Feeding Problems in Typically Developing Young Children, a Population-Based Study
Abstract
:1. Introduction
2. Material and Methods
2.1. Participants
2.2. Measures
2.2.1. Demographic and Anthropometric Data
2.2.2. Child’s Medical History
2.2.3. Behavioral Pediatrics Feeding Assessment Scale (BPFAS)
3. Statistical Analysis
4. Results
5. Discussion
6. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Acknowledgments
Conflicts of Interest
References
- Milano, K.; Chatoor, I.; Kerzner, B. A Functional Approach to Feeding Difficulties in Children. Curr. Gastroenterol. Rep. 2019, 21, 51. [Google Scholar] [CrossRef]
- Kerzner, B.; Milano, K.; MacLean, W.C.; Berall, G.; Stuart, S.; Chatoor, I. A practical approach to classifying and managing feeding difficulties. Pediatrics 2015, 135, 344–345. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Manikam, R.; Perman, J.A. Pediatric feeding disorders. J. Clin. Gastroenterol. 2000, 30, 34–46. [Google Scholar] [CrossRef] [PubMed]
- Berlin, K.; Davies, W.; Lobato, D.; Silverman, A. A Biopsychosocial Model of Normative and Problematic Pediatric Feeding. Child. Health Care 2009, 38, 263–282. [Google Scholar] [CrossRef]
- Estrem, H.H.; Pados, B.F.; Park, J.; Knafl, K.A.; Thoyre, S.M. Feeding problems in infancy and early childhood: Evolutionary concept analysis. J. Adv. Nurs. 2017, 73, 56–70. [Google Scholar] [CrossRef]
- Ammaniti, M.; Lucarelli, L.; Cimino, S.; D′Olimpio, F.; Chatoor, I. Maternal psychopathology and child risk factors in infantile anorexia. Int. J. Eat. Disord. 2010, 43, 233–240. [Google Scholar] [CrossRef]
- Printza, A.; Goutsikas, C.; Triaridis, S.; Kyrgidis, A.; Haidopoulou, K.; Constantinidis, J.; Pavlou, E. Dysphagia diagnosis with questionnaire, tongue strength measurement, and FEES in patients with childhood-onset muscular dystrophy. Int. J. Pediatr. Otorhinolaryngol. 2019, 117, 198–203. [Google Scholar] [CrossRef] [PubMed]
- Taylor, C.M.; Wernimont, S.M.; Northstone, K.; Emmett, P.M. Picky/fussy eating in children: Review of definitions, assessment, prevalence and dietary intakes. Appetite 2015, 95, 349–359. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Brown, C.L.; Vander Schaaf, E.B.; Cohen, G.M.; Irby, M.B.; Skelton, J.A. Association of Picky Eating and Food Neophobia with Weight: A Systematic Review. Child. Obes. 2016, 12, 247–262. [Google Scholar] [CrossRef] [Green Version]
- Goh, D.Y.; Jacob, A. Perception of picky eating among children in Singapore and its impact on caregivers: A questionnaire survey. Asia Pac. Fam. Med. 2012, 11, 5. [Google Scholar] [CrossRef] [Green Version]
- Marchi, M.; Cohen, P. Early childhood eating behaviors and adolescent eating disorders. J. Am. Acad. Child Adolesc. Psychiatry 1990, 29, 112–117. [Google Scholar] [CrossRef] [PubMed]
- Rydell, A.M.; Dahl, M.; Sundelin, C. Characteristics of school children who are choosy eaters. J. Genet. Psychol. 1995, 156, 217–229. [Google Scholar] [CrossRef] [PubMed]
- Reau, N.R.; Senturia, Y.D.; Lebailly, S.A.; Christoffel, K.K. Infant and toddler feeding patterns and problems: Normative data and a new direction. J. Dev. Behav. Pediatr. 1996, 17, 149–153. [Google Scholar] [CrossRef] [PubMed]
- Cerro, N.; Zeunert, S.; Simmer, K.N.; Daniels, L.A. Eating behaviour of children 1.5–3.5 years born preterm: Parents’ perceptions. J. Paediatr. Child Health 2002, 38, 72–78. [Google Scholar] [CrossRef] [PubMed]
- Jacobi, C.; Agras, W.S.; Bryson, S.; Hammer, L.D. Behavioral validation, precursors, and concomitants of picky eating in childhood. J. Am. Acad. Child Adolesc. Psychiatry 2003, 42, 76–84. [Google Scholar] [CrossRef]
- Esparo, G.; Canals, J.; Jane, C.; Ballespi, S.; Vinas, F.; Domenech, E. Feeding problems in nursery children: Prevalence and psychosocial factors. Acta Paediatr. 2004, 93, 663–668. [Google Scholar] [CrossRef]
