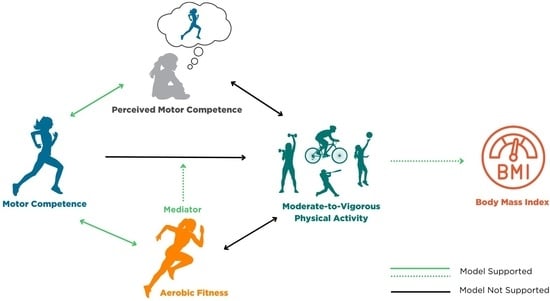
Associations among Motor Competence, Physical Activity, Perceived Motor Competence, and Aerobic Fitness in 10–15-Year-Old Youth †
Abstract
:1. Introduction
2. Materials and Methods
2.1. Study Participants
2.2. Study Design
2.2.1. Bruininks–Oseretsky Test Analysis Test for Motor Proficiency
2.2.2. Perceived Motor Competence
2.2.3. Physical Activity Assessment
2.2.4. Health-Related Fitness Assessment
2.2.5. Data Treatment and Statistical Analyses
3. Results
Participant Characteristics
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Chaput, J.P.; Willumsen, J.; Bull, F.; Chou, R.; Ekelund, U.; Firth, J.; Jago, R.; Ortega, F.B.; Katzmarzyk, P.T. 2020 WHO guidelines on physical activity and sedentary behaviour for children and adolescents aged 5–17 years: Summary of the evidence. Int. J. Behav. Nutr. Phys. Act. 2020, 17, 141. [Google Scholar] [CrossRef] [PubMed]
- Piercy, K.L.; Troiano, R.P.; Ballard, R.M.; Carlson, S.A.; Fulton, J.E.; Galuska, D.A.; George, S.M.; Olson, R.D. The Physical Activity Guidelines for Americans. JAMA 2018, 320, 2020–2028. [Google Scholar] [CrossRef]
- Malina, R.M. Tracking of physical activity and physical fitness across the lifespan. Res. Q. Exerc. Sport 1996, 67, S48–S57. [Google Scholar] [CrossRef]
- Telama, R.; Yang, X.; Leskinen, E.; Kankaanpaa, A.; Hirvensalo, M.; Tammelin, T.; Viikari, J.S.; Raitakari, O.T. Tracking of physical activity from early childhood through youth into adulthood. Med. Sci. Sports Exerc. 2014, 46, 955–962. [Google Scholar] [CrossRef]
- Marques, A.; Henriques-Neto, D.; Peralta, M.; Martins, J.; Demetriou, Y.; Schonbach, D.M.I.; Matos, M.G. Prevalence of Physical Activity among Adolescents from 105 Low, Middle, and High-income Countries. Int. J. Environ. Res. Public. Health 2020, 17, 3145. [Google Scholar] [CrossRef] [PubMed]
- Neville, R.D.; Lakes, K.D.; Hopkins, W.G.; Tarantino, G.; Draper, C.E.; Beck, R.; Madigan, S. Global Changes in Child and Adolescent Physical Activity during the COVID-19 Pandemic: A Systematic Review and Meta-analysis. JAMA Pediatr. 2022, 176, 886–894. [Google Scholar] [CrossRef]
- Troiano, R.P.; Berrigan, D.; Dodd, K.W.; Masse, L.C.; Tilert, T.; McDowell, M. Physical activity in the United States measured by accelerometer. Med. Sci. Sports Exerc. 2008, 40, 181–188. [Google Scholar] [CrossRef] [PubMed]
- Strong, W.B.; Malina, R.M.; Blimkie, C.J.; Daniels, S.R.; Dishman, R.K.; Gutin, B.; Hergenroeder, A.C.; Must, A.; Nixon, P.A.; Pivarnik, J.M.; et al. Evidence based physical activity for school-age youth. J. Pediatr. 2005, 146, 732–737. [Google Scholar] [CrossRef]
- Gallahue, D.L.; Ozmun, J.C.; Goodway, J.D. Understanding Motor Development: Infants, Children, Adolescents, Adults; McGraw-Hill: New York, NY, USA, 2012. [Google Scholar]
- Stodden, D.F.; Lagendorfer, S.J.; Roberton, M.A.; Rudisill, M.E.; Garcia, C.; Garcia, L.E. A Developmental Perspective on the Role of Motor Skill Competence in Physical Activity: An Emergent Relationship. Quest 2008, 60, 290–306. [Google Scholar] [CrossRef]
- Metcalfe, J.; Clark, J. The mountain of motor development: A metaphor. Mot. Dev. Res. Rev. 2002, 2, 163–190. [Google Scholar]
- Seefeldt, V. Developmental motor patterns: Implications for elementary school physical education. In Psychology of Motor Behavior and Sport; Nadeau, C.H.W., Roberts, G., Eds.; Human Kinetics: Champaign, IL, USA, 1980; pp. 314–323. [Google Scholar]
- deMeester, A.; Stodden, D.F.; Goodway, J.D.; True, L.; Brian, A.; Ferkel, R.; Haerens, L. Identifying a motor proficiency barrier for meeting physical activity guidelines in children. J. Sci. Med. Sport 2018, 21, 58–62. [Google Scholar] [CrossRef]
