Biocompatible Nanocomposite Coatings Deposited via Layer-by-Layer Assembly for the Mechanical Reinforcement of Highly Porous Interconnected Tissue-Engineered Scaffolds
Abstract
:1. Introduction
2. Materials and Methods
2.1. Substrate and Polyelectrolyte Preparation
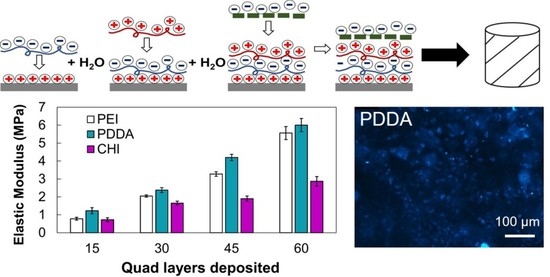
2.2. Coating Method
2.3. Zeta Potential
2.4. Scanning Electron Microscopy with Energy-Dispersive X-ray (SEM-EDX)
2.5. Stylus Profilometry
2.6. Coating Density
2.7. Micro-Computed Tomography (CT)
2.8. Instron Mechanical Testing
2.9. Cell Culture
2.10. Cell Count and Seeding
2.11. In Vitro Cell Assay to Measure Cell Viability
2.12. Scanning Electron Microscopy of U-2 OS Cells
2.13. 4′,6-Diamidino-2-Phenylindole (DAPI) Staining
2.14. Statistical Analysis
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Soni, V. Bone Defect Biodegradable Block Copolymers and Their Applications for Drug Delivery Endochondral Ossification; Tekade, R.K., Ed.; Academic Press: Cambridge, MA, USA, 2019; pp. 401–447. [Google Scholar]
- Schemitsch, E.H. Size Matters: Defining Critical in Bone Defect Size! J. Orthop. Trauma 2017, 31 (Suppl. S5), S20–S22. [Google Scholar] [CrossRef] [PubMed]
- Ogretmen, B. HHS Public Access. Physiol. Behav. 2019, 176, 139–148. [Google Scholar]
- OrthoInfo. Bone Healing; 2020; pp. 1–6. [Google Scholar]
- Winkler, T.; Sass, F.A.; Duda, G.N.; Schmidt-Bleek, K. A review of biomaterials in bone defect healing, remaining shortcomings and future opportunities for bone tissue engineering: The unsolved challenge. Bone Jt. Res. 2018, 7, 232–243. [Google Scholar] [CrossRef] [PubMed]
- Roddy, E.; DeBaun, M.R.; Daoud-Gray, A.; Yang, Y.P.; Gardner, M.J. Treatment of critical-sized bone defects: Clinical and tissue engineering perspectives. Eur. J. Orthop. Surg. Traumatol. 2018, 28, 351–362. [Google Scholar] [CrossRef]
- Zeng, J.-H.; Liu, S.-W.; Xiong, L.; Qiu, P.; Ding, L.-H.; Xiong, S.-L.; Li, J.-T.; Liao, X.-G.; Tang, Z.-M. Scaffolds for the repair of bone defects in clinical studies: A systematic review. J. Orthop. Surg. Res. 2018, 13, 33. [Google Scholar] [CrossRef]
- Reichert, J.C. Tissue Engineering Bone—Reconstruction of Critical Sized Segmental Bone Defects in a Large Animal Model. Ph.D. Thesis, Queensland University of Technology, Brisbane City, Australia, 2010. [Google Scholar]
- Sohn, H.-S.; Oh, J.-K. Review of bone graft and bone substitutes with an emphasis on fracture surgeries. Biomater. Res. 2019, 23, 9. [Google Scholar] [CrossRef] [Green Version]
- Lee, F.H.; Shen, P.C.; Jou, I.M.; Li, C.Y.; Hsieh, J.L. A Population-Based 16-Year on the Risk Factors of Surgical Site Infection in Patients after Bone Grafting: A Cross-Sectional Study in Taiwan. Medicine 2015, 94, e2034. [Google Scholar] [CrossRef]
- Wang, W.; Yeung, K.W.K. Bone grafts and biomaterials substitutes for bone defect repair: A review. Bioact. Mater. 2017, 2, 224–247. [Google Scholar] [CrossRef]
