Health-Related Quality of Life after Adolescent Fractures of the Femoral Shaft Stabilized by a Lateral Entry Femoral Nail
Abstract
:1. Introduction
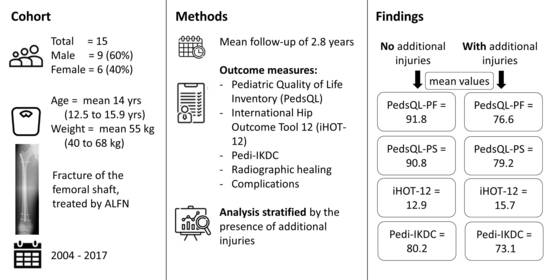
2. Materials and Methods
3. Results
4. Discussion
4.1. Limitations
4.2. Demographics, Radiographic Analysis and Complications
4.3. Health-Related Quality of Life and AO Classification
4.4. HRQoL and Other Injuries
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Conflicts of Interest
References
- Lyons, R.A.; Delahunty, A.M.; Kraus, D.; Heaven, M.; McCabe, M.; Allen, H.; Nash, P. Children’s fractures: A population based study. Inj. Prev. 1999, 5, 129–132. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Bennek, J.; Bühligen, U.; Rothe, K.; Müller, W.; Rolle, U.; Giec, T.; Bennek, C. Fracture treatment in children—data analysis and follow-up results of a prospective study. Injury 2001, 32, 26–29. [Google Scholar] [CrossRef]
- Kelly, B.; Heyworth, B.; Yen, Y.-M.; Hedequist, D. Adverse Sequelae Due to Plate Retention Following Submuscular Plating for Pediatric Femur Fractures. J. Orthop. Trauma 2013, 27, 726–729. [Google Scholar] [CrossRef]
- Moroz, L.A.; Launay, F.; Kocher, M.S.; Newton, P.O.; Frick, S.L.; Sponseller, P.D.; Flynn, J.M. Titanium elastic nailing of fractures of the femur in children. J. Bone Jt. Surgery. Br. Vol. 2006, 88, 1361–1366. [Google Scholar] [CrossRef] [PubMed]
- Weiss, J.M.; Choi, P.; Ghatan, C.; Skaggs, D.L.; Kay, R.M. Complications with flexible nailing of femur fractures more than double with child obesity and weight > 50 kg. J. Child. Orthop. 2009, 3, 53–58. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Canavese, F.; Marengo, L.; Andreacchio, A.; Mansour, M.; Paonessa, M.; Rousset, M.; Samba, A.; Dimeglio, A. Complications of elastic stable intramedullary nailing of femoral shaft fractures in children weighing fifty kilograms (one hundred and ten pounds) and more. Int. Orthop. 2016, 40, 2627–2634. [Google Scholar] [CrossRef]
- Stans, A.A.; Morrissy, R.T.; Renwick, S.E. Femoral shaft fracture treatment in patients age 6 to 16 years. J. Pediatr. Orthop. 1999, 19, 222–228. [Google Scholar] [CrossRef]
- Mileski, R.A.; Garvin, K.L.; Crosby, L.A. Avascular necrosis of the femoral head in an adolescent following intramedullary nailing of the femur. A case report. J. Bone Joint Surg. Am. 1994, 76, 1706–1708. [Google Scholar] [CrossRef]
- O’malley, D.E.; Mazur, J.M.; Cummings, R.J. Femoral Head Avascular Necrosis Associated with Intramedullary Nailing in an Adolescent. J. Pediatr. Orthop. 1995, 15, 21–23. [Google Scholar] [CrossRef]
- Gordon, J.E.; Khanna, N.; Luhmann, S.J.; Dobbs, M.B.; Ortman, M.R.; Schoenecker, P.L. Intramedullary nailing of femoral fractures in children through the lateral aspect of the greater trochanter using a modified rigid humeral intramedullary nail: Preliminary results of a new technique in 15 children. J. Orthop. Trauma 2004, 18, 416–422. [Google Scholar] [CrossRef]
- Keeler, K.A.; Dart, B.; Luhmann, S.J.; Schoenecker, P.L.; Ortman, M.R.; Dobbs, M.B.; Gordon, J.E. Antegrade Intramedullary Nailing of Pediatric Femoral Fractures Using an Interlocking Pediatric Femoral Nail and a Lateral Trochanteric Entry Point. J. Pediatr. Orthop. 2009, 29, 345–351. [Google Scholar] [CrossRef] [PubMed]