- Dubois, L.; Farmer, A.; Girard, M.; Peterson, K.; Tatone-Tokuda, F. Problem eating behaviors related to social factors and body weight in preschool children: A longitudinal study. Int. J. Behav. Nutr. Phys. Act. 2007, 4, 1–10. [Google Scholar] [CrossRef] [Green Version]
- Wright, C.M.; Parkinson, K.N.; Shipton, D.; Drewett, R.F. How do toddler eating problems relate to their eating behavior, food preferences, and growth? Pediatrics 2007, 120, e1069–e1075. [Google Scholar] [CrossRef] [PubMed]
- Hittner, J.B.; Faith, M.S. Typology of emergent eating patterns in early childhood. Eat. Behav. 2011, 12, 242–248. [Google Scholar] [CrossRef]
- Micali, N.; Simonoff, E.; Elberling, H.; Rask, C.U.; Olsen, E.M.; Skovgaard, A.M. Eating patterns in a population-based sample of children aged 5 to 7 years: Association with psychopathology and parentally perceived impairment. J. Dev. Behav. Pediatr. 2011, 32, 572–580. [Google Scholar] [CrossRef]
- Benjasuwantep, B.; Chaithirayanon, S.; Eiamudomkan, M. Feeding problems in healthy young children: Prevalence, related factors and feeding practices. Pediatr. Rep. 2013, 5, 38–42. [Google Scholar] [CrossRef] [Green Version]
- Dubois, L.; Diasparra, M.; Bédard, B.; Kaprio, J.; Fontaine-Bisson, B.; Tremblay, R.; Pérusse, D. Genetic and environmental influences on eating behaviors in 2.5-and 9-year-old children: A longitudinal twin study. Int. J. Behav. Nutr. Phys. Act. 2013, 10, 1–12. [Google Scholar] [CrossRef] [Green Version]
- Hafstad, G.S.; Abebe, D.S.; Torgersen, L.; von Soest, T. Picky eating in preschool children: The predictive role of the child’s temperament and mother’s negative affectivity. Eat. Behav. 2013, 14, 274–277. [Google Scholar] [CrossRef] [PubMed]
- Equit, M.; Pälmke, M.; Becker, N.; Moritz, A.M.; Becker, S.; von Gontard, A. Eating problems in young children—A population-based study. Acta Paediatr. 2013, 102, 149–155. [Google Scholar] [CrossRef] [PubMed]
- Tharner, A.; Jansen, P.W.; Kiefte-de Jong, J.C.; Moll, H.A.; van der Ende, J.; Jaddoe, V.W.; Franco, O.H. Toward an operative diagnosis of fussy/picky eating: A latent profile approach in a population-based cohort. Int. J. Behav. Nutr. Phys. Act. 2014, 11, 1–11. [Google Scholar] [CrossRef] [Green Version]
- Haszard, J.J.; Skidmore, P.M.; Williams, S.M.; Taylor, R.W. Associations between parental feeding practices, problem food behaviours and dietary intake in New Zealand overweight children aged 4–8 years. Public Health Nutr. 2015, 18, 1036–1043. [Google Scholar] [CrossRef] [Green Version]
- American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders, 5th ed.; American Psychiatric Pub: Arlington, VA, USA, 2013; ISBN 9780890425558. [Google Scholar]
- Dovey, T.M.; Kumari, V.; Blissett, J. Mealtime Hostage Parent Science Gang. Eating behaviour, behavioural problems and sensory profiles of children with avoidant/restrictive food intake disorder (ARFID), autistic spectrum disorders or picky eating: Same or different? Eur. Psychiatry 2019, 61, 56–62. [Google Scholar] [CrossRef] [PubMed]
- Katzman, D.K.; Norris, M.L.; Zucker, N. Avoidant Restrictive Food Intake Disorder. Psychiatr. Clin. N. Am. 2019, 42, 45–57. [Google Scholar] [CrossRef] [PubMed]
- Strand, M.; von Hausswolff-Juhlin, Y.; Welch, E. A systematic scoping review of diagnostic validity in avoidant/restrictive food intake disorder. Int. J. Eat. Disord. 2019, 52, 331–360. [Google Scholar] [CrossRef] [PubMed]
- Eddy, K.T.; Thomas, J.J. Introduction to a special issue on child and adolescent feeding and eating disorders and avoidant/restrictive food intake disorder. Int. J. Eat. Disord. 2019, 52, 327–330. [Google Scholar] [CrossRef]
- Bourne, L.; Bryant-Waugh, R.; Cook, J.; Mandy, W. Avoidant/restrictive food intake disorder: A systematic scoping review of the current literature. Psychiatry Res. 2020, 288, 112961. [Google Scholar] [CrossRef] [PubMed]
