Effect of Indian Music as an Auditory Stimulus on Physiological Measures of Stress, Anxiety, Cardiovascular and Autonomic Responses in Humans—A Randomized Controlled Trial
Abstract
:1. Introduction
2. Materials and Methods
2.1. Study Design
2.2. Ethical Approvals
2.3. The Basis for Sample Size
2.4. Recruitment
2.5. Inclusion and Exclusion Criteria
2.6. Baseline Demographic Data Recording
2.7. Randomization
2.8. Interventions
2.8.1. Music Intervention
2.8.2. Control Group Intervention
2.9. First Visit to the Lab
2.10. Second Visit to the Lab
2.11. Behavioral Measures
Measurement of Anxiety
2.12. Physiological Parameters
Saliva for Biomarkers of Stress
2.13. Cardiovascular Parameters
2.13.1. Blood Pressure (BP) and Heart Rate (HR)
2.13.2. Electrocardiogram Recording and Heart Rate Variability Analysis
2.14. Statistical Analysis
3. Results
3.1. Sociodemographic Data
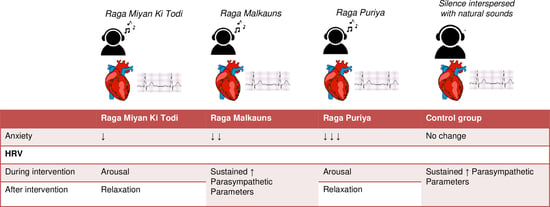
3.2. Behavioral Analysis
STAI
3.3. Physiological Parameters
Biomarkers of Stress
3.4. Cardiovascular Parameters
3.4.1. Blood Pressure and Heart Rate
3.4.2. Heart Rate Variability
Time-Domain Parameters of Heart Rate Variability
Frequency-Domain Parameters of Heart Rate Variability
4. Discussion
4.1. Behavioral Analysis
Anxiety
4.2. Biomarkers of Stress
4.3. Cardiovascular Parameters
4.3.1. Blood Pressure
4.3.2. Heart Rate Variability
4.4. Future Directions
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Schäfer, T.; Tipandjan, A.; Sedlmeier, P. The functions of music and their relationship to music preference in India and Germany. Int. J. Psychol. 2012, 47, 370–380. [Google Scholar] [CrossRef] [PubMed]
- Montinari, M.R.; Giardina, S.; Minelli, P.; Minelli, S. History of Music Therapy and Its Contemporary Applications in Cardiovascular Diseases. South. Med. J. 2018, 111, 98–102. [Google Scholar] [CrossRef] [PubMed]
- Definition and Quotes about Music Therapy | Definition and Quotes about Music Therapy | American Music Therapy Association (AMTA). Available online: https://www.musictherapy.org/ (accessed on 15 May 2019).
- McCrary, J.M.; Redding, E.; Altenmüller, E. Performing arts as a health resource? An umbrella review of the health impacts of music and dance participation. PLoS ONE 2021, 16, e0252956. [Google Scholar] [CrossRef] [PubMed]
- Fancourt, D.; Finn, S. What Is the Evidence on the Role of the Arts in Improving Health and Well-Being. A Scoping Review; World Health Organization Regional Office for Europe: Copenhagen, Denmark, 2019. Available online: https://www.ncbi.nlm.nih.gov/books/NBK553773/ (accessed on 9 August 2022).
- Reybrouck, M.; Vuust, P.; Brattico, E. Neural Correlates of Music Listening: Does the Music Matter? Brain Sci. 2021, 11, 1553. [Google Scholar] [CrossRef] [PubMed]
- Engel, A.; Hoefle, S.; Monteiro, M.C.; Moll, J.; Keller, P.E. Neural Correlates of Listening to Varying Synchrony Between Beats in Samba Percussion and Relations to Feeling the Groove. Front. Neurosci. 2022, 16, 779964. Available online: https://www.frontiersin.org/articles/10.3389/fnins.2022.779964 (accessed on 9 August 2022). [CrossRef] [PubMed]
- Biagini, M.S.; Brown, L.E.; Coburn, J.W.; Judelson, D.A.; Statler, T.A.; Bottaro, M.; Tran, T.T.; Longo, N.A. Effects of Self-Selected Music on Strength, Explosiveness, and Mood. J. Strength Cond. Res. 2012, 26, 1934–1938. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Vinciguerra, C.; De Stefano, N.; Federico, A. Exploring the role of music therapy in multiple sclerosis: Brief updates from research to clinical practice. Neurol. Sci. 2019, 40, 2277–2285. [Google Scholar] [CrossRef]
- Nardone, V.; Vinciguerra, C.; Correale, P.; Guida, C.; Tini, P.; Reginelli, A.; Cappabianca, S. Music therapy and radiation oncology: State of art and future directions. Complement. Ther. Clin. Pract. 2020, 39, 101124. [Google Scholar] [CrossRef]
- Linnemann, A.; Wenzel, M.; Grammes, J.; Kubiak, T.; Nater, U.M. Music Listening and Stress in Daily Life—A Matter of Timing. Int. J. Behav. Med. 2018, 25, 223–230. [Google Scholar] [CrossRef] [Green Version]