- Reynolds, R.A.K.; Legakis, J.E.; Thomas, R.; Slongo, T.F.; Hunter, J.B.; Clavert, J.-M. Intramedullary nails for pediatric diaphyseal femur fractures in older, heavier children: Early results. J. Child. Orthop. 2012, 6, 181–188. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- American Academy of Orthopaedic Surgeons. Treatment of Pediatric Diaphyseal Femur Fractures Evidence-Based Clinical Practice Guideline; American Academy of Orthopaedic Surgeons: Rosemont, IL, USA, 2020. [Google Scholar]
- Rapp, M.; Kraus, R.; Illing, P.; Sommerfeldt, D.W.; Kaiser, M.M. Treatment of femoral shaft fractures in children and adolescents >/=50 kg: A retrospective multicenter trial. Unfallchirurg 2018, 121, 47–57. [Google Scholar] [CrossRef] [PubMed]
- Liebs, T.; Ryser, B.; Kaiser, N.; Slongo, T.; Berger, S.; Ziebarth, K. Health-related Quality of Life After Fractures of the Lateral Third of the Clavicle in Children and Adolescents. J. Pediatr. Orthop. 2019, 39, e542–e547. [Google Scholar] [CrossRef] [PubMed]
- Liebs, T.R.; Burgard, M.; Kaiser, N.; Slongo, T.; Berger, S.; Ryser, B.; Ziebarth, K. Health-related quality of life after paediatric supracondylar humeral fractures. Bone Jt. J. 2020, 102-B, 755–765. [Google Scholar] [CrossRef] [PubMed]
- Liebs, T.R.; Rompen, I.; Berger, S.M.; Ziebarth, K. Health-related quality of life after conservatively and surgically-treated paediatric proximal humeral fractures. J. Child. Orthop. 2021, 15, 204–214. [Google Scholar] [CrossRef]
- Slongo, T.; Audige, L. AO Paediatric Classification Group. Distal metaphyseal fractures (13-M). In AO Pediatric Comprehensive Classification of Long-Bone Fractures (PCCF); Slongo, T., Audige, L., AO Paediatric Classification Group, Eds.; AO Foundation: Davos, Switzerland, 2007; p. 15. [Google Scholar]
- Winquist, R.A.; Hansen, S.T., Jr.; Clawson, D.K. Closed intramedullary nailing of femoral fractures. A report of five hundred and twenty cases. J. Bone Joint Surg. Am. 1984, 66, 529–539. [Google Scholar] [CrossRef]
- Baumann, F.; Popp, D.; Müller, K.; Müller, M.; Schmitz, P.; Nerlich, M.; Fickert, S. Validation of a German version of the International Hip Outcome Tool 12 (iHOT12) according to the COSMIN checklist. Heallth Qual. Life Outcomes 2016, 14, 52. [Google Scholar] [CrossRef] [Green Version]
- d’Entremont, A.G.; Cooper, A.P.; Johari, A.; Mulpuri, K. What clinimetric evidence exists for using hip-specific patient-reported outcome measures in pediatric hip impingement? Clin. Orthop. Relat. Res. 2015, 473, 1361–1367. [Google Scholar] [CrossRef] [Green Version]
- Kocher, M.S.; Smith, J.T.; Iversen, M.D.; Brustowicz, K.; Ogunwole, O.; Andersen, J.; Yoo, W.J.; Mcfeely, E.D.; Anderson, A.F.; Zurakowski, D. Reliability, Validity, and Responsiveness of a Modified International Knee Documentation Committee Subjective Knee Form (Pedi-IKDC) in Children with Knee Disorders. Am. J. Sports Med. 2010, 39, 933–939. [Google Scholar] [CrossRef]
- Nasreddine, A.Y.; Connell, P.L.; Kalish, L.A.; Nelson, S.; Iversen, M.D.; Anderson, A.F.; Kocher, M.S. The Pediatric International Knee Documentation Committee (Pedi-IKDC) Subjective Knee Evaluation Form: Normative Data. Am. J. Sports Med. 2017, 45, 527–534. [Google Scholar] [CrossRef] [PubMed]
- van der Velden, C.A.; van der Steen, M.C.; Leenders, J.; van Douveren, F.Q.M.P.; Janssen, R.P.A.; Reijman, M. Pedi-IKDC or KOOS-child: Which questionnaire should be used in children with knee disorders? BMC Musculoskelet. Disord. 2019, 20, 240. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Mahan, S.T.; Kalish, L.A.; Connell, P.L.; Harris, M.; Abdul-Rahim, Z.; Waters, P. PedsQL Correlates to PODCI in Pediatric Orthopaedic Outpatient Clinic. J. Pediatr. Orthop. 2014, 34, e22–e26. [Google Scholar] [CrossRef] [PubMed]