- Hay, P.; Mitchison, D.; Collado, A.E.L.; González-Chica, D.A.; Stocks, N.; Touyz, S. Burden and health-related quality of life of eating disorders, including Avoidant/Restrictive Food Intake Disorder (ARFID), in the Australian population. J. Eat. Disord. 2017, 5, 21. [Google Scholar] [CrossRef] [PubMed]
- Gonçalves, S.; Vieira, A.I.; Machado, B.C.; Costa, R.; Pinheiro, J.; Conceiçao, E. Avoidant/restrictive food intake disorder symptoms in children: Associations with child and family variables. Child Health Care 2018, 48, 1–13. [Google Scholar] [CrossRef]
- Chen, Y.L.; Chen, W.J.; Lin, K.C.; Shen, L.J.; Gau, S.S. Prevalence of DSM-5 mental disorders in a nationally representative sample of children in Taiwan: Methodology and main findings. Epidemiol. Psychiatr. Sci. 2019, 29, e15. [Google Scholar] [CrossRef]
- World Health Organization. The ICD-10 Classification of Mental and Behavioural Disorders: Clinical Descriptions and Diagnostic Guidelines; World Health Organization: Geneva, Switzerland, 1992. [Google Scholar]
- Goday, P.S.; Huh, S.Y.; Silverman, A.; Lukens, C.T.; Dodrill, P.; Cohen, S.S.; Phalen, J.A. Pediatric feeding disorder: Consensus definition and conceptual framework. J. Pediatr. Gastroenterol. Nutr. 2019, 68, 124–129. [Google Scholar] [CrossRef]
- Sanchez, K.; Spittle, A.J.; Allinson, L.; Morgan, A. Parent questionnaires measuring feeding disorders in preschool children: A systematic review. Dev. Med. Child Neurol. 2015, 57, 798–807. [Google Scholar] [CrossRef] [Green Version]
- Crist, W.; McDonnell, P.; Beck, M.; Gillespie, C.T.; Barrett, P.; Mathews, J. Behavior at mealtimes and the young child with cystic fibrosis. J. Dev. Behav. Pediatr. 1994, 15, 157–161. [Google Scholar] [CrossRef]
- Dovey, T.M.; Martin, C.I.; Alridge, V.K.; Haycraft, E.; Meyer, C. Measures, measures everywhere, but which one should I use. Feed. News 2011, 6, 1–13. [Google Scholar]
- Mitchell, M.J.; Powers, S.W.; Byars, K.C.; Dickstein, S.; Stark, L.J. Family functioning in young children with cystic fibrosis: Observations of interactions at mealtime. J. Dev. Behav. Pediatr. 2004, 25, 335–346. [Google Scholar] [CrossRef] [PubMed]
- Marshall, J.; Raatz, M.; Ward, E.C.; Dodrill, P. Use of parent report to screen for feeding difficulties in young children. J. Paediatr. Child Health 2015, 51, 307–313. [Google Scholar] [CrossRef] [Green Version]
- Davis, A.M.; Canter, K.S.; Stough, C.O.; Gillette, M.D.; Patton, S. Measurement of mealtime behaviors in rural overweight children: An explorato-ry factor analysis of the Behavioral Pediatrics Feeding Assessment Scale. J. Pediatr. Psychol. 2014, 39, 332–339. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Patton, S.R.; Dolan, L.M.; Powers, S.W. Parent report of mealtime behaviors in young children with type 1 diabetes mellitus: Implications for better assessment of dietary adherence problems in the clinic. J. Dev. Behav. Pediatr. 2006, 27, 202–208. [Google Scholar] [CrossRef] [PubMed]
- Wu, Y.P.; Franciosi, J.P.; Rothenberg, M.E.; Hommel, K.A. Behavioral feeding problems and parenting stress in eosinophilic gastrointestinal disorders in children. Pediatr. Allergy Immunol. 2012, 23, 730–735. [Google Scholar] [CrossRef]
- Dovey, T.M.; Jordan, C.; Aldridge, V.K.; Martin, C.I. Screening for feeding disorders. Creating critical values using the behavioral pediatrics feeding assessment scale. Appetite 2013, 69, 108–113. [Google Scholar] [CrossRef] [PubMed]
- WHO. WHO Anthro for Personal Computers, Software for Assessing Growth and Development of the World’s Children, Version 3.2.2, 2011; WHO: Geneva, Switzerland, 2010; Available online: http://www.who.int/childgrowth/software/en/ (accessed on 22 February 2020).