- Shin, S.Y.; Rios, H.F.; Giannobile, W.V.; Oh, T.J. Periodontal Regeneration; Vishwakarma, A., Sharpe, P., Ramalingan, M., Eds.; Academic Press: Cambridge, MA, USA, 2015; pp. 433–444. [Google Scholar]
- Eltom, A.; Zhong, G.; Muhammad, A. Scaffold Techniques and Designs in Tissue Engineering Functions and Purposes: A Review. Adv. Mater. Sci. Eng. 2019, 2019, 3429527. [Google Scholar] [CrossRef] [Green Version]
- Polo-Corrales, L.; Latorre-Esteves, M.; Ramirez-Vick, J.E. Scaffold design for bone regeneration. J. Nanosci. Nanotechnol. 2014, 14, 15–56. [Google Scholar] [CrossRef] [Green Version]
- Ghassemi, T.; Shahroodi, A.; Ebrahimzadeh, M.H.; Mousavian, A.; Movaffagh, J.; Moradi, A. Current Concepts in Scaffolding for Bone Tissue Engineering. Arch. Bone Jt. Surg. 2018, 6, 90–99. [Google Scholar] [PubMed]
- Gerhardt, L.-C.; Boccaccini, A. Review—Bioactive Glass and Glass-Ceramic Scaffolds for Bone Tissue Engineering. Materials 2010, 3, 3867–3910. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Lee, S.; Porter, M.; Wasko, S.; Lau, G.; Chen, P.-Y.; Novitskaya, E.E.; Tomsia, A.P.; Almutairi, A.; Meyers, M.; McKittrick, J. Potential bone replacement materials prepared by two methods. Mater. Res. Soc. Symp. Proc. 2012, 1418, 177–188. [Google Scholar] [CrossRef] [Green Version]
- Matabola, K.P.; Bambo, M.F.; Sikhwivhilu, K.; Vatsha, B.; Moutloali, R.M. Chemical Grafting of Polystyrene Sodium Sulfonate (PSS) onto Polyethersulfone (PES) Powder and Effect on the Characteristics of the Resultant Ultrafiltration Membranes. Mater. Today Proc. 2015, 2, 3957–3963. [Google Scholar] [CrossRef]
- Ziminska, M.; Dunne, N.; Hamilton, A.R. Porous Materials with Tunable Structure and Mechanical Properties via Templated Layer-by-Layer Assembly. ACS Appl. Mater. Interfaces 2016, 8, 21968–21973. [Google Scholar] [CrossRef] [Green Version]
- Khansarizadeh, M.; Mokhtarzadeh, A.; Rashedinia, M.; Taghdisi, S.; Lari, P.; Abnous, K.; Ramezani, M. Identification of possible cytotoxicity mechanism of polyethylenimine by proteomics analysis. Hum. Exp. Toxicol. 2016, 35, 377–387. [Google Scholar] [CrossRef] [PubMed]
- Ding, C.; Xu, S.; Wang, J.; Liu, Y.; Chen, P.; Feng, S. Controlled loading and release of methylene blue in layer-by-layer assembled polyelectrolyte films. Mater. Sci. Eng. C 2012, 32, 670–673. [Google Scholar] [CrossRef]
- Acevedo-Fani, A.; Salvia-Trujillo, L.; Soliva-Fortuny, R.; Martín-Belloso, O. Modulating biopolymer electrical charge to optimize the assembly of edible multilayer nanofilms by the layer-by-layer technique. Biomacromolecules 2015, 16, 2895–2903. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Michel, M.; Toniazzo, V.; Ruch, D.; Ball, V. Deposition Mechanisms in Layer-by-Layer or Step-by-Step Deposition Methods: From Elastic and Impermeable Films to Soft Membranes with Ion Exchange Properties. ISRN Mater. Sci. 2012, 2012, 701695. [Google Scholar] [CrossRef] [Green Version]