- Thoma, M.V.; La Marca, R.; Brönnimann, R.; Finkel, L.; Ehlert, U.; Nater, U.M. The Effect of Music on the Human Stress Response. PLoS ONE 2013, 8, e70156. [Google Scholar] [CrossRef]
- Linnemann, A.; Strahler, J.; Nater, U.M. The stress-reducing effect of music listening varies depending on the social context. Psychoneuroendocrinology 2016, 72, 97–105. [Google Scholar] [CrossRef]
- Linnemann, A.; Strahler, J.; Nater, U.M. Assessing the Effects of Music Listening on Psychobiological Stress in Daily Life. J. Vis. Exp. 2017, 120, 54920. [Google Scholar] [CrossRef]
- Labbe, E.; Schmidt, N.; Babin, J.; Pharr, M. Coping with Stress: The Effectiveness of Different Types of Music. Appl. Psychophysiol. Biofeedback 2007, 32, 163–168. [Google Scholar] [CrossRef]
- Alagha, J.; Ipradjian, A. The Effects of Different Types of Music on Stress Levels. Glob. J. Hum.-Soc. Sci. A Arts Humanit.—Psychol. 2017, 17, 5. [Google Scholar]
- De Witte, M.; Spruit, A.; Van Hooren, S.; Moonen, X.; Stams, G.-J. Effects of music interventions on stress-related outcomes: A systematic review and two meta-analyses. Health Psychol. Rev. 2020, 14, 294–324. [Google Scholar] [CrossRef]
- Wuttke-Linnemann, A.; Nater, U.M.; Ehlert, U.; Ditzen, B. Sex-specific Effects of Music Listening on Couples’ Stress in Everyday Life. Sci. Rep. 2019, 9, 4880. [Google Scholar] [CrossRef] [Green Version]
- Pezzin, L.E.; Larson, E.R.; Lorber, W.; McGinley, E.L.; Dillingham, T.R. Music-instruction intervention for treatment of post-traumatic stress disorder: A randomized pilot study. BMC Psychol. 2018, 6, 60. [Google Scholar] [CrossRef]
- Hegde, S. Music therapy for mental disorder and mental health: The untapped potential of Indian classical music. BJPsych. Int. 2017, 14, 31–33. [Google Scholar] [CrossRef] [Green Version]
- Knobloch, S.; Zillmann, D. Mood Management via the Digital Jukebox. J. Commun. 2002, 52, 351–366. [Google Scholar] [CrossRef]
- Ubrangala, K.K.; Kunnavil, R.; Goturu, J.; Vijayadas, M.; Prakash, V.S.; Murthy, N.S. Effect of specific melodic scales of Indian music in reducing state and trait anxiety: A randomized clinical trial. Psychol. Music 2021, 50, 1390–1407. [Google Scholar] [CrossRef]
- Kunikullaya, K.U.; Goturu, J.; Muradi, V.; Hukkeri, P.A.; Kunnavil, R.; Doreswamy, V.; Prakash, V.S.; Murthy, N.S. Combination of music with lifestyle modification versus lifestyle modification alone on blood pressure reduction—A randomized controlled trial. Complement. Ther. Clin. Pract. 2016, 23, 102–109. [Google Scholar] [CrossRef]
- Lu, G.; Jia, R.; Liang, D.; Yu, J.; Wu, Z.; Chen, C. Effects of music therapy on anxiety: A meta-analysis of randomized controlled trials. Psychiatry Res. 2021, 304, 114137. [Google Scholar] [CrossRef]
- Kühlmann, A.Y.R.; de Rooij, A.; Kroese, L.F.; van Dijk, M.; Hunink, M.G.M.; Jeekel, J. Meta-analysis evaluating music interventions for anxiety and pain in surgery. Br. J. Surg. 2018, 105, 773–783. [Google Scholar] [CrossRef] [Green Version]
- Van Willenswaard, K.C.; Lynn, F.; McNeill, J.; McQueen, K.; Dennis, C.-L.; Lobel, M.; Alderdice, F. Music interventions to reduce stress and anxiety in pregnancy: A systematic review and meta-analysis. BMC Psychiatry 2017, 17, 271. [Google Scholar] [CrossRef] [Green Version]
- Márquez-Celedonio, F.G.; Téxon-Fernández, O.; Chávez-Negrete, A.; Hernández-López, S.; Marín-Rendónm, S.; Berlín-Lascurain, S. Clinical effect of lifestyle modification on cardiovascular risk in prehypertensives: PREHIPER I study. Rev. Esp. Cardiol. 2009, 62, 86–90. [Google Scholar] [CrossRef]
- Bekiroğlu, T.; Ovayolu, N.; Ergün, Y.; Ekerbiçer, H. Effect of Turkish classical music on blood pressure: A randomized controlled trial in hypertensive elderly patients. Complement. Ther. Med. 2013, 21, 147–154. [Google Scholar] [CrossRef]
- Loomba, R.S.; Arora, R.; Shah, P.H.; Chandrasekar, S.; Molnar, J. Effects of music on systolic blood pressure, diastolic blood pressure, and heart rate: A meta-analysis. Indian Heart J. 2012, 64, 309–313. [Google Scholar] [CrossRef] [Green Version]