- Ackerman, I.N.; Dieppe, P.A.; March, L.M.; Roos, E.M.; Nilsdotter, A.K.; Brown, G.C.; Sloan, K.E.; Osborne, R.H. Variation in age and physical status prior to total knee and hip replacement surgery: A comparison of centers in Australia and Europe. Arthritis Care Res. 2009, 61, 166–173. [Google Scholar] [CrossRef] [PubMed]
- Gordon, J.E.; Mehlman, C.T. The Community Orthopaedic Surgeon Taking Trauma Call: Pediatric Femoral Shaft Fracture Pearls and Pitfalls. J. Orthop. Trauma 2017, 31, S16–S21. [Google Scholar] [CrossRef]
- Winthrop, A.L.; Brasel, K.J.; Stahovic, L.; Paulson, J.; Schneeberger, B.; Kuhn, E.M. Quality of life and functional outcome after pediatric trauma. J. Trauma 2005, 58, 468–473. [Google Scholar] [CrossRef]




| Additional Injury | |||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| No Additional Injury | With Additional Injury | Total | |||||||||||||||||
| n | Column N % | Mean | SD | Min | Max | n | Column N % | Mean | SD | Min | Max | n | Column N % | Mean | SD | Min | Max | ||
| Gender | |||||||||||||||||||
| female | 3 | 33% | 3 | 50% | 6 | 40% | |||||||||||||
| male | 6 | 67% | 3 | 50% | 9 | 60% | |||||||||||||
| Age at the time of injury [years] | 9 | 13.8 | 1.0 | 12.5 | 15.6 | 6 | 14.2 | 1.0 | 13.1 | 15.9 | 15 | 14.0 | 1.0 | 12.5 | 15.9 | ||||
| Weight [kg] at time of the injury | 9 | 52 | 6 | 40 | 60 | 6 | 59 | 6 | 50 | 68 | 15 | 55 | 7 | 40 | 68 | ||||
| Height [cm] at time of the injury | 9 | 164 | 10 | 153 | 178 | 6 | 166 | 5 | 160 | 171 | 15 | 165 | 8 | 153 | 178 | ||||
| BMI [kg/m2] at time of the injury | 9 | 19.1 | 2.0 | 17.1 | 23.3 | 6 | 21.7 | 2.2 | 19.5 | 25.9 | 15 | 20.2 | 2.4 | 17.1 | 25.9 | ||||
| Injured side (right vs. left) | |||||||||||||||||||
| right | 4 | 44% | 3 | 50% | 7 | 47% | |||||||||||||
| left | 5 | 56% | 2 | 33% | 7 | 47% | |||||||||||||
| bilateral | 1 | 17% | 1 | 7% | |||||||||||||||
| Radiological classification according to the AO | |||||||||||||||||||
| 32-D/4.1 | 3 | 33% | 1 | 17% | 4 | 27% | |||||||||||||
| 32-D/5.1 | 5 | 56% | 3 | 50% | 8 | 53% | |||||||||||||
| 32-D/5.2 | 1 | 11% | 2 | 33% | 3 | 20% | |||||||||||||
| Winquist and Hansen classification regarding the degree of comminution | |||||||||||||||||||
| 0: Transverse or short oblique fractures with no comminution | 4 | 44% | 1 | 17% | 5 | 33% | |||||||||||||
| 1: Small butterfly fragment of less than 25% of width of the bone | 3 | 33% | 2 | 33% | 5 | 33% | |||||||||||||
| 2: Butterfly fragment of 50% or less of the width of the bone | 2 | 33% | 2 | 13% | |||||||||||||||
| 3: Large butterfly fragment greater than 50% of the width of bone | 1 | 11% | 1 | 7% | |||||||||||||||
| 4: Segmental comminution | 1 | 11% | 1 | 17% | 2 | 13% | |||||||||||||
| ALFN as the primary treatment or as a revision | |||||||||||||||||||
| ALFN used for revision of otherwise failed fixation | 1 | 11% | 1 | 17% | 2 | 13% | |||||||||||||
| ALFN used as primary fixation | 8 | 89% | 5 | 83% | 13 | 87% | |||||||||||||
| Injury mechanism | |||||||||||||||||||
| motor vehicle accident | 2 | 22% | 6 | 100% | 8 | 53% | |||||||||||||
| sports | 4 | 44% | 4 | 27% | |||||||||||||||
| fall from tree/play | 3 | 33% | 3 | 20% | |||||||||||||||
| Was the skin injured at the time of the injury? | |||||||||||||||||||
| No, skin was intact | 9 | 100% | 5 | 83% | 14 | 93% | |||||||||||||
| Yes, but was just a scratch | |||||||||||||||||||
| Yes, a suture was necessary | 1 | 17% | 1 | 7% | |||||||||||||||
