, 1957–1972. [Google Scholar] [CrossRef] [PubMed]
- Lerner, R.M.; Konowitz, L.S. Commentary: Theoretical and Methodological Dimensions of Convergence and Divergence of Adolescent and Parent Reports about Youth Development and Family Structure and Function—A Relational Developmental Systems Perspective. J. Youth Adolesc. 2016, 45, 2178–2184. [Google Scholar] [CrossRef] [PubMed]
- Rote, W.M.; Smetana, J.G. Patterns and Predictors of Mother–Adolescent Discrepancies across Family Constructs. J. Youth Adolesc. 2016, 45, 2064–2079. [Google Scholar] [CrossRef] [PubMed]
- Lippold, M.A.; Greenberg, M.T.; Collins, L.M. Parental Knowledge and Youth Risky Behavior: A Person Oriented Approach. J. Youth Adolesc. 2013, 42, 1732. [Google Scholar] [CrossRef] [PubMed]
- Lippold, M.A.; Greenberg, M.T.; Feinberg, M.E. A Dyadic Approach to Understanding the Relationship of Maternal Knowledge of Youths’ Activities to Youths’ Problem Behavior Among Rural Adolescents. J. Youth Adolesc. 2011, 40, 1178–1191. [Google Scholar] [CrossRef]
- Lippold, M.A.; Greenberg, M.T.; Collins, L.M. Youths’ Substance Use and Changes in Parental Knowledge-Related Behaviors During Middle School: A Person-Oriented Approach. J. Youth Adolesc. 2014, 43, 729. [Google Scholar] [CrossRef]
- Yaban, E.H.; Sayil, M.; Tepe, Y.K. Are Discrepancies in Perceptions of Psychological Control Related to Maladjustment A Study of Adolescents and Their Parents in Turkey. Int. J. Behav. Dev. 2014, 38, 550–562. [Google Scholar] [CrossRef]
- Diamond, A. Executive Functions. Annu. Rev. Psychol. 2013, 64, 135–168. [Google Scholar] [CrossRef] [PubMed]
- Harmer, C.J.; O’Sullivan, U.; Favaron, E.; Massey-Chase, R.; Ayres, R.; Reinecke, A.; Goodwin, G.M.; Cowen, P.J. Effect of Acute Antidepressant Administration on Negative Affective Bias in Depressed Patients. Am. J. Psychiatry 2009, 166, 1178–1184. [Google Scholar] [CrossRef] [PubMed]
- Schwartz, O.S.; Simmons, J.G.; Whittle, S.; Byrne, M.L.; Yap, M.B.H.; Sheeber, L.B.; Allen, N.B. Affective Parenting Behaviors, Adolescent Depression, and Brain Development: A Review of Findings From the Orygen Adolescent Development Study. Child Dev. Perspect. 2017, 11, 90–96. [Google Scholar] [CrossRef]
- Burke, T.; Wynne, B.; O’Brien, C.; Elamin, M.; Bede, P.; Hardiman, O.; Pender, N. Retrospective Investigations of Practice Effects on Repeated Neuropsychological Measures of Executive Functioning. Irish J. Psychol. 2014, 35, 178–187. [Google Scholar] [CrossRef]
- Cox, M.J.; Paley, B. Understanding Families as Systems. Curr. Dir. Psychol. Sci. 2003, 12, 193–196. [Google Scholar] [CrossRef]
- Satir, V.; Ochmańska, Ł.; Trzebiatowska, M. Rodzina: Tu Powstaje Człowiek; Gdańskie Wydawnictwo Psychologiczne: Gdańsk, Poland, 2002. [Google Scholar]
- Cicchetti, D.; Rogosch, F.A. A Developmental Psychopathology Perspective on Adolescence. J. Consult. Clin. Psychol. 2002, 70, 6–20. [Google Scholar] [CrossRef] [PubMed]
- Goldenberg, H.; Goldenberg, I.; Stanton, M. Family Therapy: An Overview, 9th ed.; CENGAGE Learning Custom Publishing: Mason, OH, USA, 2016. [Google Scholar]
- Eckshtain, D.; Horn, R.; Weisz, J.R. Family-Based Interventions for Youth Depression: Meta-Analysis of Randomized Clinical Trials. Child Psychiatry Hum. Dev. 2023, 54, 1737–1748. [Google Scholar] [CrossRef]