- Barnett, L.M.; Webster, E.K.; Hulteen, R.M.; De Meester, A.; Valentini, N.C.; Lenoir, M.; Pesce, C.; Getchell, N.; Lopes, V.P.; Robinson, L.E.; et al. Through the Looking Glass: A Systematic Review of Longitudinal Evidence, Providing New Insight for Motor Competence and Health. Sports Med. 2022, 52, 875–920. [Google Scholar] [CrossRef] [PubMed]
- Robinson, L.E.; Stodden, D.F.; Barnett, L.M.; Lopes, V.P.; Logan, S.W.; Rodrigues, L.P.; D’Hondt, E. Motor Competence and its Effect on Positive Developmental Trajectories of Health. Sports Med. 2015, 45, 1273–1284. [Google Scholar] [CrossRef] [PubMed]
- Spessato, B.C.; Gabbard, C.; Robinson, L.; Valentini, N.C. Body mass index, perceived and actual physical competence: The relationship among young children. Child. Care Health Dev. 2013, 39, 845–850. [Google Scholar] [CrossRef]
- Stodden, D.F.; Goodway, J.D. The Dynamic Association Between Motor Skill Development and Physical Activity. J. Phys. Educ. 2007, 78, 33–49. [Google Scholar] [CrossRef]
- den Uil, A.R.; Janssen, M.; Busch, V.; Kat, I.T.; Scholte, R.H.J. The relationships between children’s motor competence, physical activity, perceived motor competence, physical fitness and weight status in relation to age. PLoS ONE 2023, 18, e0278438. [Google Scholar] [CrossRef] [PubMed]
- Burton, A.M.; Cowburn, I.; Thompson, F.; Eisenmann, J.C.; Nicholson, B.; Till, K. Associations between Motor Competence and Physical Activity, Physical Fitness and Psychosocial Characteristics in Adolescents: A Systematic Review and Meta-analysis. Sports Med. 2023, 53, 2191–2256. [Google Scholar] [CrossRef]
- Burns, R.D.; Fu, Y. Testing the Motor Competence and Health-Related Variable Conceptual Model: A Path Analysis. J. Funct. Morphol. Kinesiol. 2018, 3, 61. [Google Scholar] [CrossRef]
- Khodaverdi, Z.; Bahram, A.; Stodden, D.; Kazemnejad, A. The relationship between actual motor competence and physical activity in children: Mediating roles of perceived motor competence and health-related physical fitness. J. Sports Sci. 2016, 34, 1523–1529. [Google Scholar] [CrossRef]
- Royo, E.; Latorre-Peña, J.; Denoni, M.; Orejudo, S. The Mediating Role Played by Perceived Motor Competence in the Relationship between Motor Competence and Physical Activity in Spanish Adolescents. Sustainability 2023, 15, 16327. [Google Scholar] [CrossRef]
- Haga, M. Physical fitness in children with high motor competence is different from that in children with low motor competence. Phys. Ther. 2009, 89, 1089–1097. [Google Scholar] [CrossRef]
- Stodden, D.F.; Roberton, M.A. The Association between Motor Skill Competence and Physical Fitness in Young Adults. Res. Q. Exerc. Sport 2009, 80, 223–229. [Google Scholar] [CrossRef]
- Wrotniak, B.H.; Epstein, L.H.; Dorn, J.M.; Jones, K.E.; Kondilis, V.A. The relationship between motor proficiency and physical activity in children. Pediatrics 2006, 118, e1758–e1765. [Google Scholar] [CrossRef] [PubMed]
- Lopes, V.P.; Rodrigues, L.P. The Role of Physical Fitness on the Relationship between Motor Competence and Physical Activity: Mediator or Moderator? J. Mot. Learn. Dev. 2021, 9, 456–469. [Google Scholar] [CrossRef]
- Cattuzzo, M.T.; Dos Santos Henrique, R.; Re, A.H.; de Oliveira, I.S.; Melo, B.M.; de Sousa Moura, M.; de Araujo, R.C.; Stodden, D. Motor competence and health related physical fitness in youth: A systematic review. J. Sci. Med. Sport 2016, 19, 123–129. [Google Scholar] [CrossRef] [PubMed]
- D’Hondt, E.; Deforche, B.; Gentier, I.; De Bourdeaudhuij, I.; Vaeyens, R.; Philippaerts, R.; Lenoir, M. A longitudinal analysis of gross motor coordination in overweight and obese children versus normal-weight peers. Int. J. Obes. 2013, 37, 61–67. [Google Scholar] [CrossRef] [PubMed]