- WHO. WHO AnthroPlus for Personal Computers Manual: Software for Assessing Growth of the World’s Children and Adolescents; WHO: Geneva, Switzerland, 2009; Available online: http://www.who.int/growthref/tools/en/ (accessed on 22 February 2020).
- Crist, W.; Napier-Phillips, A. Mealtime Behaviors of Young Children: A Comparison of Normative and Clinical Data. J. Dev. Behav. Pediatr. 2001, 22, 279–286. [Google Scholar] [CrossRef]
- Dovey, T.M.; Martin, C.I. A parent-led contingent reward desensitisation intervention for children with a feeding problem resulting from sensory defensiveness. Infant Child Adolesc. Nutr. 2012, 4, 384–393. [Google Scholar] [CrossRef]
- Dovey, T.M.; Martin, C.I. A quantitative psychometric evaluation of an intervention for poor dietary variety in children with a feeding problem of clinical significance. Infant Ment. Health J. 2012, 33, 148–162. [Google Scholar] [CrossRef]
- Allen, S.L.; Smith, I.M.; Duku, E.; Vaillancourt, T.; Szatmari, P.; Bryson, S.; Fombonne, E.; Volden, J.; Waddell, C.; Zwaigenbaum, L.; et al. Behavioral Pediatrics Feeding Assessment Scale in Young Children With Autism Spectrum Disorder: Psychometrics and Associations With Child and Parent Variables. J. Pediatr. Psychol. 2015, 40, 581–590. [Google Scholar] [CrossRef] [Green Version]
- Sdravou, K.; Evangeliou, A.; Tentzidou, K.; Sotiriadou, F.; Stasinou, E.; Fotoulaki, M. The behaviouralpaediatrics feeding assessment scale is a reliable and valid tool for Greek children. Acta Paediatr. 2018, 107, 1653–1654. [Google Scholar] [CrossRef]
- Sdravou, K.; Emmanouilidou-Fotoulaki, E.; Printza, A.; Andreoulakis, E.; Evangeliou, A.; Fotoulaki, M. Mealtime Environment and Control of Food Intake in Healthy Children and in Children with Gastrointestinal Diseases. Children 2021, 8, 77. [Google Scholar] [CrossRef] [PubMed]
- Sdravou, K.; Andreoulakis, E.; Printza, A.; Sotiriadou, F.; Evangeliou, A.; Fotoulaki, M. Parental management of feeding problems in young children-a population-based study. Int. J. Pediatr. Otorhinolaryngol. 2020, 136, 110162. [Google Scholar] [CrossRef] [PubMed]
- Machado, B.C.; Dias, P.; Lima, V.S.; Campos, J.; Gonçalves, S. Prevalence and correlates of picky eating in preschool-aged children: A popula-tion-based study. Eat. Behav. 2016, 22, 16–21. [Google Scholar] [CrossRef] [PubMed]
- Hodder, R.K.; O’Brien, K.M.; Stacey, F.G.; Tzelepis, F.; Wyse, R.J.; Bartlem, K.M.; Sutherland, R.; James, E.L.; Barnes, C.; Wolfenden, L. Interventions for increasing fruit and vegetable consumption in children aged five years and under. Cochrane Database Syst. Rev. 2020, 25, CD008552. [Google Scholar] [CrossRef]
- Inchley, J.C.; Currie, D.B.; Young, T.; Samdal, O.; Torsheim, T.; Augustson, L. Growing Up Unequal: Gender and Socioeconomic Differences in Young People’s Health and Well-Being: Health Behaviour in School-Aged Children (HBSC) Study: International Report from the 2013/2014 Survey; Health Policy for Children and Adolescents, 7; WHO Regional Office for Europe: Copenhagen, Denmark, 2016; p. 277. [Google Scholar]