- Im-Oun, S.; Kotruchin, P.; Thinsug, P.; Mitsungnern, T.; Techa-Atik, P.; Pongchaiyakul, C. Effect of Thai instrumental folk music on blood pressure: A randomized controlled trial in stage-2 hypertensive patients. Complement. Ther. Med. 2018, 39, 43–48. [Google Scholar] [CrossRef]
- Amaral, M.A.S.D.; Neto, M.G.; de Queiroz, J.G.; Martins-Filho, P.R.S.; Saquetto, M.B.; Carvalho, V.O. Effect of music therapy on blood pressure of individuals with hypertension: A systematic review and Meta-analysis. Int. J. Cardiol. 2016, 214, 461–464. [Google Scholar] [CrossRef]
- Salmore, R.G.; Nelson, J.P. The effect of preprocedure teaching, relaxation instruction, and music on anxiety as measured by blood pressures in an outpatient gastrointestinal endoscopy laboratory. Gastroenterol. Nurs. 2000, 23, 102–110. [Google Scholar] [CrossRef]
- Smolen, D.; Topp, R.; Singer, L. The effect of self-selected music during colonoscopy on anxiety, heart rate, and blood pressure. Appl. Nurs. Res. 2002, 15, 126–136. [Google Scholar] [CrossRef]
- Dileo, C. Effects of music and music therapy on medical patients: A meta-analysis of the research and implications for the future. J. Soc. Integr. Oncol. 2006, 4, 67–70. [Google Scholar] [CrossRef] [PubMed]
- Cadigan, M.E.; Caruso, N.A.; Haldeman, S.M.; McNamara, M.E.; Noyes, D.A.; Spadafora, M.A.; Carroll, D.L. The Effects of Music on Cardiac Patients on Bed Rest. Prog. Cardiovasc. Nurs. 2001, 16, 5–13. [Google Scholar] [CrossRef] [PubMed]
- Berbel, P.; Moix, J.; Quintana, S. Music versus diazepam to reduce preoperative anxiety: A randomized controlled clinical trial. Rev. Esp. Anestesiol. Reanim. 2007, 54, 355–358. [Google Scholar] [PubMed]
- Kunikullaya, U.K.; Kunnavil, R.; Vijayadas; Goturu, J.; Prakash, V.S.; Murthy, N.S. Normative data and gender differences in heart rate variability in the healthy young individuals aged 18–30 years, a South Indian cross-sectional study. Indian Pacing Electrophysiol. J. 2021, 21, 112–119. [Google Scholar] [CrossRef] [PubMed]
- Kunikullaya, K.U.; Goturu, J.; Muradi, V.; Hukkeri, P.A.; Kunnavil, R.; Doreswamy, V.; Prakash, V.S.; Murthy, N.S. Music versus lifestyle on the autonomic nervous system of prehypertensives and hypertensives—A randomized control trial. Complement. Ther. Med. 2015, 23, 733–740. [Google Scholar] [CrossRef] [PubMed]
- Hamel, W.J. The effects of music intervention on anxiety in the patient waiting for cardiac catheterization. Intensive Crit. Care Nurs. 2001, 17, 279–285. [Google Scholar] [CrossRef] [PubMed]
- Bernardi, L.; Porta, C.; Sleight, P. Cardiovascular, cerebrovascular, and respiratory changes induced by different types of music in musicians and non-musicians: The importance of silence. Heart 2006, 92, 445–452. [Google Scholar] [CrossRef] [Green Version]
- Larsen, P.D. The sound of silence is music to the heart. Heart 2006, 92, 433–434. [Google Scholar] [CrossRef] [Green Version]
- Okada, K.; Kurita, A.; Takase, B.; Otsuka, T.; Kodani, E.; Kusama, Y.; Atarashi, H.; Mizuno, K. Effects of music therapy on autonomic nervous system activity, incidence of heart failure events, and plasma cytokine and catecholamine levels in elderly patients with cerebrovascular disease and dementia. Int. Heart J. 2009, 50, 95–110. [Google Scholar] [CrossRef] [Green Version]
- Yamamoto, T.; Ohkuwa, T.; Itoh, H.; Kitoh, M.; Terasawa, J.; Tsuda, T.; Kitagawa, S.; Sato, Y. Effects of Pre-exercise Listening to Slow and Fast Rhythm Music on Supramaximal Cycle Performance and Selected Metabolic Variables. Arch. Physiol. Biochem. 2003, 111, 211–214. [Google Scholar] [CrossRef]
- Urakawa, K.; Yokoyama, K. Music Can Enhance Exercise-Induced Sympathetic Dominancy Assessed by Heart Rate Variability. Tohoku J. Exp. Med. 2005, 206, 213–218. [Google Scholar] [CrossRef] [Green Version]
- Dey, A.; Bhattacharya, D.K.; Tibarewala, D.N.; Palit, S.K. Effect of Music on Autonomic Nervous System through the Study of Symbolic Dynamics of Heart Rate Variability Signals. J. Proc. 2013, 3, 120–124. Available online: http://journals.theired.org/journals/paper/details/1649.html (accessed on 30 January 2019).
