Longitudinal Trends in Severe Dyslipidemia in the Czech Population: The Czech MONICA and Czech Post-MONICA Study
Abstract
:1. Introduction
2. Materials and Methods
2.1. Study Population
2.2. Screening Examination
2.3. Laboratory Analysis
2.4. Definition of Major Risk Factors
2.5. Statistical Analysis
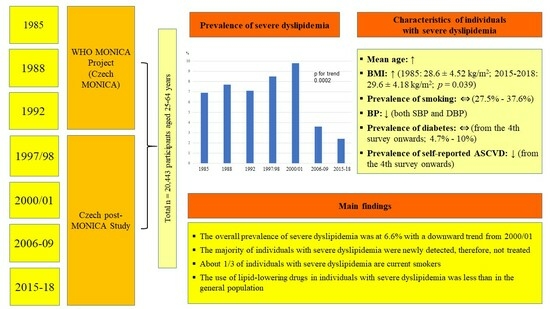
3. Results
3.1. Characteristics of Population Samples
3.2. Prevalence of Severe Dyslipidemia
3.3. Longitudinal Trends in Characteristics of Individuals with Severe Dyslipidemia
3.4. Longitudinal Trends in Lipid Parameters of Individuals with Severe Dyslipidemia
4. Discussion
4.1. Strengths and Limitations
4.2. Implications for the General Population
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Timmis, A.; Vardas, P.; Townsend, N.; Torbica, A.; Katus, H.; De Smedt, D.; Gale, C.P.; Maggioni, A.P.; Petersen, S.E.; Huculeci, R.; et al. European Society of Cardiology: Cardiovascular disease statistics 2021. Eur. Heart J. 2022, 43, 716–799. [Google Scholar] [CrossRef]
- Cífková, R.; Skodová, Z.; Bruthans, J.; Holub, J.; Adámková, V.; Jozífová, M.; Galovcová, M.; Wohlfahrt, P.; Krajčoviechová, A.; Petržílková, Z.; et al. Longitudinal trends in cardiovascular mortality and blood pressure levels, prevalence, awareness, treatment, and control of hypertension in the Czech population from 1985 to 2007/2008. J. Hypertens 2010, 28, 2196–2203. [Google Scholar] [CrossRef]
- Visseren, F.L.J.; Mach, F.; Smulders, Y.M.; Carballo, D.; Koskinas, K.C.; Bäck, M.; Benetos, A.; Biffi, A.; Boavida, J.M.; Capodanno, D.; et al. 2021 ESC Guidelines on cardiovascular disease prevention in clinical practice. Eur. Heart J. 2021, 42, 3227–3337. [Google Scholar] [CrossRef]
- Mach, F.; Baigent, C.; Catapano, A.L.; Koskinas, K.C.; Casula, M.; Badimon, L.; Chapman, M.J.; De Backer, G.G.; Delgado, V.; Ference, B.A.; et al. 2019 ESC/EAS Guidelines for the management of dyslipidaemias: Lipid modification to reduce cardiovascular risk. Eur. Heart J. 2020, 41, 111–188. [Google Scholar] [CrossRef] [Green Version]
- Bruthans, J.; Cífková, R.; Lánská, V.; O’Flaherty, M.; Critchley, J.A.; Holub, J.; Janský, P.; Zvárová, J.; Capewell, S. Explaining the decline in coronary heart disease mortality in the Czech Republic between 1985 and 2007. Eur. J. Prev. Cardiol. 2014, 21, 829–839. [Google Scholar] [CrossRef]
- Cífková, R.; Bruthans, J.; Wohlfahrt, P.; Krajčoviechová, A.; Šulc, P.; Jozífová, M.; Eremiášová, L.; Pudil, J.; Linhart, A.; Widimský, J., Jr.; et al. 30-year trends in major cardiovascular risk factors in the Czech population, Czech MONICA and Czech post-MONICA, 1985–2016/17. PLoS ONE 2020, 15, e0232845. [Google Scholar] [CrossRef]