- Dippel, N.; Szota, K.; Cuijpers, P.; Christiansen, H.; Brakemeier, E.L. Family Involvement in Psychotherapy for Depression in Children and Adolescents: Systematic Review and Meta-Analysis. Psychol. Psychother. Theory Res. Pract. 2022, 95, 656–679. [Google Scholar] [CrossRef]
- Tsvieli, N.; Nir-Gottlieb, O.; Lifshitz, C.; Diamond, G.S.; Kobak, R.; Diamond, G.M. Therapist Interventions Associated with Productive Emotional Processing in the Context of Attachment-Based Family Therapy for Depressed and Suicidal Adolescents. Fam. Process 2020, 59, 428–444. [Google Scholar] [CrossRef]
- Stern, R.S.; King, A.A.; Diamond, G. Repairing Attachment in Families with Depressed Adolescents: A Task Analysis. J. Clin. Psychol. 2023, 79, 201–209. [Google Scholar] [CrossRef]
- Tichovolsky, M.H.; Griffith, S.F.; Rolon-Arroyo, B.; Arnold, D.H.; Harvey, E.A. A Longitudinal Study of Fathers’ and Young Children’s Depressive Symptoms. J. Clin. Child Adolesc. Psychol. 2018, 47, S190–S204. [Google Scholar] [CrossRef] [PubMed]
- Vakrat, A.; Apter-Levy, Y.; Feldman, R. Sensitive Fathering Buffers the Effects of Chronic Maternal Depression on Child Psychopathology. Child Psychiatry Hum. Dev. 2018, 49, 779–785. [Google Scholar] [CrossRef] [PubMed]
- Luthar, S.S.; Cicchetti, D.; Becker, B. The Construct of Resilience: A Critical Evaluation and Guidelines for Future Work. Child Dev. 2000, 71, 543. [Google Scholar] [CrossRef] [PubMed]
- Psychogiou, L.; Parry, E. Why Do Depressed Individuals Have Difficulties in Their Parenting Role? Psychol. Med. 2014, 44, 1345–1347. [Google Scholar] [CrossRef] [PubMed]
- Barrett, J.; Fleming, A.S. Annual Research Review: All Mothers Are Not Created Equal: Neural and Psychobiological Perspectives on Mothering and the Importance of Individual Differences. J. Child Psychol. Psychiatry 2011, 52, 368–397. [Google Scholar] [CrossRef] [PubMed]
- Bögels, S.M.; Lehtonen, A.; Restifo, K. Mindful Parenting in Mental Health Care. Mindfulness 2010, 1, 107–120. [Google Scholar] [CrossRef] [PubMed]
- Bartkowski, J.P.; Xu, X.; Bartkowski, S. Mixed Blessing: The Beneficial and Detrimental Effects of Religion on Child Development among Third-Graders. Religions 2019, 10, 37. [Google Scholar] [CrossRef]
| Depressed Adolescents (n = 63) | Healthy Controls (n = 46) | |||||
|---|---|---|---|---|---|---|
| χ² | p | |||||
| sex | 35 girls (56%) 28 boys (44%) | 22 girls (48%) 24 boys (52%) | −0.7907 | 0.4249 | ||
| Me ± IQR | min.–max. | Me ± IQR | min.–max. | intergroup difference | p | |
| Age | 17 (4) | 15–19 | 17 (4) | 15–19 | z = −1.2844 | 0.1989 |
| Overall intellectual functioning TRS-Z (1–30) | 8 (6) | 2–19 | 9 (5) | 3–23 | z = −0.1601 | 0.8728 |
| Mood | ||||||
| CDI-2 self-rating (T score: 0–79) | 74 (8) | 54–79 | 47 (16) | 21–64 | z = −8.7064 | 0.0001 |
| CDI-2 assessed by mothers (T score: 0–79) | 75 (30) | 49–79 | 45 (37) | 23–60 | z = −8.64 | 0.0001 |
| ± SD | min.–max. | ± SD | min.–max. | intergroup difference | p | |
| BDI-II (raw score: 0–63) | 37 (8) | 20–53 | 8 (9) | 0–23 | t = 8.8702 | 0.0001 |
| Cognitive Flexibility | ||||||
| Me ± IQR | Me ± IQR | |||||
| The Brixton Spatial Anticipation Test (scaled score: 0–10) | 4.57 (1.94) | 1–10 | 6.98 (1.44) | 4–10 | z = 6.0568 | 0.001 |
| Mother | Depressed Adolescents (n = 63) | Healthy Controls (n = 46) | ||||