- Shimomura, Y.; Hoshiba, K.; Morigiwa, T.; Matsumoto, K. Psychophysiological study of music stimuli on music therapy. J. Jpn. Biomusic. Assoc. 1997, 15, 121–128. [Google Scholar]
- Linnemann, A.; Ditzen, B.; Strahler, J.; Doerr, J.M.; Nater, U.M. Music listening as a means of stress reduction in daily life. Psychoneuroendocrinology 2015, 60, 82–90. [Google Scholar] [CrossRef]
- Lieber, A.C.; Bose, J.; Zhang, X.; Seltzberg, H.; Loewy, J.; Rossetti, A.; Mocco, J.; Kellner, C.P. Effects of music therapy on anxiety and physiologic parameters in angiography: A systematic review and meta-analysis. J. Neurointerv. Surg. 2019, 11, 416–423. [Google Scholar] [CrossRef]
- Panteleeva, Y.; Ceschi, G.; Glowinski, D.; Courvoisier, D.S.; Grandjean, D. Music for anxiety? Meta-analysis of anxiety reduction in non-clinical samples. Psychol. Music 2018, 46, 473–487. [Google Scholar] [CrossRef] [Green Version]
- Mojtabavi, H.; Saghazadeh, A.; Valenti, V.E.; Rezaei, N. Can music influence cardiac autonomic system? A systematic review and narrative synthesis to evaluate its impact on heart rate variability. Complement. Ther. Clin. Pract. 2020, 39, 101162. [Google Scholar] [CrossRef]
- Kühlmann, A.Y.R.; Etnel, J.R.G.; Roos-Hesselink, J.W.; Jeekel, J.; Bogers, A.J.J.C.; Takkenberg, J.J.M. Systematic review and meta-analysis of music interventions in hypertension treatment: A quest for answers. BMC Cardiovasc. Disord. 2016, 16, 69. [Google Scholar] [CrossRef] [Green Version]
- Mathur, A.; Vijayakumar, S.H.; Chakrabarti, B.; Singh, N.C. Emotional responses to Hindustani raga music: The role of musical structure. Front. Psychol. 2015, 6, 513. [Google Scholar] [CrossRef] [Green Version]
- Midya, V.; Valla, J.; Balasubramanian, H.; Mathur, A.; Singh, N.C. Cultural differences in the use of acoustic cues for musical emotion experience. PLoS ONE 2019, 14, e0222380. [Google Scholar] [CrossRef]
- Bowling, D.L.; Sundararajan, J.; Han, S.; Purves, D. Expression of Emotion in Eastern and Western Music Mirrors Vocalization. PLoS ONE 2012, 7, e31942. [Google Scholar] [CrossRef]
- Balkwill, L.-L.; Thompson, W. A Cross-Cultural Investigation of the Perception of Emotion in Music: Psychophysical and Cultural Cues. Music Percept. 1999, 17, 43–64. [Google Scholar] [CrossRef]
- Mukherjee, S.; Palit, S.K.; Banerjee, S.; Bhattacharya, D.K. A Comparative Study on Three Different Types of Music Based on Same Indian Raga and Their Effects on Human Autonomic Nervous Systems. In Chaos, Complexity and Leadership 2013; Springer: Cham, Switzerland, 2015; pp. 243–254. Available online: https://link.springer.com/chapter/10.1007/978-3-319-09710-7_21 (accessed on 30 April 2019).
- Osmer, B. ‘Raga Chikitsa and Raga Ragini Vidya—Bill Osmer’, December 2006. pp. 1–29. Available online: https://swaraabhimanee.files.wordpress.com/2016/11/raga-ragani-vidya.pdf (accessed on 17 October 2018).
- Jairazbhoy, N.A. The Rāgs of North Indian Music: Their Structure and Evolution; Popular Prakashan: Mumbai, India, 1995. [Google Scholar]
- ITC Sangeet Research Academy. Available online: https://www.itcsra.org/cronology600 (accessed on 29 March 2019).
- Kaufmann, W. Rasa, Raga-Mala and Performance Times in North Indian Ragas. Ethnomusicology 1965, 9, 272–291. [Google Scholar] [CrossRef]
- McNeil, A. Ragas, Recipes, and Rasas, Oxford Handbooks Online, 7 April 2015. Available online: https://www.oxfordhandbooks.com/view/10.1093/oxfordhb/9780199935321.001.0001/oxfordhb-9780199935321-e-43 (accessed on 29 April 2020).
- WMA—The World Medical Association-WMA Declaration of Helsinki—Ethical Principles for Medical Research Involving Human Subjects. Available online: https://www.wma.net/policies-post/wma-declaration-of-helsinki-ethical-principles-for-medical-research-involving-human-subjects/ (accessed on 9 August 2022).