- Perak, A.M.; Ning, H.; de Ferranti, S.D.; Gooding, H.C.; Wilkins, J.T.; Lloyd-Jones, D.M. Long-Term Risk of Atherosclerotic Cardiovascular Disease in US Adults With the Familial Hypercholesterolemia Phenotype. Circulation 2016, 134, 9–19. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Tunstall-Pedoe, H.; Kuulasmaa, K.; Mähönen, M.; Tolonen, H.; Ruokokoski, E.; Amouyel, P. Contribution of trends in survival and coronary-event rates to changes in coronary heart disease mortality: 10-year results from 37 WHO MONICA project populations. Monitoring trends and determinants in cardiovascular disease. Lancet 1999, 353, 1547–1557. [Google Scholar] [CrossRef] [PubMed]
- Cífková, R.; Skodová, Z.; Bruthans, J.; Adámková, V.; Jozífová, M.; Galovcová, M.; Wohlfahrt, P.; Krajcoviechová, A.; Poledne, R.; Stávek, P.; et al. Longitudinal trends in major cardiovascular risk factors in the Czech population between 1985 and 2007/8. Czech MONICA and Czech post-MONICA. Atherosclerosis 2010, 211, 676–681. [Google Scholar] [CrossRef] [PubMed]
- Friedewald, W.T.; Levy, R.I.; Fredrickson, D.S. Estimation of the concentration of low-density lipoprotein cholesterol in plasma, without use of the preparative ultracentrifuge. Clin. Chem. 1972, 18, 499–502. [Google Scholar] [CrossRef]
- Evans, A.; Tolonen, H.; Hense, H.W.; Ferrario, M.; Sans, S.; Kuulasmaa, K. Trends in coronary risk factors in the WHO MONICA project. Int. J. Epidemiol. 2001, 30 (Suppl. S1), S35–S40. [Google Scholar] [CrossRef] [Green Version]
- Report of the Expert Committee on the Diagnosis and Classification of Diabetes Mellitus. Diabetes Care 1997, 20, 1183–1197. [CrossRef]
- Sniderman, A.D.; Tsimikas, S.; Fazio, S. The severe hypercholesterolemia phenotype: Clinical diagnosis, management, and emerging therapies. J. Am. Coll. Cardiol. 2014, 63, 1935–1947. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Bucholz, E.M.; Rodday, A.M.; Kolor, K.; Khoury, M.J.; de Ferranti, S.D. Prevalence and Predictors of Cholesterol Screening, Awareness, and Statin Treatment Among US Adults With Familial Hypercholesterolemia or Other Forms of Severe Dyslipidemia (1999–2014). Circulation 2018, 137, 2218–2230. [Google Scholar] [CrossRef] [PubMed]
- Saadatagah, S.; Alhalabi, L.; Farwati, M.; Zordok, M.; Bhat, A.; Smith, C.Y.; Wood-Wentz, C.M.; Bailey, K.R.; Kullo, I.J. The burden of severe hypercholesterolemia and familial hypercholesterolemia in a population-based setting in the US. Am. J. Prev. Cardiol. 2022, 12, 100393. [Google Scholar] [CrossRef] [PubMed]
- Kutkienė, S.; Petrulionienė, Ž.; Laucevičius, A.; Petrylaitė, M.; Maskeliūnaitė, D.; Puronaitė, R.; Kovaitė, M.; Kalibaitaitė, I.; Rinkūnienė, E.; Dženkevičiūtė, V.; et al. Severe dyslipidemia and concomitant risk factors in the middle-aged Lithuanian adults: A cross-sectional cohort study. Lipids Health Dis. 2018, 17, 88. [Google Scholar] [CrossRef] [PubMed]