- McManus, L.L.; Bonnier, F.; Burke, G.A.; Meenan, B.J.; Boyd, A.R.; Byrne, H.J. Assessment of an osteoblast-like cell line as a model for human primary osteoblasts using Raman spectroscopy. Analyst 2012, 137, 1559–1569. [Google Scholar] [CrossRef] [Green Version]
- Lavalle, P.; Schaaf, P.; Boulmedais, F. Polyelectrolyte Multilayers: A Versatile Tool for Preparing Antimicrobial Coatings. Langmuir 2015, 31, 12856–12872. [Google Scholar] [CrossRef]
- Podsiadlo, P.; Michel, M.; Lee, J.; Verploegen, E.; Kam, N.W.S.; Ball, V.; Lee, J.; Qi, Y.; Hart, A.J.; Hammond, P.T.; et al. Exponential Growth of LBL Films with Incorporated Inorganic Sheets. Nano Lett. 2008, 8, 1762–1770. [Google Scholar] [CrossRef] [PubMed]
- Wu, R.; Li, Y.; Shen, M.; Yang, X.; Zhang, L.; Ke, X.; Yang, G.; Gao, C.; Gou, Z.; Xu, S. Bone tissue regeneration: The role of finely tuned pore architecture of bioactive scaffolds before clinical translation. Bioact. Mater. 2021, 6, 1242–1254. [Google Scholar] [CrossRef] [PubMed]
- Paul, A.; Eun, C.J.; Song, J.M. Cytotoxicity mechanism of non-viral carriers polyethylenimine and poly-l-lysine using real time high-content cellular assay. Polymer 2014, 55, 5178–5188. [Google Scholar] [CrossRef]
- Larsen, A.K.; Malinska, D.; Koszela-Piotrowska, I.; Parhamifar, L.; Hunter, A.C.; Moghimi, S.M. Polyethylenimine-mediated impairment of mitochondrial membrane potential, respiration and membrane integrity: Implications for nucleic acid delivery and gene therapy. Mitochondrion 2012, 12, 162–168. [Google Scholar] [CrossRef]
- Abbina, S.; Mohtaram, N.K.; Kizhakkedathu, J.N. Cell surface engineering. In Functional Biopolymers; Springer: Cham, Switzerland, 2019; pp. 307–346. [Google Scholar] [CrossRef]
- Sharifi-Rad, J.; Quispe, C.; Butnariu, M.; Rotariu, L.S.; Sytar, O.; Sestito, S.; Rapposelli, S.; Akram, M.; Iqbal, M.; Krishna, A.; et al. Chitosan nanoparticles as a promising tool in nanomedicine with particular emphasis on oncological treatment. Cancer Cell Int. 2021, 21, 318. [Google Scholar] [CrossRef]
- Henkel, J.; Woodruff, M.; Epari, D.; Steck, R.; Glatt, V.; Dickinson, I.C.; Choong, P.; Schuetz, M.A.; Hutmacher, D.W. Bone Regeneration Based on Tissue Engineering Conceptions—A 21st Century Perspective. Bone Res. 2013, 1, 216–248. [Google Scholar] [CrossRef] [Green Version]
- McIvor, M.J.; Sharma, P.K.; Birt, C.E.; McDowell, H.; Wilson, S.; McKillop, S.; Acheson, J.G.; Boyd, A.R.; Meenan, B.J. Direct monitoring of single-cell response to biomaterials by Raman spectroscopy. J. Mater. Sci. Mater. Med. 2021, 32, 148. [Google Scholar] [CrossRef]
- Rodzeń, K.; McIvor, M.J.; Sharma, P.K.; Acheson, J.G.; McIlhagger, A.; Mokhtari, M.; McFerran, A.; Ward, J.; Meenan, B.J.; Boyd, A.R. The surface characterisation of fused filament fabricated (FFF) 3D printed peek/hydroxyapatite composites. Polymers 2021, 13, 3117. [Google Scholar] [CrossRef]








| Solution | Dip Time | ||
|---|---|---|---|