- Graff, V.; Cai, L.; Badiola, I.; Elkassabany, N.M. Music versus midazolam during preoperative nerve block placements: A prospective randomized controlled study. Reg. Anesth. Pain Med. 2019, 44, 796–799. [Google Scholar] [CrossRef] [PubMed]
- Idrobo-Ávila, E.H.; Loaiza-Correa, H.; Van Noorden, L.; Muñoz-Bolaños, F.G.; Vargas-Canas, R. Different Types of Sounds and Their Relationship with the Electrocardiographic Signals and the Cardiovascular System—Review. Front. Physiol. 2018, 9, 525. [Google Scholar] [CrossRef] [PubMed]
- McNeil, A. Seed ideas and creativity in Hindustani raga music: Beyond the composition–improvisation dialectic. Ethnomusicol. Forum 2017, 26, 116–132. [Google Scholar] [CrossRef]
- Bansuri, Wikipedia. 30 March 2018. Available online: https://en.wikipedia.org/w/index.php?title=Bansuri&oldid=833200245 (accessed on 13 June 2018).
- Watanabe, K.; Ooishi, Y.; Kashino, M. Heart rate responses induced by acoustic tempo and its interaction with basal heart rate. Sci. Rep. 2017, 7, 43856. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Liu, Y.; Liu, G.; Wei, D.; Li, Q.; Yuan, G.; Wu, S.; Wang, G.; Zhao, X. Effects of Musical Tempo on Musicians’ and Non-musicians’ Emotional Experience When Listening to Music. Front. Psychol. 2018, 9, 2118. [Google Scholar] [CrossRef]
- Levitin, D.J.; Grahn, J.A.; London, J. The Psychology of Music: Rhythm and Movement. Annu. Rev. Psychol. 2018, 69, 51–75. [Google Scholar] [CrossRef] [Green Version]
- Zhao, T.C.; Lam, H.G.; Sohi, H.; Kuhl, P.K. Neural processing of musical meter in musicians and non-musicians. Neuropsychologia 2017, 106, 289–297. [Google Scholar] [CrossRef]
- Stith, C.C. The Effects of Musical Tempo and Dynamic Range on Heart Rate Variability in Healthy Adults: A Counterbalanced, Within-subjects Study. Ph.D. Thesis, Appalachian State University, Boone, NC, USA, May 2015. [Google Scholar]
- Patel, A.D.; Iversen, J. The evolutionary neuroscience of musical beat perception: The Action Simulation for Auditory Prediction (ASAP) hypothesis. Front. Syst. Neurosci. 2014, 8, 57. [Google Scholar] [CrossRef]
- Daly, I.; Hallowell, J.; Hwang, F.; Kirke, A.; Malik, A.; Roesch, E.; Weaver, J.; Williams, D.; Miranda, E.; Nasuto, S.J. Changes in music tempo entrain movement related brain activity. In Proceedings of the 2014 36th Annual International Conference of the IEEE Engineering in Medicine and Biology Society, Chicago, IL, USA, 26–30 August 2014; Volume 2014, pp. 4595–4598. [Google Scholar] [CrossRef]
- Schaub, K.; Demos, L.; Centeno, T.; Daugherty, B. Effects of Musical Tempo on Heart Rate, Brain Activity, and Short-term Memory. J. Adv. Stud. Sci. 2011, 1, 11. Available online: http://jass.neuro.wisc.edu/2011/01/ (accessed on 16 October 2022).
- State-Trait Anxiety Inventory for Adults (STAI-AD)-Assessments, Tests | Mind Garden-Mind Garden. Available online: https://www.mindgarden.com/145-state-trait-anxiety-inventory-for-adults (accessed on 28 November 2018).
