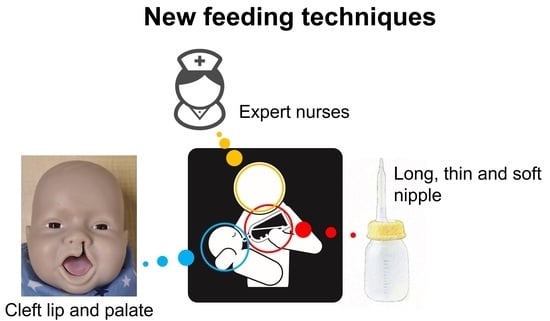
The Kumagai Method Utilizing the Pigeon Bottle Feeder with a Long Nipple: A Descriptive Study for the Development of Feeding Techniques for Children with Cleft Lip and/or Palate
Abstract
:1. Introduction
2. Materials and Methods
2.1. Design
2.2. Study Setting
2.3. Participants
2.4. Data Collection
2.5. Data Analysis
2.6. Rigor Enhancement
2.7. Ethical Considerations
3. Results
3.1. Characteristics of Participants
3.2. Goals of the Kumagai Method
I defined the word “chokubo-zui” to describe that the child’s tongue is shaped like a U and that the nipple is caught by the entire tongue to create negative pressure for drinking. A healthy child drinks breast milk in a similar way; the tongue is shaped like a U, setting the nipple into a wave-like motion when drinking. A child without a cleft palate does this when drinking. It is the correct way to drink, or maybe I should say that it is similar to breastfeeding, which increases the child’s level of satisfaction. When the “chokubo-zui” begins to appear, the child’s sucking becomes more stable, and the necessary amount of milk can be obtained. Therefore, the Kumagai method aims to induce this “chokubo-zui”.(Participant D)
I believe that only when all the Kumagai method I have described are performed carefully, will the child accept the nipple and be able to drink by self-sucking with his lips tightly closed. Drinking milk with the mouth closed indicates that the child has accepted the nipple.(Participant C)
3.3. Basic Posture
The child’s body should be held as straight as possible without directing the chin too much upward or downward. Ideally, the angle of the child’s body should be in a slightly upright position. The reason for this approach is that the nipple must be inserted into the mouth so that the tongue and nipple are parallel, and if the child’s body leans back too much, the nipple must be tilted down to keep it parallel with the tongue. If you do this, milk will automatically drip down, and the child will have a negative perception of the nipple. The important part is to keep the nipple and the tongue parallel, which is why I hold the child at this angle.(Participant B)
3.4. How to Hold the Bottle
When I use this Long Nipple for a child with swallowing problems, I take care of the direction of the nipple hole. When attaching the nipple to the holder, make sure the nipple hole does not point downward. Ideally, the nipple hole should be on the right or left side, but it is good enough if the hole position is not downward. The milk squirts onto the side of the nipple where the hole is. If the hole is facing down, the milk streams directly toward the child’s throat, which is dangerous. If the child can drink without choking, you do not need to worry much about the direction of the hole.(Participant A)
This (pinching) position should be in the center of the nipple where the nipple is thicker. The reason for holding at this location is because it produces the least amount of shaking. The nipple should be inserted in a taut, pinned position by maintaining the nipple like a stick so that it does not bend. The finger (holding the nipple) should be as relaxed as possible. By slightly curling the finger, unnecessary force from the finger is prevented, and the tongue movement is better transmitted. By keeping the fingers relaxed, the child’s lips and mouth will be free from unnecessary force.(Participant E)
3.5. Nipple Insertion into the Mouth
Bring the nipple horizontally to the child’s lips. If the nipple is tilted toward the tongue, milk will flow.(Participant B)
First, gently place the nipple against the lower lip. Once the mouth is open, insert the nipple while tilting the nipple so that it is centered on the tongue to ensure contact of the nipple with the lip and the tongue. Placing the nipple on the lower lip, then inserting the nipple along the surface of the tongue will trigger the sucking reflex and smoothly start the sucking.(Participant E)