| PEI | PDDA | CHI | 2 s |
| DI Rinse | DI Rinse | DI Rinse | 3 s |
| PAA | PAA | ALG | 2 s |
| DI Rinse | DI Rinse | DI Rinse | 3 s |
| PEI | PDDA | CHI | 2 s |
| DI Rinse | DI Rinse | DI Rinse | 3 s |
| NC | NC | NC | 2 s |
| DI Rinse | DI Rinse | DI Rinse | 3 s |
| Polyelectrolyte | Ζ-Potential (mV) | pH |
|---|---|---|
| PEI | 7.63 ± 0.6 | 11 |
| PAA | −25.87 ± 5.9 | 8 |
| PDDA | 21.5 ± 2.57 | 4.4 |
| CHI | 11.63 ± 0.76 | 7 |
| ALG | −31.33 ± 2.20 | 3 |
| NC | −28.61 ± 0.30 | 8 |
| Stylus Type | Radius = 2 µm |
| Range | 534 µm |
| Length | 5000 µm |
| Duration | 60 s |
| Stylus Force | 3 mg |
| Profile | Hills and Valleys |
| 15 QL | 60 QL | |||
|---|---|---|---|---|
| Mean Density (g/cm3) | Std. Dev | Mean Density (g/cm3) | Std. Dev | |
| PEI | 1.12 | 0.26 | 1.29 | 0.29 |
| PDDA | 1.14 | 0.26 | 1.36 | 0.37 |
| CHI | 1.76 | 0.58 | 2.64 | 0.67 |
| PEI Coating | PDDA Coating | CHI Coating | ||||
|---|---|---|---|---|---|---|
| Element | Atomic % | Std. Dev | Atomic % | Std. Dev | Atomic % | Std. Dev |
| C | 23.33 | 0.38 | 49.63 | 0.57 | 38.23 | 0.85 |
| O | 36.97 | 0.68 | 31.03 | 4.88 | 39.53 | 0.86 |
| N | 25.67 | 1.01 | 5.93 | 3.17 | 5.07 | 0.25 |
| Si | 6.57 | 0.06 | 6.67 | 1.08 | 10.13 | 0.86 |
| Al | 2.97 | 0.50 | 3.05 | 0.64 | 4.03 | 0.15 |
| Na | 0.00 | 0.00 | 0.00 | 0.00 | 0.30 | 0.10 |
| 15 QL | 60 QL | |||
|---|---|---|---|---|
| Total Porosity (%) | Std. Dev | Total Porosity (%) | Std. Dev | |
| PEI | 95.85 | 0.40 | 88.87 | 1.01 |
| PDDA | 93.55 | 1.35 | 88.64 | 0.60 |
| CHI | 95.92 | 0.68 | 89.28 | 0.51 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
McFerran, A.; McIvor, M.J.; Lemoine, P.; Meenan, B.J.; Acheson, J.G. Biocompatible Nanocomposite Coatings Deposited via Layer-by-Layer Assembly for the Mechanical Reinforcement of Highly Porous Interconnected Tissue-Engineered Scaffolds. Bioengineering 2022, 9, 585. https://doi.org/10.3390/bioengineering9100585
McFerran A, McIvor MJ, Lemoine P, Meenan BJ, Acheson JG. Biocompatible Nanocomposite Coatings Deposited via Layer-by-Layer Assembly for the Mechanical Reinforcement of Highly Porous Interconnected Tissue-Engineered Scaffolds. Bioengineering. 2022; 9(10):585. https://doi.org/10.3390/bioengineering9100585
Chicago/Turabian StyleMcFerran, Aoife, Mary Josephine McIvor, Patrick Lemoine, Brian J. Meenan, and Jonathan G. Acheson. 2022. "Biocompatible Nanocomposite Coatings Deposited via Layer-by-Layer Assembly for the Mechanical Reinforcement of Highly Porous Interconnected Tissue-Engineered Scaffolds" Bioengineering 9, no. 10: 585. https://doi.org/10.3390/bioengineering9100585
APA StyleMcFerran, A., McIvor, M. J., Lemoine, P., Meenan, B. J., & Acheson, J. G. (2022). Biocompatible Nanocomposite Coatings Deposited via Layer-by-Layer Assembly for the Mechanical Reinforcement of Highly Porous Interconnected Tissue-Engineered Scaffolds. Bioengineering, 9(10), 585. https://doi.org/10.3390/bioengineering9100585