- Julian, L.J. Measures of anxiety: State-Trait Anxiety Inventory (STAI), Beck Anxiety Inventory (BAI), and Hospital Anxiety and Depression Scale-Anxiety (HADS-A). Arthritis Care Res. 2011, 63, S467–S472. [Google Scholar] [CrossRef] [Green Version]
- Grös, D.F.; Antony, M.M.; Simms, L.J.; McCabe, R.E. Psychometric properties of the State-Trait Inventory for Cognitive and Somatic Anxiety (STICSA): Comparison to the State-Trait Anxiety Inventory (STAI). Psychol. Assess. 2007, 19, 369–381. [Google Scholar] [CrossRef] [Green Version]
- Riquelme, A.G.; Buela-Casal, G. Meta-analysis of group comparison and meta-analysis of reliability generalization of the State-Trait Anxiety Inventory Questionnaire (STAI). Rev. Española Salud Pública 2014, 88, 101–112. [Google Scholar] [CrossRef]
- Petrakova, L.; Doering, B.K.; Vits, S.; Engler, H.; Rief, W.; Schedlowski, M.; Grigoleit, J.-S. Psychosocial Stress Increases Salivary Alpha-Amylase Activity Independently from Plasma Noradrenaline Levels. PLoS ONE 2015, 10, e0134561. [Google Scholar] [CrossRef] [Green Version]
- Nater, U.M.; Abbruzzese, E.; Krebs, M.; Ehlert, U. Sex differences in emotional and psychophysiological responses to musical stimuli. Int. J. Psychophysiol. 2006, 62, 300–308. [Google Scholar] [CrossRef]
- Skosnik, P.D.; Chatterton, R.T.; Swisher, T.; Park, S. Modulation of attentional inhibition by norepinephrine and cortisol after psychological stress. Int. J. Psychophysiol. 2000, 36, 59–68. [Google Scholar] [CrossRef]
- Takahashi, H.; Yoshika, M.; Yokoi, T. Validation of three automatic devices for the self-measurement of blood pressure according to the European Society of Hypertension International Protocol revision 2010: The Omron HEM-7130, HEM-7320F, and HEM-7500F. Blood Press. Monit. 2015, 20, 92–97. [Google Scholar] [CrossRef]
- Peretz, I.; Zatorre, R.J. Brain Organization for Music Processing. Annu. Rev. Psychol. 2005, 56, 89–114. [Google Scholar] [CrossRef] [Green Version]
- Ventura, T.; Gomes, M.; Carreira, T. Cortisol and anxiety response to a relaxing intervention on pregnant women awaiting amniocentesis. Psychoneuroendocrinology 2012, 37, 148–156. [Google Scholar] [CrossRef] [PubMed]
- Wang, S.-M.; Kulkarni, L.; Dolev, J.; Kain, Z.N. Music and preoperative anxiety: A randomized, controlled study. Anesth. Analg. 2002, 94, 1489–1494. [Google Scholar] [CrossRef] [PubMed]
- Voss, J.A.; Good, M.; Yates, B.; Baun, M.M.; Thompson, A.; Hertzog, M. Sedative music reduces anxiety and pain during chair rest after open-heart surgery. Pain 2004, 112, 197–203. [Google Scholar] [CrossRef] [PubMed]
- Khalfa, S.; Bella, S.D.; Roy, M.; Peretz, I.; Lupien, S.J. Effects of Relaxing Music on Salivary Cortisol Level after Psychological Stress. Ann. N. Y. Acad. Sci. 2003, 999, 374–376. [Google Scholar] [CrossRef]
- Uedo, N.; Ishikawa, H.; Morimoto, K.; Ishihara, R.; Narahara, H.; Akedo, I.; Ioka, T.; Kaji, I.; Fukuda, S. Reduction in salivary cortisol level by music therapy during colonoscopic examination. Hepatogastroenterology 2004, 51, 451–453. [Google Scholar]
- Hasanah, I.; Mulatsih, S.; Haryanti, F.; Haikal, Z. Effect of music therapy on cortisol as a stress biomarker in children undergoing IV-line insertion. J. Taibah Univ. Med. Sci. 2020, 15, 238–243. [Google Scholar] [CrossRef]
- Hou, Y.-C.; Lin, Y.-J.; Lu, K.-C.; Chiang, H.-S.; Chang, C.-C.; Yang, L.-K. Music Therapy-Induced Changes in Salivary Cortisol Level are Predictive of Cardiovascular Mortality in Patients under Maintenance Hemodialysis. Ther. Clin. Risk Manag. 2017, 13, 263–272. [Google Scholar] [CrossRef] [Green Version]
- Trappe, H.-J.; Voit, G. The Cardiovascular Effect of Musical Genres. Dtsch. Arztebl. Int. 2016, 113, 347–352. [Google Scholar] [CrossRef] [Green Version]
- Tervaniemi, M.; Makkonen, T.; Nie, P. Psychological and Physiological Signatures of Music Listening in Different Listening Environments—An Exploratory Study. Brain Sci. 2021, 11, 593. [Google Scholar] [CrossRef]