| Additional Injury | |||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| No Additional Injury | With Additional Injury | Total | |||||||||||||||||
| Mean | SD | Min | Max | Count | Column N % | Mean | SD | Min | Max | Count | Column N % | Mean | SD | Min | Max | Count | Column N % | ||
| Follow-up duration [years] | 2.94 | 2.91 | 0.45 | 7.16 | 9 | 2.55 | 2.29 | 0.29 | 5.63 | 6 | 2.79 | 2.6 | 0.29 | 7.16 | 15 | ||||
| iHOT-12 (0–100) | 12.9 | 14.8 | 9 | 15.7 | 17.4 | 6 | 14 | 15.4 | 15 | ||||||||||
| IKDC | 80.2 | 7.54 | 9 | 73.1 | 14.8 | 6 | 77.2 | 11.3 | 15 | ||||||||||
| PedsQL physical function | 91.8 | 9.02 | 9 | 76.6 | 27.2 | 6 | 85.7 | 19.3 | 15 | ||||||||||
| PedsQL social function | 90.8 | 7.72 | 9 | 79.2 | 15.7 | 6 | 86.2 | 12.5 | 15 | ||||||||||
| Are you satisfied with the thigh that was injured? | |||||||||||||||||||
| Very satisfied | 5 | 56% | 4 | 67% | 9 | 60% | |||||||||||||
| A little satisfied | 3 | 33% | 2 | 33% | 5 | 33% | |||||||||||||
| A little unsatisfied | 1 | 11% | 1 | 7% | |||||||||||||||
| Very unsatisfied | |||||||||||||||||||
| Are you satisfied with the treatment that was performed? | |||||||||||||||||||
| Very satisfied | 5 | 71% | 3 | 75% | 8 | 73% | |||||||||||||
| A little satisfied | 2 | 29% | 1 | 25% | 3 | 27% | |||||||||||||
| A little unsatisfied | |||||||||||||||||||
| Very unsatisfied | |||||||||||||||||||
| Now you know the treatment and the results. If you could turn back time, would you choose this treatment again? | |||||||||||||||||||
| Yes, definitely | 5 | 71% | 3 | 75% | 8 | 73% | |||||||||||||
| Yes, probably | 2 | 29% | 1 | 25% | 3 | 27% | |||||||||||||
| No, probably not | |||||||||||||||||||
| No, not at all | |||||||||||||||||||
| How would you describe the pain that you typically experience in your thigh? | |||||||||||||||||||
| No pain | 2 | 22% | 5 | 83% | 7 | 47% | |||||||||||||
| Little pain | 6 | 67% | 6 | 40% | |||||||||||||||
| Moderate pain | 1 | 11% | 1 | 17% | 2 | 13% | |||||||||||||
| Strong pain | |||||||||||||||||||
| When does the pain typically occur? | |||||||||||||||||||
| I do not have any pain | 4 | 44% | 4 | 67% | 8 | 53% | |||||||||||||
| Only for the first steps | 1 | 11% | 1 | 17% | 2 | 13% | |||||||||||||
| Only after longer walks (30 min) | 4 | 44% | 1 | 17% | 5 | 33% | |||||||||||||
| When walking | |||||||||||||||||||
| Constant pain | |||||||||||||||||||
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Liebs, T.R.; Meßling, A.; Milosevic, M.; Berger, S.M.; Ziebarth, K. Health-Related Quality of Life after Adolescent Fractures of the Femoral Shaft Stabilized by a Lateral Entry Femoral Nail. Children 2022, 9, 327. https://doi.org/10.3390/children9030327
Liebs TR, Meßling A, Milosevic M, Berger SM, Ziebarth K. Health-Related Quality of Life after Adolescent Fractures of the Femoral Shaft Stabilized by a Lateral Entry Femoral Nail. Children. 2022; 9(3):327. https://doi.org/10.3390/children9030327
Chicago/Turabian StyleLiebs, Thoralf Randolph, Anna Meßling, Milan Milosevic, Steffen Michael Berger, and Kai Ziebarth. 2022. "Health-Related Quality of Life after Adolescent Fractures of the Femoral Shaft Stabilized by a Lateral Entry Femoral Nail" Children 9, no. 3: 327. https://doi.org/10.3390/children9030327
APA StyleLiebs, T. R., Meßling, A., Milosevic, M., Berger, S. M., & Ziebarth, K. (2022). Health-Related Quality of Life after Adolescent Fractures of the Femoral Shaft Stabilized by a Lateral Entry Femoral Nail. Children, 9(3), 327. https://doi.org/10.3390/children9030327