|---|---|---|---|---|---|---|
| ± SD/Me ± IQR | min.–max. | ± SD/Me ± IQR | min.–max. | Intergroup Difference | p | |
| Age | Me ± IQR 44.98 (4.71) | 35–55 | Me ± IQR 43.54 (4.19) | 36–54 | t = 1.65 | 0.10 |
| BDI-II | ± SD 15 (16) | 0–43 | ± SD 8 (5) | 3–25 | z = 3.2475 | 0.0011 |
| Family Functioning | Depressed Adolescents (n = 63) | Healthy Controls (n = 46) | ||||
|---|---|---|---|---|---|---|
| A—Adolescent M—Mother | Me ± IQR | min.–max. | Me ± IQR | min.–max. | Intergroup Difference | p |
| General Family Functioning A (0–3) | 0.56 ± 0.41 | 0.21–1.77 | 0.78 ± 0.42 | 0.40–2.00 | z = −3.9673 | 0.0001 |
| General Family Functioning M (0–3) | 0.72 ± 0.66 | 0.15–1.89 | 0.91 ± 0.30 | 0.48–1.75 | z = −2.2090 | 0.0271 |
| Cohesion A (0–3) | 0.53 ± 0.47 | 0.13–1.75 | 0.77 ± 0.46 | 0.24–2.50 | z = −3.3088 | 0.0009 |
| Cohesion M (0–3) | 0.67 ± 0.70 | 0.13–3.00 | 0.77 ± 0.28 | 0.40–1.80 | z = −0.8196 | 0.4124 |
| Flexibility A (0–3) | 0.63 ± 0.40 | 0.25–3.00 | 0.87 ± 0.54 | 0.46–2.40 | z = −3.4132 | 0.0006 |
| Flexiblity M (0–3) | 0.77 ± 0.59 | 0.18–2.00 | 1.00 ± 0.40 | 0.57–2.33 | z = −3.24118 | 0.0011 |
| Communication raw score A (0–50) | 28 ± 12 | 12–49 | 37.50 ± 11 | 23–50 | z = −5.1398 | 0.0001 |
| Communication raw score M (0–50) | 35 ± 10 | 4–50 | 39 ± 7 | 29–48 | z = −4.3432 | 0.0001 |
| ± SD | ± SD | |||||
| Satisfaction raw score A (0–50) | 27.27 ± 6.81 | 13–48 | 38.39 ± 6.60 | 24–50 | t = −6.8303 | 0.0001 |
| Satisfaction raw score M (0–50) | 32.40 ± 7.23 | 13–48 | 39.17 ± 4.94 | 30–47 | t = −5.0082 | 0.0001 |
| Model | Factors Associated | B | SE | Wald | df | p | Exp(B) [95% CI] |
|---|---|---|---|---|---|---|---|
| 1 | Family life satisfaction (FACES IV) | −0.05 | 0.01 | 31.84 | 1 | <0.001 | 0.95 [0.93–0.97] |
| Intercept | 2.55 | 0.47 | 29.86 | 1 | <0.001 | 12.83 | |
| Model χ2(8) = 9.29, p = 0.318; Nagelkerke R2 = 0.521 | |||||||
| 2 | Family life satisfaction (FACES IV) | −0.06 | 0.01 | 20.79 | 1 | <0.001 | 0.94 [0.91–0.97] |
| Cognitive flexibility (The Brixton Spatial Anticipation Test) | −1.15 | 0.29 | 15.49 | 1 | <0.001 | 0.32 [0.18–0.56] | |
| Intercept | 9.90 | 2.22 | 19.82 | 1 | <0.001 | 19,862.73 | |
| Model χ2(8) = 5.42; p = 0.712; Nagelkerke R2 = 0.739 | |||||||
| 3 | Family life satisfaction (FACES IV) | −0.08 | 0.02 | 17.76 | 1 | <0.001 | 0.93 [0.89–0.96] |
| BDI-II: Mother’s depressive symptoms/Baseline: low level | 8.99 | 2 | 0.011 | ||||
| average level | −0.11 | 0.84 | 0.02 | 1 | 0.896 | 0.90 [0.17–4.69] | |
| high level | 2.87 | 1.09 | 6.91 | 1 | 0.009 | 17.59 [2.07–149.20] | |
| Cognitive flexibility (The Brixton Spatial Anticipation Test) | −1.17 | 0.33 | 12.66 | 1 | <0.001 | 0.31 [0.16–0.59] | |
| Intercept | 9.84 | 2.51 | 15.33 | 1 | <0.001 | 18,850.75 | |
| Model χ2(8) = 3.29; p = 0.915; Nagelkerke R2 = 0.804 | |||||||
| Model | Factors Associated | B | SE | Wald | df | p | Exp(B) [95% CI] |
|---|---|---|---|---|---|---|---|
| 1 | Cognitive flexibility (The Brixton Spatial Anticipation Test) | −0.82 | 0.17 | 24.21 | 1 | <0.001 | 0.44 [0.32–0.61] |
| Intercept | 5.10 | 1.03 | 24.55 | 1 | <0.001 | 163.99 | |
| 2 | Family life satisfaction (FACES IV) | −0.03 | 0.01 | 9.27 | 1 | 0.002 | 0.97 [0.95–0.99] |