- Cotoia, A.; Dibello, F.; Moscatelli, F.; Sciusco, A.; Polito, P.; Modolo, A.; Gallo, C.; Cibelli, G.; Cinnella, G. Effects of Tibetan Music on Neuroendocrine and Autonomic Functions in Patients Waiting for Surgery: A Randomized, Controlled Study. Anesthesiol. Res. Pract. 2018, 2018, 9683780. [Google Scholar] [CrossRef]
- Chafin, S.; Roy, M.; Gerin, W.; Christenfeld, N. Music can facilitate blood pressure recovery from stress. Br. J. Health Psychol. 2004, 9 Pt 3, 393–403. [Google Scholar] [CrossRef]
- Lingham, J.; Theorell, T. Self-selected “favourite” stimulative and sedative music listening—How does familiar and preferred music listening affect the body? Nord. J. Music Ther. 2009, 18, 150–166. [Google Scholar] [CrossRef]
- Shaffer, F.; Ginsberg, J.P. An Overview of Heart Rate Variability Metrics and Norms. Front. Public Health 2017, 5, 258. [Google Scholar] [CrossRef]
- Kunikullaya, U.K.; Vijayadas; Kunnavil, R.; Goturu, J.; Prakash, V.S.; Murthy, N.S. Short-term effects of passive listening to an Indian musical scale on blood pressure and heart rate variability among healthy individuals—A randomised controlled trial. Indian J. Physiol. Pharmacol. 2022, 66, 29–44. [Google Scholar] [CrossRef]
- Lee, W.-L.; Sung, H.-C.; Liu, S.-H.; Chang, S.-M. Meditative music listening to reduce state anxiety in patients during the uptake phase before positron emission tomography (PET) scans. Br. J. Radiol. 2017, 90, 20160466. [Google Scholar] [CrossRef] [Green Version]
- Kirthana Kunikullaya, U.; Sasidharan, A.; Srinivasa, R.; Goturu, J.; Murthy, N.S. Temporal changes in electroencephalographic power spectrum on passive listening to three selected melodic scales of Indian music on healthy young individuals—A randomized controlled trial. Music. Med. 2022, 14, 06–26. [Google Scholar] [CrossRef]
- Valenti, V.E.; Guida, H.L.; Frizzo, A.C.F.; Cardoso, A.C.V.; Vanderlei, L.C.M.; de Abreu, L.C. Auditory stimulation and cardiac autonomic regulation. Clinics 2012, 67, 955–958. [Google Scholar] [CrossRef]
- Raja, D. ‘Deepak Raja’s World of Hindustani Music: Raga Miya-Ki Todi…. Reluctant Differentiation’, Deepak Raja’s World of Hindustani Music, 24 April 2011. Available online: http://swaratala.blogspot.com/2011/04/raga-miya-ki-todi-reluctant.html (accessed on 19 March 2020).
- Film Songs in Rag Mian Ki Todi. Available online: https://chandrakantha.com/raga_raag/film_song_raga/mian_ki_todi.shtml (accessed on 19 March 2020).
- ‘The Raga Guide—Malkauns’, 20 June 2009. Available online: https://web.archive.org/web/20090620030217/http://www.wyastone.co.uk/nrl/world/raga/malkauns.html (accessed on 19 March 2020).
- Raag Puriya—Indian Classical Music—Tanarang.com. Available online: http://www.tanarang.com/english/puriya_eng.htm (accessed on 19 March 2020).
- ‘Puriya’, Wikipedia. 20 November 2019. Available online: https://en.wikipedia.org/w/index.php?title=Puriya&oldid=927072231 (accessed on 19 March 2020).






| Svara/Note | Hindustani Name | Staff Note | Western Scale Interval Name |
|---|---|---|---|
| Raga Miyan ki Todi (Scale A) (heptatonic, G appears in descent) | |||
| S | Shadja | C | Perfect unison |
| r | Komal Rishab | D♭ | Minor second |
| g | Komal Gandhar | E♭ | Minor third |
| M | Tivra Madhyam | F# | Augmented fourth |
| P | Pancham | G | Perfect fifth |
| d | Komal Dhaivat | A♭ | Minor sixth |
| N | Shuddha Nishad | B | Major seventh |
| Raga Malkauns (Scale B) Ascent and descent same—pentatonic | |||
| S | Shadja | C | Perfect unison |
| g | Komal Gandhar | E♭ | Minor third |
| m | Shuddha Madhyam | F | Perfect fourth |
| d | Komal Dhaivat | A♭ | Minor sixth |
| n | Komal Nishad | B♭ | Minor seventh |
| Raga Puriya (Scale C) C, D♭, E, G♭, G, A/A♭, B (hexatonic) | |||
| S | Shadja | C | Perfect unison |
| r | Komal Rishab | D♭ | Minor second |
| G | Shuddha Gandhar | E | Major third |
| M | Tivra Madhyam | F# | Augmented fourth |
| D | Shuddha Dhaivat | A | Major sixth |
| N | Shuddha Nishad | B | Major seventh |
| Variables | Group A | Group B | Group C | Group D | p-Value |
|---|---|---|---|---|---|