The angles of the nipple are important, and how to achieve the angles with the arm holding the bottle is also important. Instead of raising the elbow to set the insertion angle, the angle should be set with the wrist only. This action makes it easier for us to manage the angle and facilitates feeding.(Participant A)
Generally, if you place this nipple at the center of the tongue, it will lead to a waving motion of the child’s tongue. Additionally, the child’s tongue wraps around the nipple in a U-shape, and the position of the nipple in the oral cavity becomes more stable. So you should place the nipple straight at the center of the tongue.(Participant E)
The just point, we have said, is the depth of insertion of the nipple into the mouth; the nipple is inserted 2 or 3 millimeters beyond the border where the nipple thickens. Insertion of the nipple beyond the just point induces the vomiting reflex. Moreover, when the child raises the tongue during sucking, the nipple may bend in the mouth and touch the palate, making the child reluctant to continue. If the insertion is too shallow, only a very small amount of milk is released when sucking. The tongue may also feel the sharp tip of the nipple, making the child more reluctant to proceed.(Participant D)
The nipple should remain straight, not bent or flexed; when the two fingers pinch the nipple, each finger should pinch with the same force, and the fingers should always stay in contact with the nipple even when the pressure is released.(Participant D)
Place the nipple on the lower lip (tap), put it in the mouth (swim), and pinch the nipple to push the milk out (push). The time of this “tap, swim, push” sequence is approximately 2 seconds. If you are too slow to insert the nipple, you will miss the time when the child desires to drink.(Participant B)
3.6. Maintaining Feeding
When the mouth is not closed, the child might be somewhat uncomfortable, so I try again to insert the nipple correctly.(Participant B)
Always watch the child’s breathing when you push the nipple. We observe at what interval the child breathes and assess how much milk should be released continuously. We should control the amount of milk released according to the child’s breathing.(Participant C)
I need to adjust the feeding speed until the child accepts the Long Nipple. The child will not be satisfied if the feeding is over in 5 min; meanwhile, sloppy drinking over 30 min will tire the mother.(Participant D)
3.7. End of Feeding
It is poor practice to let the nipple bounce or pull it out against the upper lip while removing. If this is done before the child accepts the nipple, the child will feel discomfort. If the nipple is bent, milk will flow out. Therefore, if the tip of the nipple hits the mouth while removing the nipple, milk will enter the mouth, and the child will gag. If the nipple is filled with milk, milk will not flow out unless the feeding angle is changed. If the angle is changed or the nipple is bent, milk will come out unintentionally and may splash on the child’s face or enter the mouth, making the child feel uncomfortable.(Participant D)
4. Discussion
4.1. Strengths and Limitations of the Work
4.2. Further Research
4.3. Implications for Policy and Practice
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Elad, D.; Kozlovsky, P.; Blum, O.; Laine, A.F.; Po, M.J.; Botzer, E.; Dollberg, S.; Zelicovich, M.; Sira, L.B. Biomechanics of milk extraction during breast-feeding. Proc. Natl. Acad. Sci. USA 2014, 111, 5230–5235. [Google Scholar] [CrossRef] [PubMed]
- Geddes, D.T.; Kent, J.C.; Mitoulas, L.R.; Hartmann, P.E. Tongue movement and intra-oral vacuum in breastfeeding infants. Early Hum. Dev. 2008, 84, 471–477. [Google Scholar] [CrossRef] [PubMed]
- Watkins, S.E.; Meyer, R.E.; Strauss, R.P.; Aylsworth, A.S. Classification, epidemiology, and genetics of orofacial clefts. Clin. Plast. Surg. 2014, 41, 149–163. [Google Scholar] [CrossRef] [PubMed]