| Cognitive flexibility (The Brixton Spatial Anticipation Test) | −0.76 | 0.18 | 17.87 | 1 | <0.001 | 0.47 [0.33–0.67] | |
| Intercept | 6.20 | 1.24 | 25.03 | 1 | <0.001 | 491.56 | |
| 3 | Mother’s depression/Baseline: low level | 8.66 | 2 | 0.013 | |||
| average level BDI-II: | −0.10 | 0.62 | 0.02 | 1 | 0.877 | 0.91 [0.27–3.04] | |
| high level | 1.95 | 0.73 | 7.15 | 1 | 0.007 | 7.03 [1.68–29.37] | |
| Family life satisfaction (FACES IV) | −0.03 | 0.01 | 9.63 | 1 | 0.002 | 0.97 [0.95–0.99] | |
| Cognitive flexibility (The Brixton Spatial Anticipation Test) | −0.67 | 0.18 | 14.01 | 1 | <0.001 | 0.51 [0.36–0.73] | |
| Intercept | 5.35 | 1.28 | 17.57 | 1 | <0.001 | 210.73 | |
| 4 | Mother’s depression/Baseline: low level | 7.04 | 2 | 0.030 | |||
| average level BDI-II: | 0.05 | 0.64 | 0.01 | 1 | 0.943 | 1.05 [0.30–3.68] | |
| high level | 1.86 | 0.75 | 6.10 | 1 | 0.013 | 6.45 [1.47–28.30] | |
| Family cohesion (FACES IV) | 2.11 | 0.96 | 4.82 | 1 | 0.028 | 8.21 [1.25–53.72] | |
| Family life satisfaction (FACES IV) | −0.05 | 0.01 | 12.21 | 1 | <0.001 | 0.95 [0.93–0.98] | |
| Cognitive flexibility (The Brixton Spatial Anticipation Test) | −0.65 | 0.18 | 12.34 | 1 | <0.001 | 0.52 [0.36–0.75] | |
| Intercept | 4.22 | 1.35 | 9.80 | 1 | 0.002 | 67.71 | |
| 5 | Mother’s depression/Baseline: low level | 6.01 | 2 | 0.049 | |||
| average level BDI-II: | 0.04 | 0.67 | 0.00 | 1 | 0.952 | 1.04 [0.28–3.89] | |
| high level | 1.84 | 0.80 | 5.31 | 1 | 0.021 | 6.31 [1.32–30.19] | |
| Family flexibility (FACES IV) | −2.27 | 1.07 | 4.47 | 1 | 0.034 | 0.10 [0.01–0.85] | |
| Family cohesion (FACES IV) | 3.17 | 1.17 | 7.31 | 1 | 0.007 | 23.91 [2.39–238.77] | |
| Family life satisfaction (FACES IV) | −0.05 | 0.01 | 11.92 | 1 | 0.001 | 0.95 [0.92–0.98] | |
| Cognitive flexibility (The Brixton Spatial Anticipation Test) | −0.57 | 0.19 | 9.06 | 1 | 0.003 | 0.56 [0.39–0.82] | |
| Intercept | 5.14 | 1.47 | 12.17 | 1 | <0.001 | 171.23 | |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Urbańska-Grosz, J.; Sitek, E.J.; Pakalska, A.; Pietraszczyk-Kędziora, B.; Skwarska, K.; Walkiewicz, M. Family Functioning, Maternal Depression, and Adolescent Cognitive Flexibility and Its Associations with Adolescent Depression: A Cross-Sectional Study. Children 2024, 11, 131. https://doi.org/10.3390/children11010131
Urbańska-Grosz J, Sitek EJ, Pakalska A, Pietraszczyk-Kędziora B, Skwarska K, Walkiewicz M. Family Functioning, Maternal Depression, and Adolescent Cognitive Flexibility and Its Associations with Adolescent Depression: A Cross-Sectional Study. Children. 2024; 11(1):131. https://doi.org/10.3390/children11010131
Chicago/Turabian StyleUrbańska-Grosz, Justyna, Emilia J. Sitek, Anna Pakalska, Bożena Pietraszczyk-Kędziora, Kalina Skwarska, and Maciej Walkiewicz. 2024. "Family Functioning, Maternal Depression, and Adolescent Cognitive Flexibility and Its Associations with Adolescent Depression: A Cross-Sectional Study" Children 11, no. 1: 131. https://doi.org/10.3390/children11010131
APA StyleUrbańska-Grosz, J., Sitek, E. J., Pakalska, A., Pietraszczyk-Kędziora, B., Skwarska, K., & Walkiewicz, M. (2024). Family Functioning, Maternal Depression, and Adolescent Cognitive Flexibility and Its Associations with Adolescent Depression: A Cross-Sectional Study. Children, 11(1), 131. https://doi.org/10.3390/children11010131