- Gentier, I.; D’Hondt, E.; Shultz, S.; Deforche, B.; Augustijn, M.; Hoorne, S.; Verlaecke, K.; De Bourdeaudhuij, I.; Lenoir, M. Fine and gross motor skills differ between healthy-weight and obese children. Res. Dev. Disabil. 2013, 34, 4043–4051. [Google Scholar] [CrossRef]
- Morrison, K.M.; Cairney, J.; Eisenmann, J.; Pfeiffer, K.; Gould, D. Associations of Body Mass Index, Motor Performance, and Perceived Athletic Competence with Physical Activity in Normal Weight and Overweight Children. J. Obes. 2018, 2018, 3598321. [Google Scholar] [CrossRef]
- Caspersen, C.J.; Powell, K.E.; Christenson, G.M. Physical activity, exercise, and physical fitness: Definitions and distinctions for health-related research. Public Health Rep. 1985, 100, 126–131. [Google Scholar] [PubMed]
- Bruininks, R.H.; Bruininks, B.D. Bruininks-Oseretsky Test of Motor Proficiency, 2nd ed.; Pearson: Bloomington, MN, USA, 2013. [Google Scholar]
- Harter, S. Effectance motivation reconsidered: Toward a developmental model. Hum. Dev. 1978, 21, 34–64. [Google Scholar] [CrossRef]
- Harter, S. The Perceived Competence Scale of Children. Child Dev. 1982, 53, 87–97. [Google Scholar] [CrossRef]
- Harter, S. Self-Perception Profile for Adolescents (SPPA). APA PsycTests 2012. [Google Scholar] [CrossRef]
- Hibbing, P.R.; Bassett, D.R.; Crouter, S.E. Modifying Accelerometer Cut-Points Affects Criterion Validity in Simulated Free-Living for Adolescents and Adults. Res. Q. Exerc. Sport 2020, 91, 514–524. [Google Scholar] [CrossRef]
- Brønd, J.C.; Arvidsson, D. Sampling frequency affects the processing of Actigraph raw acceleration data to activity counts. J. Appl. Physiol. 2016, 120, 362–369. [Google Scholar] [CrossRef]
- Evenson, K.R.; Catellier, D.J.; Gill, K.; Ondrak, K.S.; McMurray, R.G. Calibration of two objective measures of physical activity for children. J. Sports Sci. 2008, 26, 1557–1565. [Google Scholar] [CrossRef]
- Rich, C.; Geraci, M.; Griffiths, L.; Sera, F.; Dezateux, C.; Cortina-Borja, M. Quality control methods in accelerometer data processing: Defining minimum wear time. PLoS ONE 2013, 8, e67206. [Google Scholar] [CrossRef]
- The Cooper Institute. FITNESSGRAM/ACTIVITYGRAM Test Administration Manual; The Cooper Institute: Dallas, TX, USA, 2013. [Google Scholar]
- Kuczmarski, R.J.; Ogden, C.L.; Guo, S.S.; Grummer-Strawn, L.M.; Flegal, K.M.; Mei, Z.; Wei, R.; Curtin, L.R.; Roche, A.F.; Johnson, C.L. 2000 CDC Growth Charts for the United States: Methods and development. Vital Health Stat. 11 2002, 246, 1–190. [Google Scholar]
- Mirwald, R.L.; Baxter-Jones, A.D.; Bailey, D.A.; Beunen, G.P. An assessment of maturity from anthropometric measurements. Med. Sci. Sports Exerc. 2002, 34, 689–694. [Google Scholar] [CrossRef] [PubMed]
- Biddle, S.J.; Whitehead, S.H.; Nevill, M.E. Correlates of participation in physical activity for adolescent girls: A systematic review of recent literature. J. Phys. Act. Health 2005, 2, 423–434. [Google Scholar] [CrossRef]
- Davison, K.K.; Schmalz, D.L.; Downs, D.S. Hop, skip…no! Explaining adolescent girls’ disinclination for physical activity. Ann. Behav. Med. 2010, 39, 290–302. [Google Scholar] [CrossRef] [PubMed]
- Morano, M.; Colella, D.; Rutigliano, I.; Fiore, P.; Pettoello-Mantovani, M.; Campanozzi, A. Changes in actual and perceived physical abilities in clinically obese children: A 9-month multi-component intervention study. PLoS ONE 2012, 7, e50782. [Google Scholar] [CrossRef]
- Pontifex, M.B.; Raine, L.B.; Johnson, C.R.; Chaddock, L.; Voss, M.W.; Cohen, N.J.; Kramer, A.F.; Hillman, C.H. Cardiorespiratory fitness and the flexible modulation of cognitive control in preadolescent children. J. Cogn. Neurosci. 2011, 23, 1332–1345. [Google Scholar] [CrossRef] [PubMed]