- Torres, T.O.; Gomes, D.R.; Mattos, M.P. Factors associated with food neophobia in children: Systematic review. Rev. Paul. Pediatr. 2020, 39, e2020089. [Google Scholar] [CrossRef]
- Łoboś, P.; Januszewicz, A. Food neophobia in children. Pediatr. Endocrinol. Diabetes. Metab. 2019, 25, 150–154. [Google Scholar] [CrossRef] [PubMed]
- Nieuwenhuis, T.; Verhagen, E.A.; Bos, A.F.; van Dijk, M.W. Children born preterm and full term have similar rates of feeding problems at three years of age. Acta Paediatr. 2016, 105, e452–e457. [Google Scholar] [CrossRef]
- Phalen, J.A. Managing feeding problems and feeding disorders. Pediatrics Rev. 2013, 34, 549–557. [Google Scholar] [CrossRef]
- Silverman, A.H. Interdisciplinary care for feeding problems in children. Nutr. Clin. Pract. 2010, 25, 160–165. [Google Scholar] [CrossRef] [PubMed]
- Tanner, A.; Andreone, B.E. Using graduated exposure and differential reinforcement to increase food repertoire in a child with autism. Behav. Anal. Pract. 2015, 8, 233–240. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Valdimarsdóttir, H.; Halldórsdóttir, L.Y.; Sigurthardóttir, Z.G. Increasing the variety of foods consumed by a picky eater: Generalization of effects across caregivers and settings. J. Appl. Behav. Anal. 2010, 43, 101–105. [Google Scholar] [CrossRef] [Green Version]
- Coulthard, H.; Sealy, A. Play with your food! Sensory play is associated with tasting of fruits and vegetables in preschool children. Appetite 2017, 113, 84–90. [Google Scholar] [CrossRef] [PubMed]
- Højer, R.; Wistoft, K.; Frøst, M.B. Play with Your Food and Cook It! Tactile Play with Fish as a Way of Promoting Acceptance of Fish in 11- to 13-Year-Old Children in a School Setting-A Qualitative Study. Nutrients 2020, 12, 3180. [Google Scholar] [CrossRef] [PubMed]
- Aldridge, V.K.; Dovey, T.M.; Martin, C.I.; Meyer, C. Identifying clinically relevant feeding problems and disorders. J. Child Health Care 2010, 14, 261–270. [Google Scholar] [CrossRef]
- Ramsay, M.; Martel, C.; Porporino, M.; Zygmuntowicz, C. The Montreal Children’s Hospital Feeding Scale: A brief bilingual screening tool for identifying feeding problems. Paediatr. Child Health 2011, 16, 147–e17. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Migraine, A.; Nicklaus, S.; Parnet, P.; Lange, C.; Monnery-Patris, S.; Des Robert, C.; Darmaun, D.; Flamant, C.; Amarger, V.; Roze, J.C. Effect of preterm birth and birth weight on eating behavior at 2 y of age. Am. J. Clin. Nutr. 2013, 97, 1270–1277. [Google Scholar] [CrossRef] [Green Version]
- Hendricks, K.; Briefel, R.; Novak, T.; Ziegler, P. Maternal and Child Characteristics Associated with Infant and Toddler Feeding Practices. J. Acad. Nutr. Diet. 2006, 106, 135–148. [Google Scholar] [CrossRef]
- Cassells, E.L.; Magarey, A.M.; Daniels, L.A.; Mallan, K.M. The influence of maternal infant feeding practices and beliefs on the expression of food neophobia in toddlers. Appetite 2014, 82, 36–42. [Google Scholar] [CrossRef] [Green Version]
- Brinksma, A.; Sulkers, E.; IJpma, I.; Burgerhof, J.G.M.; Tissing, W.J.E. Eating and feeding problems in children with cancer: Prevalence, related factors, and consequences. Clin. Nutr. 2020, 39, 3072–3079. [Google Scholar] [CrossRef]