- Jansen, A.C.; van Aalst-Cohen, E.S.; Tanck, M.W.; Trip, M.D.; Lansberg, P.J.; Liem, A.H.; van Lennep, H.W.; Sijbrands, E.J.; Kastelein, J.J. The contribution of classical risk factors to cardiovascular disease in familial hypercholesterolaemia: Data in 2400 patients. J. Intern. Med. 2004, 256, 482–490. [Google Scholar] [CrossRef] [PubMed]
- Williams, B.; Mancia, G.; Spiering, W.; Agabiti Rosei, E.; Azizi, M.; Burnier, M.; Clement, D.L.; Coca, A.; de Simone, G.; Dominiczak, A.; et al. 2018 ESC/ESH Guidelines for the management of arterial hypertension: The Task Force for the management of arterial hypertension of the European Society of Cardiology and the European Society of Hypertension: The Task Force for the management of arterial hypertension of the European Society of Cardiology and the European Society of Hypertension. J. Hypertens 2018, 36, 1953–2041. [Google Scholar]
- Tolonen, H.; Dobson, A.; Kulathinal, S. Assessing the quality of risk factor survey data: Lessons from the WHO MONICA Project. Eur. J. Cardiovasc. Prev. Rehabil. 2006, 13, 104–114. [Google Scholar]
- Ahmad, Z.; Adams-Huet, B.; Chen, C.; Garg, A. Low prevalence of mutations in known loci for autosomal dominant hypercholesterolemia in a multiethnic patient cohort. Circ. Cardiovasc. Genet. 2012, 5, 666–675. [Google Scholar] [CrossRef] [Green Version]
- Khera, A.V.; Won, H.H.; Peloso, G.M.; Lawson, K.S.; Bartz, T.M.; Deng, X.; van Leeuwen, E.M.; Natarajan, P.; Emdin, C.A.; Bick, A.G.; et al. Diagnostic Yield and Clinical Utility of Sequencing Familial Hypercholesterolemia Genes in Patients With Severe Hypercholesterolemia. J. Am. Coll. Cardiol. 2016, 67, 2578–2589. [Google Scholar] [CrossRef] [PubMed]
- Ruel, I.; Brisson, D.; Aljenedil, S.; Awan, Z.; Baass, A.; Bélanger, A.; Bergeron, J.; Bewick, D.; Brophy, J.M.; Brunham, L.R.; et al. Simplified Canadian Definition for Familial Hypercholesterolemia. Can. J. Cardiol. 2018, 34, 1210–1214. [Google Scholar] [CrossRef] [PubMed]


| 1985 | 1988 | 1992 | 1997/98 | 2000/01 | 2006–2009 | 2015–2018 | p for trend | |
|---|---|---|---|---|---|---|---|---|
| Total | 2570 | 2768 | 2343 | 3208 | 3320 | 3612 | 2621 | |
| Mean age, years | 44.9 ± 11.4 | 45.1 ± 11.3 | 44.7 ± 10.9 | 45.6 ± 10.6 | 46.4 ± 11.0 | 47.1 ± 11.3 | 48.0 ± 10.9 | <0.001 |
| Men | 1253 | 1357 | 1134 | 1538 | 1627 | 1737 | 1250 | |
| Mean age, years | 45.0 ± 11.4 | 45.3 ± 11.3 | 44.6 ± 10.8 | 45.6 ± 10.7 | 46.6± 11.0 | 47.8 ± 11.5 | 48.3 ± 10.9 | <0.001 |
| Response rate (%) | 81.5 | 85.5 | 73.2 | 62.5 | 63.8 | 62.1 | 43.1 | <0.001 |
| Age group, n (%) | ||||||||