- Whitehead, S.H.; Biddle, S.J. Adolescent girls’ perceptions of physical activity: A focus group study. Eur. Phys. Educ. Rev. 2008, 14, 243–262. [Google Scholar] [CrossRef]
- Ensrud-Skraastad, O.K.; Haga, M. Associations between Motor Competence, Physical Self-Perception and Autonomous Motivation for Physical Activity in Children. Sports 2020, 8, 120. [Google Scholar] [CrossRef] [PubMed]
- Baghurst, T.M.; Mwavita, M. Preschool motor development predicting high school health-related physical fitness: A prospective study. Percept. Mot. Ski. Phys. Dev. Meas. 2014, 119, 279–291. [Google Scholar]
- Hands, B.; Larkin, D.; Parker, H.; Straker, L.; Perry, M. The relationship among physical activity, motor competence and health-related fitness in 14-year-old adolescents. Scand. J. Med. Sci. Sports 2009, 19, 655–663. [Google Scholar] [CrossRef]
- Rodrigues, L.P.; Stodden, D.F.; Lopes, V.P. Developmental pathways of change in fitness and motor competence are related to overweight and obesity status at the end of primary school. J. Sci. Med. Sport 2016, 19, 87–92. [Google Scholar] [CrossRef]
- Friel, C.P.; Duran, A.T.; Shechter, A.; Diaz, K.M. U.S. Children Meeting Physical Activity, Screen Time, and Sleep Guidelines. Am. J. Prev. Med. 2020, 59, 513–521. [Google Scholar] [CrossRef]
- Carrel, A.L.; Bowser, J.; White, D.; Moberg, D.P.; Weaver, B.; Hisgen, J.; Eickhoff, J.; Allen, D.B. Standardized childhood fitness percentiles derived from school-based testing. J. Pediatr. 2012, 161, 120–124. [Google Scholar] [CrossRef]

| Variable | Mean (SD) | n (%) |
|---|---|---|
| Age (y) | 12.2 (1.7) | |
| Mass (kg) | 50.5 (16.2) | |
| Height (cm) | 157.2 (13.1) | |
| BMI (kg/m2) | 20.0 (4.2) | |
| Weight Status | ||
| Underweight | 1 (2.1) | |
| Healthy Weight | 33 (70.2) | |
| Overweight | 10 (21.3) | |
| Obese | 3 (6.4) | |
| Maturity Offset | ||
| Pre-Peak Height Velocity | 42 (89.4) | |
| At-Peak Height Velocity | 3 (6.4) | |
| Post-Peak Height Velocity | 2 (4.3) | |
| Sex | ||
| Male | 26 (55.3) | |
| Female | 21 (44.7) | |
| Race | ||
| Caucasian | 47 (100) |
| Variable | Aerobic Capacity | Motor Competence | Perceived Motor Competence | MVPA |
|---|---|---|---|---|
| BMI | −0.295 * | −0.207 | −0.318 * | −0.358 * |
| Aerobic Capacity | 0.469 ** | 0.682 ** | 0.243 | |
| Motor Competence | 0.416 ** | −0.012 | ||
| Perceived Motor Competence | 0.212 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Coe, D.P.; Post, E.M.; Fitzhugh, E.C.; Fairbrother, J.T.; Webster, E.K. Associations among Motor Competence, Physical Activity, Perceived Motor Competence, and Aerobic Fitness in 10–15-Year-Old Youth. Children 2024, 11, 260. https://doi.org/10.3390/children11020260
Coe DP, Post EM, Fitzhugh EC, Fairbrother JT, Webster EK. Associations among Motor Competence, Physical Activity, Perceived Motor Competence, and Aerobic Fitness in 10–15-Year-Old Youth. Children. 2024; 11(2):260. https://doi.org/10.3390/children11020260
Chicago/Turabian StyleCoe, Dawn P., Emily M. Post, Eugene C. Fitzhugh, Jeffrey T. Fairbrother, and E. Kipling Webster. 2024. "Associations among Motor Competence, Physical Activity, Perceived Motor Competence, and Aerobic Fitness in 10–15-Year-Old Youth" Children 11, no. 2: 260. https://doi.org/10.3390/children11020260
APA StyleCoe, D. P., Post, E. M., Fitzhugh, E. C., Fairbrother, J. T., & Webster, E. K. (2024). Associations among Motor Competence, Physical Activity, Perceived Motor Competence, and Aerobic Fitness in 10–15-Year-Old Youth. Children, 11(2), 260. https://doi.org/10.3390/children11020260