- Powers, S.W.; Patton, S.R.; Byars, K.C.; Mitchell, M.J.; Jelalian, E.; Mulvihill, M.M.; Hovell, M.F.; Stark, L.J. Caloric intake and eating behavior in infants and toddlers with cystic fibrosis. Pediatrics 2002, 109, e75. [Google Scholar] [CrossRef] [Green Version]
| Study | Outcome Measure of Feeding Problem | Population (Participants, Age) | Country | Prevalence |
|---|---|---|---|---|
| Marchi and Cohen, 1990 [11] | Interview with mothers | 800 children 1–10 years old | USA | 29% |
| Rydell et al., 1995 [12] | Set of questions ** | 240 children 6.1–11.0 years old | Sweden | 30% |
| Reau et al., 1996 [13] | Set of questions | 130 infants 151 toddlers 13–27 months | USA | 33% of infants 52% of toddlers |
| Cerro et al., 2002 [14] | Set of questions | 95 children aged 1.5–3.5 years | New Zealand | 20% |
| Jacobi et al., 2003 [15] | Single question | 135 children 3.5–5.5 years | USA | 21% |
| Esparo et al., 2004 [16] | Set of questions | 851 children 3–6 years | Spain | 4.8% |
| Dubois et al., 2007 [17] | Set of questions | 1498 preschoolers, 2.5, 3.5, and 4.5 years old | Canada | 14–17% |
| Wright et al., 2007 [18] | Set of questions | 455 parents 30 months | UK | 8.3% |
| Hittner and Faith, 2011 [19] | Set of questions | 487 children 1 and 3 years old | USA | 9% |
| Micali et al., 2011 [20] | Set of questions | 1327 children 5 to 7 years old | Denmark | 7.3% picky eating 1.4% poor eating |
| Goh et al., 2012 [10] | Set of questions | 407 parents/grandparents of children aged 1 to 10 years | Singapore | 25.1% picky eating 15.2% difficulties |
| Benjasuwantep et al., 2013 [21] | Set of questions | 402 children Aged 1–4 years | Thailand | 26.9% |
| Dubois et al., 2013 [22] | Set of questions | 692 (346 twin siblings) 2.5 and 9 years old | Canada | 9.4% at 2.5 years 10.7% at 9 years |
| Hafstad et al., 2013 [23] | Set of questions | 913 children 1.5 to 4.5 years old | Norway | 22–35% |
| Equit et al., 2013 [24] | Set of questions | 1090 children 4–7 years old | Germany | 23.2% picky eating 4.8% food avoidance |
| Tharner et al., 2014 [25] | Child Eating Behavior Questionnaire (CEBQ) | 3117 children Aged 4 years old | The Netherlands | 5.8% |
| Haszardet al., 2015 [26] | Set of questions | 203 overweight children 4–8 years | New Zealand | 36.5% |
| Ν (%) | ||
|---|---|---|
| Child sex | Female | 372 (50.1) |
| Child age group | >5 years | 401 (54.0) |
| Only child | yes | 169 (22.8) |
| Firstborn | yes | 387 (52.2) |
| Parental sex | Female | 687 (92.6) |
| Parental age group | <40 years | 548 (73.9) |
| Parental education | >12 years | 408 (55.0) |
| Working parent | yes | 529 (71.3) |
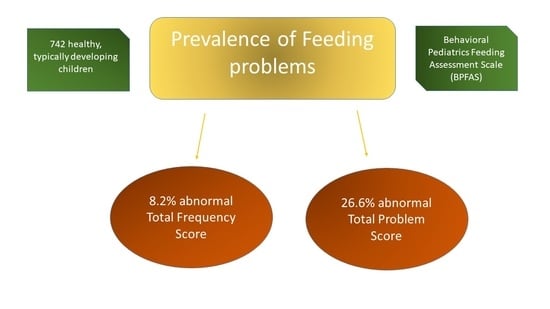
| TFS score by cut-off | >84 | 61 (8.2) |
| TPS score by cut-off | >9 | 189 (26.6) |
| Child’s age (years) | Mean ± SD Median (Q1, Q3) | 4.92 ± 1.00 5.17 (4.42, 5.67) |
| BMI z-score (current) | Mean ± SD Median (Q1, Q3) | 0.28 ± 1.41 0.24 (−0.57, 0.24) |
| Birth weight (grams) | Mean ± SD Median (Q1, Q3) | 3268.43 ± 444.80 3230 (3000, 3550) |