| 25–34 | 307 (24.5) | 322 (23.7) | 246 (21.7) | 317 (20.6) | 301 (18.5) | 316 (18.2) | 185 (14.8) | <0.001 |
| 35–44 | 296 (23.6) | 323 (23.8) | 350 (30.9) | 372 (24.2) | 390 (24.0) | 401 (23.1) | 300 (24.0) | ns |
| 45–54 | 334 (26.7) | 361 (26.6) | 310 (27.3) | 507 (33.0) | 472 (29.0) | 404 (23.3) | 332 (26.6) | ns |
| 55–64 | 316 (25.2) | 351 (25.9) | 228 (20.1) | 342 (23.2) | 464 (28.5) | 616 (35.5) | 433 (34.6) | ns |
| Women | 1317 | 1411 | 1209 | 1670 | 1693 | 1875 | 1371 | |
| Mean age, years | 44.9 ± 11.4 | 44.9 ± 11.2 | 44.9 ± 11.0 | 45.5 ± 10.6 | 46.2 ± 11.1 | 46.5 ± 11.2 | 47.7 ± 11.0 | <0.001 |
| Response rate (%) | 85.0 | 88.4 | 76.7 | 66.2 | 64.8 | 63.1 | 48.6 | <0.001 |
| Age group, n (%) | ||||||||
| 25–34 | 322 (24.4) | 342 (24.2) | 266 (22.0) | 331 (19.8) | 330 (19.5) | 377 (20.1) | 224 (16.3) | <0.01 |
| 35–44 | 340 (25.8) | 369 (26.2) | 356 (29.4) | 446 (26.7) | 434 (25.6) | 461 (24.6) | 312 (22.8) | ns |
| 45–54 | 343 (26.0) | 360 (25.5) | 311 (25.7) | 532 (31.9) | 465 (27.5) | 502 (26.8) | 420 (30.6) | ns |
| 55–64 | 312 (23.7) | 340 (24.1) | 276 (22.8) | 361 (21.6) | 464 (27.4) | 535 (28.5) | 415 (30.3) | ns |
| 1985 | 1988 | 1992 | 1997/98 | 2000/01 | 2006–2009 | 2015–2018 | p for trend | |
|---|---|---|---|---|---|---|---|---|
| Number | 178 | 213 | 167 | 273 | 326 | 130 | 64 | |
| Age, years | 49.9 ± 10.6 | 51.0 ± 9.4 | 51.9 ± 8.8 | 51.0 ± 8.8 | 51.9 ± 9.3 | 52.7 ± 9.1 | 53.1 ± 8.1 | 0.005 |
| M/F | 83/95 | 102/111 | 80/87 | 126/147 | 152/174 | 69/61 | 38/26 | ns |
| BMI, kg/m2 | 28.6 ± 4.52 | 28.6 ± 4.39 | 28.7 ± 4.21 | 28.7 ± 4.24 | 29.6 ± 4.97 | 29.1 ± 4.82 | 29.6 ± 4.18 | 0.039 |
| Current smoking (%) | 67 (37.6) | 74 (34.7) | 46 (27.5) | 93 (34.1) | 106 (32.5) | 40 (30.8) | 21 (32.8) | ns |
| SBP, mmHg | 139.8 ± 20.7 | 138.2 ± 20.1 | 140.6 ± 22.4 | 133.9 ± 17.5 | 134.0 ± 18.7 | 136.7 ± 19.6 | 131.8 ± 16.0 | 0.002 |
| DBP, mm Hg | 86.7 ± 11.4 | 85.2 ± 10.7 | 88.3 ± 12.3 | 85.5 ± 10.0 | 84.4 ± 10.3 | 84.5 ± 11.0 | 84.7 ± 10.6 | 0.014 |
| Hypertension (%) | 104 (58.4) | 129 (60.6) | 108 (64.7) | 143 (52.4) | 168 (51.5) | 75 (57.7) | 31 (48.4) | 0.023 |
| Diabetes (%) | - | - | - | 26 (9.5) | 21 (6.4) | 13 (10.0) | 3 (4.7) | ns |
| Personal history of ASCVD (%) | - | - | - | 26 (9.5) | 19 (5.8) | 4 (3.1) | 1 (1.6) | 0.002 |
| 1985 | 1988 | 1992 | 1997/98 | 2000/01 | 2006–2009 | 2015–2018 | p for trend | |
|---|---|---|---|---|---|---|---|---|
| Males | ||||||||
| Total cholesterol, mmol/L | 9.10 ± 1.39 | 8.88 ± 0.89 | 8.77 ± 1.41 | 7.92 ± 0.75 | 7.87 ± 0.75 | 7.98 ± 0.93 | 7.65 ± 0.99 | <0.001 |
| HDL-cholesterol, mmol/L | 1.24 ± 0.36 | 1.26 ± 0.39 | 1.32 ± 0.33 | 1.22 ± 0.28 | 1.24 ± 0.31 | 1.22 ± 0.29 | 1.19 ± 0.25 | ns |