| Sample | N = 37 (%) | N = 36 (%) | N = 36 (%) | N = 35 (%) | |
| Age (Years) | |||||
| <=18 | 9 (24.3) | 5 (13.9) | 6 (16.7) | 4 (11.4) | 0.171 |
| 19–21 | 18 (48.6) | 18 (50.0) | 15 (41.7) | 19 (54.3) | |
| 22–24 | 8 (21.6) | 11 (30.6) | 11 (30.6) | 4 (11.4) | |
| >=25 | 2 (5.4) | 2 (5.6) | 4 (11.1) | 8 (22.9) | |
| Age (years) Mean, SD | 20.54, 2.5 | 20.75, 2.5 | 21.11, 2.6 | 21.26, 3.0 | 0.646 |
| Gender | |||||
| Female | 29 (78.4) | 20 (55.6) | 24 (66.7) | 25 (71.4) | 0.202 |
| Male | 8 (21.6) | 16 (44.4) | 12 (33.3) | 10 (28.6) | |
| Education | |||||
| High school/Intermediate | 16 (43.2) | 7 (19.4) | 16 (44.4) | 29 (82.9) | <0.001 |
| Graduate/Postgraduate | 21 (56.8) | 29 (80.6) | 20 (55.6) | 6 (17.1) | |
| Marital status | |||||
| Married | 36 (97.3) | 35 (97.2) | 35 (97.2) | 33 (94.3) | 0.875 |
| Single | 1 (2.7) | 1 (2.8) | 1 (2.8) | 2 (5.7) | |
| Diet | |||||
| Vegetarian | 14 (37.8) | 11 (30.6) | 7 (19.4) | 16 (45.7) | 0.112 |
| Non-vegetarian | 23 (62.2) | 25 (69.4) | 29 (80.6) | 19 (54.3) | |
| BMI (kg/m2) Mean, SD | 23.17, 3.96 | 22.96, 4.71 | 22.16, 3.47 | 22.47, 4.10 | 0.714 |
| Music Training—Yes—N (%) | 17 (45.9) | 14 (38.9) | 11 (30.6) | 12 (34.3) | 0.562 |
| Group | Mean | SD | md | Quartiles | p | |||
|---|---|---|---|---|---|---|---|---|
| 25 | 50 | 75 | ||||||
| STAI State Anxiety | ||||||||
| A (N = 37) | Pre | 35.16 | 10.8 | 2.35 | 28.5 | 33 | 40 | 0.054 |
| Post | 32.81 | 10.7 | 24.5 | 30 | 39 | |||
| B (N = 36) | Pre | 34.92 | 12.3 | 3.83 | 24.5 | 30.5 | 44.3 | 0.057 |
| Post | 31.08 | 8.9 | 23.5 | 29 | 34 | |||
| C (N = 36) | Pre | 36.11 | 11.7 | 3.94 | 25.5 | 35.5 | 43.8 | 0.018 |
| Post | 32.17 | 10.3 | 25 | 29.5 | 37 | |||
| D (N = 34) | Pre | 34.21 | 7.2 | 0.32 | 30 | 32.5 | 37 | 0.781 |
| Post | 33.74 | 8.3 | 28 | 30.5 | 40 | |||
| STAI Trait Anxiety | ||||||||
| A (N = 37) | Pre | 56 | 10.4 | −1.87 | 47 | 58 | 63.5 | 0.057 |
| Post | 57.87 | 9.8 | 51 | 58 | 64 | |||
| B (N = 36) | Pre | 57.44 | 8.4 | −1.08 | 51.25 | 57 | 64 | 0.135 |
| Post | 58.53 | 8.2 | 53.3 | 59 | 63 | |||
| C (N = 36) | Pre | 57.69 | 9.3 | −2.33 | 51 | 57.5 | 64.5 | 0.011 |
| Post | 60.03 | 9.4 | 53 | 60 | 66.8 | |||
| D (N = 34) | Pre | 59.32 | 8.0 | −0.88 | 53 | 60 | 65 | 0.302 |
| Post | 60.09 | 9.0 | 54 | 61 | 67 | |||
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kunikullaya Ubrangala, K.; Kunnavil, R.; Sanjeeva Vernekar, M.; Goturu, J.; Vijayadas; Prakash, V.S.; Murthy, N.S. Effect of Indian Music as an Auditory Stimulus on Physiological Measures of Stress, Anxiety, Cardiovascular and Autonomic Responses in Humans—A Randomized Controlled Trial. Eur. J. Investig. Health Psychol. Educ. 2022, 12, 1535-1558. https://doi.org/10.3390/ejihpe12100108
Kunikullaya Ubrangala K, Kunnavil R, Sanjeeva Vernekar M, Goturu J, Vijayadas, Prakash VS, Murthy NS. Effect of Indian Music as an Auditory Stimulus on Physiological Measures of Stress, Anxiety, Cardiovascular and Autonomic Responses in Humans—A Randomized Controlled Trial. European Journal of Investigation in Health, Psychology and Education. 2022; 12(10):1535-1558. https://doi.org/10.3390/ejihpe12100108
Chicago/Turabian StyleKunikullaya Ubrangala, Kirthana, Radhika Kunnavil, Mamta Sanjeeva Vernekar, Jaisri Goturu, Vijayadas, V. S. Prakash, and Nandagudi Srinivasa Murthy. 2022. "Effect of Indian Music as an Auditory Stimulus on Physiological Measures of Stress, Anxiety, Cardiovascular and Autonomic Responses in Humans—A Randomized Controlled Trial" European Journal of Investigation in Health, Psychology and Education 12, no. 10: 1535-1558. https://doi.org/10.3390/ejihpe12100108
APA StyleKunikullaya Ubrangala, K., Kunnavil, R., Sanjeeva Vernekar, M., Goturu, J., Vijayadas, Prakash, V. S., & Murthy, N. S. (2022). Effect of Indian Music as an Auditory Stimulus on Physiological Measures of Stress, Anxiety, Cardiovascular and Autonomic Responses in Humans—A Randomized Controlled Trial. European Journal of Investigation in Health, Psychology and Education, 12(10), 1535-1558. https://doi.org/10.3390/ejihpe12100108