| TFS score | Mean ± SD Median (Q1, Q3) | 62.71 ± 14.23 60.00 (52.75, 70.00) |
| TPS score | Mean ± SD Median (Q1, Q3) | 6.23 ± 6.40 4.00 (1.00, 10.00) |
| TFS Score | TPS Score | |
|---|---|---|
| TFS | 0.713 (<0.001) | |
| TPS | 0.713 (<0.001) | |
| Child age | 0.053 (0.150) | 0.083 (0.026) |
| zBMI | −0.131 (0.001) | −0.106 (0.006) |
| Birth Weight | −0.048 (0.191) | −0.030 (0.417) |
| TFS | TPS | ||||||||
|---|---|---|---|---|---|---|---|---|---|
| TFS ≤ 84 Ν = 681 Ν (%) | TFS > 84 Ν = 61 Ν (%) | Chi Square | p | TPS ≤ 9 Ν = 522 Ν (%) | TPS > 9 Ν = 189 Ν (%) | Chi Square | p | ||
| Child sex | Female | 341 (50.1) | 31 (50.8) | 0.012 | 0.911 | 268 (51.3) | 87 (46.0) | 1.565 | 0.211 |
| Child age group | >5 years | 364 (53.5) | 37 (60.7) | 1.170 | 0.279 | 272 (52.1) | 117 (61.9) | 5376 | 0.020 |
| Only child | Yes | 150 (22.0) | 19 (31.1) | 2.648 | 0.104 | 107 (20.5) | 54 (28.6) | 5.163 | 0.023 |
| Firstborn | Yes | 342 (50.2) | 45 (73.8) | 12.443 | <0.001 | 255 (48.9) | 116 (61.4) | 8.724 | 0.003 |
| Parent sex | Female | 629 (92.4) | 58 (95.1) | 0.603 | 0.438 | 475 (91.0) | 181 (95.8) | 4.425 | 0.035 |
| Parent age group | <40 years | 496 (72.8) | 52 (85.2) | 4.467 | 0.035 | 370 (70.9) | 153 (81.0) | 7.236 | 0.007 |
| Parental education | Higher | 373 (54.8) | 35 (57.4) | 0.153 | 0.695 | 282 (54.0) | 109 (57.7) | 0.746 | 0.388 |
| Working parent | Yes | 485 (71.2) | 44 (72.1) | 0.023 | 0.880 | 374 (71.6) | 132 (69.8) | 0.221 | 0.639 |
| TFS ≤ 84 Mean ± SD | TFS > 84 Mean ± SD | U test (z) | p | TPS < 9 Mean ± SD | TPS ≥ 9 Mean ± SD | U test (z) | p | ||
| Child age | U = 22,533.0 z = 1.100 | 0.272 | U = 55,351.0 z = 2.490 | 0.013 | |||||
| zBMI | 4.92 ± 0.99 | 4.98 ± 1.09 | U = 13,848.0 z = −3.210 | 0.001 | 4.88 ± 1.00 | 5.07 ± 0.95 | U = 37,233 z = −2.570 | 0.010 | |
| Birth weight | 0.33 ± 1.36 | −0.25 ± 1.76 | U = 23,744.0 z = 1.854 | 0.064 | 0.34 ± 1.36 | 0.07 ± 1.46 | U = 47,928.5 z = −0.579 | 0.563 | |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Sdravou, K.; Fotoulaki, M.; Emmanouilidou-Fotoulaki, E.; Andreoulakis, E.; Makris, G.; Sotiriadou, F.; Printza, A. Feeding Problems in Typically Developing Young Children, a Population-Based Study. Children 2021, 8, 388. https://doi.org/10.3390/children8050388
Sdravou K, Fotoulaki M, Emmanouilidou-Fotoulaki E, Andreoulakis E, Makris G, Sotiriadou F, Printza A. Feeding Problems in Typically Developing Young Children, a Population-Based Study. Children. 2021; 8(5):388. https://doi.org/10.3390/children8050388
Chicago/Turabian StyleSdravou, Katerina, Maria Fotoulaki, Elpida Emmanouilidou-Fotoulaki, Elias Andreoulakis, Giorgos Makris, Fotini Sotiriadou, and Athanasia Printza. 2021. "Feeding Problems in Typically Developing Young Children, a Population-Based Study" Children 8, no. 5: 388. https://doi.org/10.3390/children8050388
APA StyleSdravou, K., Fotoulaki, M., Emmanouilidou-Fotoulaki, E., Andreoulakis, E., Makris, G., Sotiriadou, F., & Printza, A. (2021). Feeding Problems in Typically Developing Young Children, a Population-Based Study. Children, 8(5), 388. https://doi.org/10.3390/children8050388