| Non-HDL-cholesterol; mmol/L | 7.85 ± 1.45 | 7.61 ± 1.02 | 7.39 ± 1.29 | 6.62 ± 0.70 | 6.61 ± 0.76 | 6.65 ± 0.74 | 6.46 ± 1.07 | <0.001 |
| Triglycerides, mmol/L | - | - | - | 3.14 ± 3.29 | 2.53 ± 2.13 | 3.23 ± 2.99 | 2.28 ± 2.67 | ns |
| LDL-cholesterol, mmol/L | - | - | - | 5.53 ± 0.48 | 5.58 ± 0.53 | 5.56 ± 0.50 | 5.45 ± 0.41 | ns |
| Lipid lowering drugs (%) | - | - | - | 9 (7.3) | 13 (8.6) | 3 (4.4) | 4 (10.5) | ns |
| Females | ||||||||
| Total cholesterol, mmol/L | 8.95 ± 0.89 | 8.82 ± 0.83 | 8.78 ± 0.75 | 8.11 ± 0.82 | 7.97 ± 0.84 | 7.93 ± 0.66 | 7.69 ± 0.48 | <0.001 |
| HDL-cholesterol, mmol/L | 1.57 ± 0.42 | 1.57 ± 0.37 | 1.58 ± 0.41 | 1.44 ± 0.32 | 1.44 ± 0.38 | 1.49 ± 0.37 | 1.56 ± 0.35 | 0.011 |
| Non-HDL-cholesterol, mmol/L | 7.38 ± 0.90 | 7.26 ± 0.96 | 7.20 ± 0.86 | 6.67 ± 0.85 | 6.51 ± 0.79 | 6.44 ± 0.69 | 6.13 ± 0.43 | <0.001 |
| Triglycerides, mmol/L | - | - | - | 2.15 ± 1.08 | 2.06 ± 1.22 | 1.98 ± 1.09 | 1.53 ± 0.72 | 0.012 |
| LDL-cholesterol, mmol/L | - | - | - | 5.71 ± 0.72 | 5.59 ± 0.59 | 5.55 ± 0.50 | 5.44 ± 0.33 | 0.046 |
| Lipid lowering drugs (%) | - | - | - | 5 (3.4) | 12 (6.9) | 3 (4.9) | 1 (3.9) | ns |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Cífková, R.; Bruthans, J.; Wohlfahrt, P.; Hrubeš Krajčoviechová, A.; Šulc, P.; Jozífová, M.; Eremiášová, L.; Pudil, J.; Linhart, A.; Widimský, J., Jr.; et al. Longitudinal Trends in Severe Dyslipidemia in the Czech Population: The Czech MONICA and Czech Post-MONICA Study. J. Cardiovasc. Dev. Dis. 2023, 10, 328. https://doi.org/10.3390/jcdd10080328
Cífková R, Bruthans J, Wohlfahrt P, Hrubeš Krajčoviechová A, Šulc P, Jozífová M, Eremiášová L, Pudil J, Linhart A, Widimský J Jr., et al. Longitudinal Trends in Severe Dyslipidemia in the Czech Population: The Czech MONICA and Czech Post-MONICA Study. Journal of Cardiovascular Development and Disease. 2023; 10(8):328. https://doi.org/10.3390/jcdd10080328
Chicago/Turabian StyleCífková, Renata, Jan Bruthans, Peter Wohlfahrt, Alena Hrubeš Krajčoviechová, Pavel Šulc, Marie Jozífová, Lenka Eremiášová, Jan Pudil, Aleš Linhart, Jiří Widimský, Jr., and et al. 2023. "Longitudinal Trends in Severe Dyslipidemia in the Czech Population: The Czech MONICA and Czech Post-MONICA Study" Journal of Cardiovascular Development and Disease 10, no. 8: 328. https://doi.org/10.3390/jcdd10080328
APA StyleCífková, R., Bruthans, J., Wohlfahrt, P., Hrubeš Krajčoviechová, A., Šulc, P., Jozífová, M., Eremiášová, L., Pudil, J., Linhart, A., Widimský, J., Jr., Filipovský, J., Mayer, O., Jr., Poledne, R., Stávek, P., Lánská, V., & Strilchuk, L. (2023). Longitudinal Trends in Severe Dyslipidemia in the Czech Population: The Czech MONICA and Czech Post-MONICA Study. Journal of Cardiovascular Development and Disease, 10(8), 328. https://doi.org/10.3390/jcdd10080328