- Michael, A.I.; Olorunfemi, G.; Olusanya, A.; Oluwatosin, O. Trends of cleft surgeries and predictors of late primary surgery among children with cleft lip and palate at the University College Hospital, Nigeria: A retrospective cohort study. PLoS ONE 2023, 18, e0274657. [Google Scholar] [CrossRef] [PubMed]
- Reid, J.; Reilly, S.; Kilpatrick, N. Sucking performance of babies with cleft conditions. Cleft Palate Craniofacial J. 2007, 44, 312–320. [Google Scholar] [CrossRef] [PubMed]
- Augsornwan, D.; Pattangtanang, P.; Surakunprapha, P. Development of information system for patients with cleft lip and palate undergoing operation. J. Med. Assoc. Thai 2015, 98, S151–S157. [Google Scholar]
- Green, M.A.; Resnick, C.M. Feeding considerations for infants with craniofacial malformations. Semin. Fetal Neonatal Med. 2021, 26, 101280. [Google Scholar] [CrossRef]
- Kaye, A.; Thaete, K.; Snell, A.; Chesser, C.; Goldak, C.; Huff, H. Initial nutritional assessment of infants with cleft lip and/or palate: Interventions and return to birth weight. Cleft Palate Craniofacial J. 2017, 54, 127–136. [Google Scholar] [CrossRef]
- Baylis, A.L.; Pearson, G.D.; Hall, C.; Madhoun, L.L.; Cummings, C.; Neal, N.; Smith, A.; Eastman, K.; Stocker, C.; Kirschner, R.E. A quality improvement initiative to improve feeding and growth of infants with cleft lip and/or palate. Cleft Palate Craniofacial J. 2018, 5, 1218–1224. [Google Scholar] [CrossRef]
- Gailey, D.G. Feeding infants with cleft and the postoperative cleft management. Oral Maxillofac. Surg. Clin. North. Am. 2016, 28, 153–159. [Google Scholar] [CrossRef]
- Nasar, F.; Amer, S.; Aly, H. Feeding protocol for mothers having infant with cleft lip and cleft palate. Am. J. Nurs. 2018, 7, 62–71. [Google Scholar] [CrossRef]
- Shahzad, F.; Sanati-Mehrizy, P. Feeding protocol in cleft palate patients. In Surgical Atlas of Cleft Palate and Palatal Fistulae; Fayyaz, G.Q., Ed.; Springer: Singapore, 2022; pp. 1–14. [Google Scholar] [CrossRef]
- Srivastav, S.; Duggal, I.; Duggal, R.; Tewari, N.; Chaudhari, P.K.; Pandey, R.M. Parental response to the feeding behavior problems in children with cleft lip and palate: A systematic review. Spec. Care Dentist 2021, 41, 559–571. [Google Scholar] [CrossRef] [PubMed]
- Sharma, S. Feeding intervention for cleft lip and palate child. J. Emerg. Technol. Innov. Res. 2020, 7, 1347–1351. [Google Scholar]
- Ueki, S.; Fujita, A.; Kumagai, Y.; Hirai, Y.; Tashiro, E.; Miyata, J. Bottle-feeding techniques for children with cleft lip and palate experiencing feeding difficulties. Int. J. Nurs. Sci. 2023, 10, 82–88. [Google Scholar] [CrossRef] [PubMed]
- Zajac, D.J.; Vallino, L.D. Evaluation and Management of Cleft Lip and Palate: A Developmental Perspective, 1st ed.; Plural Publishing: San Diego, CA, USA, 2017. [Google Scholar]
- Cooper-Brown, L.; Copeland, S.; Dailey, S.; Downey, D.; Petersen, M.C.; Stimson, C.; Van Dyke, D.C. Feeding and swallowing dysfunction in genetic syndromes. Dev. Disabil. Res. Rev. 2008, 14, 147–157. [Google Scholar] [CrossRef] [PubMed]
- Jindal, K.M.; Khan, S.Y. How to feed cleft patient? Int. J. Clin. Pediatr. Dent. 2012, 6, 100–103. [Google Scholar] [CrossRef] [PubMed]
- Naveen, B.H.; Prasad, R.S.; Kashinath, K.R.; Kumar, S.; Kalavathi, S.D.; Laishram, N. An innovative modified feeding appliance for an infant with cleft lip and cleft palate: A case report. J. Family Med. Prim. Care 2019, 8, 2134–2136. [Google Scholar] [CrossRef] [PubMed]
- Vaismoradi, M.; Turunen, H.; Bondas, T. Content analysis and thematic analysis: Implications for conducting a qualitative descriptive study. Nurs. Health Sci. 2013, 15, 398–405. [Google Scholar] [CrossRef]
- Korstjens, I.; Moser, A. Series: Practical guidance to qualitative research. Part 4: Trustworthiness and publishing. Eur. J. Gen. Pract. 2018, 24, 120–124. [Google Scholar] [CrossRef]
- Kumagai, Y. Effectiveness of silicone long nipple for child with bilateral cleft lip and palate and feeding difficulty. Jpn. J. Perinat. Care 2021, 40, 1024–1031. [Google Scholar]
- Pigeon corporation. Cleft Lip and Palate Feeder. Available online: https://pigeon.com.my/product/cleft-lip-and-palate-feeder/ (accessed on 25 March 2023).
- Penny, C.; McGuire, C.; Bezuhly, M. A systematic review of feeding interventions for infants with cleft palate. Cleft Palate Craniofacial J. 2022, 59, 1527–1536. [Google Scholar] [CrossRef]
- Lau, C.; Smith, E.O.; Schanler, R.J. Coordination of suck-swallow and swallow respiration in preterm infants. Acta Paediatr. 2003, 92, 721–727. [Google Scholar] [CrossRef]
- Devi, E.S.; Sankar, A.J.S.; Kumar, M.G.M.; Sujatha, B. Maiden morsel—Feeding in cleft lip and palate infants. J. Int. Soc. Prev. Community Dent. 2012, 2, 31–37. [Google Scholar] [CrossRef]
- Brand, B.M. Cleft Lip and Palate Feeding Intervention: A Scoping Review. Master’s Thesis, Stellenbosch University, Stellenbosch, South Africa, March 2020. [Google Scholar]
- Oechsle, A.L.; Wiechers, C.; Abadie, V.; Abel, F.; Breugem, C.; Poets, C.F. Study protocol for a multicenter, multinational, observational registry of epidemiology, treatment and outcome of patients with Robin sequence. Head. Face Med. 2023, 19, 20. [Google Scholar] [CrossRef]
- Bielsa, V.F. Virtual reality simulation in plastic surgery training. Literature review. J. Plast. Reconstr. Aesthet. Surg. 2021, 74, 2372–2378. [Google Scholar] [CrossRef]
- Jallad, S.T.; Işık, B. The effectiveness of virtual reality simulation as learning strategy in the acquisition of medical skills in nursing education: A systematic review. Ir. J. Med. Sci. 2022, 191, 1407–1426. [Google Scholar] [CrossRef] [PubMed]



| General Bottle | PCPSB, Medela SNF | Syringe, Spoon, Cup | Long Nipple | |
|---|---|---|---|---|
| Method to facilitate milk extraction | The nipple is placed in the child’s mouth letting the child suckle | Bottle or nipple squeezing | The milk is poured into the child’s mouth | Unknown |
| Need for the child to create negative pressure for the milk to flow out | Yes | No | No | No |
| Nipple shape characteristics | Various sizes | Somewhat thick | No nipple | Thin and long |
| Cost | Varying | Expensive | Cheap | Cheap |
| (a) | |
| Category | Subcategory |
| Cuddling as if pulling the child toward oneself. |
|
| |
| |
| |
| Holding the child straight in a slightly upright position. |
|
| |
| (b) | |
| Category | Subcategory |
| Holding the bottle with three fingers. |
|
| |
| |
| Pinching the center of the nipple between the index and middle fingers. |
|
| |
| |
| Raw Data (Participant D) | Codes | Subcategories |
|---|---|---|
| I tuck the child’s arm under my armpit (1). That helps to keep the upper limbs in place (2) and the child’s body in close contact with my body (3). The arm is always tucked under the armpit. My hand provides support at the border between the child’s thigh and buttock (4). The important point is to make sure that the child’s nuchal region can be held in close contact with the V-shaped part (the inside) of the elbow joint (5). |
|
|
| (a) | |
| Category | Subcategory |
| Moving the bottle horizontally and lightly placing the nipple against the lower lip. |
|
| Placing the nipple into the mouth so that it adheres to the lower lip and the tongue. |
|
| |
| |
| |
| |
| |
| |
| |
| Pushing the milk out by pinching the nipple between the index and middle fingers. |
|
| |
| |
| (b) | |
| Category | Subcategory |
| Pinching the nipple in time with the sucking. |
|
| |
| |
| Adjusting the pinching force according to the child’s sucking ability. |
|
| |
| (c) | |
| Category | Subcategory |
| Pulling the nipple straight out. |
|
| |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Ueki, S.; Kumagai, Y.; Hirai, Y.; Nagatomo, E.; Miyauchi, S.; Inoue, T.; An, Q.; Miyata, J. The Kumagai Method Utilizing the Pigeon Bottle Feeder with a Long Nipple: A Descriptive Study for the Development of Feeding Techniques for Children with Cleft Lip and/or Palate. Children 2024, 11, 365. https://doi.org/10.3390/children11030365
Ueki S, Kumagai Y, Hirai Y, Nagatomo E, Miyauchi S, Inoue T, An Q, Miyata J. The Kumagai Method Utilizing the Pigeon Bottle Feeder with a Long Nipple: A Descriptive Study for the Development of Feeding Techniques for Children with Cleft Lip and/or Palate. Children. 2024; 11(3):365. https://doi.org/10.3390/children11030365
Chicago/Turabian StyleUeki, Shingo, Yukari Kumagai, Yumi Hirai, Eri Nagatomo, Shoko Miyauchi, Takuro Inoue, Qi An, and Junko Miyata. 2024. "The Kumagai Method Utilizing the Pigeon Bottle Feeder with a Long Nipple: A Descriptive Study for the Development of Feeding Techniques for Children with Cleft Lip and/or Palate" Children 11, no. 3: 365. https://doi.org/10.3390/children11030365
APA StyleUeki, S., Kumagai, Y., Hirai, Y., Nagatomo, E., Miyauchi, S., Inoue, T., An, Q., & Miyata, J. (2024). The Kumagai Method Utilizing the Pigeon Bottle Feeder with a Long Nipple: A Descriptive Study for the Development of Feeding Techniques for Children with Cleft Lip and/or Palate. Children, 11(3), 365. https://doi.org/10.3390/children11030365