Prediction of Long-Term Survival after Coronary Artery Bypass with Bilateral Internal Thoracic Artery Grafting: External Validation of A Contemporary Nomogram
Abstract
:1. Introduction
2. Materials and Methods
2.1. Ethical Statement
2.2. Study Design
2.3. Patient Population and Data
2.4. Statistical Analysis
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Buttar, S.N.; Yan, T.D.; Taggart, D.P.; Tian, D.H. Long-term and short-term outcomes of using bilateral internal mammary artery grafting versus left internal mammary artery grafting: A meta-analysis. Heart 2017, 103, 1419–1426. [Google Scholar] [CrossRef]
- DeSimone, J.P.; Malenka, D.J.; Weldner, P.W.; Iribarne, A.; Leavitt, B.J.; McCullough, J.N.; Quinn, R.D.; Schmoker, J.D.; Kramer, R.S.; Baribeau, Y.; et al. Coronary revascularization with single versus bilateral mammary arteries: Is it time to change? Ann. Thorac. Surg. 2018, 106, 466–472. [Google Scholar] [CrossRef] [Green Version]
- Kurlansky, P.A.; Traad, E.A.; Dorman, M.J.; Galbut, D.L.; Zucker, M.; Ebra, G. Thirty-year follow-up defines survival benefit for second internal mammary artery in propensity-matched groups. Ann. Thorac. Surg. 2010, 90, 101–108. [Google Scholar] [CrossRef]
- Saran, N.; Locker, C.; Said, S.M.; Daly, R.C.; Maltais, S.; Stulak, J.M.; Greason, K.L.; Pochettino, A.; Schaff, H.V.; Dearani, J.A.; et al. Current trends in bilateral internal thoracic artery use for coronary revascularization: Extending benefit to high-risk patients. J. Thorac. Cardiovasc. Surg. 2018, 155, 2331–2343. [Google Scholar] [CrossRef]
- Zhu, Y.; Lingala, B.; Wang, H.; Woo, Y.J. Bilateral vs. Single internal mammary artery grafts for coronary artery bypass in the united states. Ann. Thorac. Surg. 2021, 111, 629–635. [Google Scholar] [CrossRef]
- Ascione, R.; Underwood, M.J.; Lloyd, C.T.; Jeremy, J.Y.; Bryan, A.J.; Angelini, G.D. Clinical and angiographic outcome of different surgical strategies of bilateral internal mammary artery grafting. Ann. Thorac. Surg. 2001, 72, 959–965. [Google Scholar] [CrossRef]
- Taggart, D.P.; Benedetto, U.; Gerry, S.; Altman, D.G.; Gray, A.M.; Lees, B.; Gaudino, M.; Zamvar, V.; Bochenek, A.; Buxton, B.; et al. Bilateral versus single internal-thoracic-artery grafts at 10 years. N. Engl. J. Med. 2019, 380, 437–446. [Google Scholar] [CrossRef]
- Ziv-Baran, T.; Mohr, R.; Pevni, D.; Ben-Gal, Y. A simple-to-use nomogram to predict long term survival of patients undergoing coronary artery bypass grafting (CABG) using bilateral internal thoracic artery grafting technique. PLoS ONE 2019, 14, e0224310. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Collins, G.S.; Reitsma, J.B.; Altman, D.G.; Moons, K.G. Transparent reporting of a multivariable prediction model for individual prognosis or diagnosis (TRIPOD): The TRIPOD statement. J. Clin. Epidemiol. 2015, 68, 134–143. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Quinn, J.; Kramer, N.; McDermott, D. Validation of the social security death index (SSDI): An important readily-available outcomes database for researchers. West. J. Emerg. Med. 2008, 9, 6–8. [Google Scholar] [PubMed]
- Cattaneo, M.; Malighetti, P.; Spinalli, D. Estimating receiver operative characteristic curves for time-dependent outcomes: The stroccurve package. Stata J. 2017, 17, 1015–1023. [Google Scholar] [CrossRef]
- Royston, P. Tools for checking calibration of a cox model in external validation: Approach based on individual event probabilities. Stata J. 2014, 14, 738–755. [Google Scholar] [CrossRef] [Green Version]
- Ruhe, C. Estimating survival functions after stcox with time-varying coefficients. Stata J. 2016, 16, 867–879. [Google Scholar] [CrossRef] [Green Version]
- Bender, A.; Scheipl, F. Pammtools: Piece-wise exponential additive mixed modeling tools. arXiv 2018, arXiv:1806.01042. Available online: https://arxiv.org/pdf/1806.01042.pdf (accessed on 4 June 2018).
- Breheny, P.; Burchett, W. Visualization of Regression Models Using Visreg. Available online: https://cran.r-project.org/web/packages/visreg/visreg.pdf (accessed on 4 June 2020).
- Carmona-Bayonas, A.; Jimenez-Fonseca, P.; Lamarca, A.; Barriuso, J.; Castano, A.; Benavent, M.; Alonso, V.; Riesco-Martínez, M.D.C.; Alonso-Gordoa, T.; Custodio, A.; et al. Prediction of progression-free survival in patients with advanced, well-differentiated, neuroendocrine tumors being treated with a somatostatin analog: The getne-trasgu study. J. Clin. Oncol. 2019, 37, 2571–2580. [Google Scholar] [CrossRef]
- Harrell, F.E.J. Package ‘rms’. Available online: https://cran.r-project.org/web/packages/rms/rms.pdf (accessed on 29 November 2020).
- Wood, S. Generalized Additive Models: An Introduction with R. Available online: https://cran.r-project.org/web/packages/mgcv/mgcv.pdf (accessed on 27 August 2020).
- Therneau, T. A Package for Survival Analysis in R. Available online: https://cran.r-project.org/web/packages/survival/survival.pdf (accessed on 28 September 2020).
- Therneau, T. Spline Terms in a Cox Model. Available online: https://cran.r-project.org/web/packages/survival/vignettes/splines.pdf (accessed on 25 September 2020).
- Wu, C.; Camacho, F.T.; Wechsler, A.S.; Lahey, S.; Culliford, A.T.; Jordan, D.; Gold, J.P.; Higgins, R.S.D.; Smith, C.R.; Hannan, E.L. Risk score for predicting long-term mortality after coronary artery bypass graft surgery. Circulation 2012, 125, 2423–2430. [Google Scholar] [CrossRef] [Green Version]
- Neumann, F.J.; Sousa-Uva, M.; Ahlsson, A.; Alfonso, F.; Banning, A.P.; Benedetto, U.; Byrne, R.A.; Collet, J.P.; Falk, V.; Head, S.J.; et al. 2018 ESC/EACTS Guidelines on myocardial revascularization. Eur. Heart J. 2019, 40, 87–165. [Google Scholar]
- Kieser, T.M.; Lewin, A.M.; Graham, M.M.; Martin, B.J.; Galbraith, P.D.; Rabi, D.M.; Norris, C.M.; Faris, P.D.; Knudtson, M.L.; Ghali, W.A. Outcomes associated with bilateral internal thoracic artery grafting: The importance of age. Ann. Thorac. Surg. 2011, 92, 1269–1275. [Google Scholar] [CrossRef]
- Toumpoulis, I.K.; Anagnostopoulos, C.E.; Derose, J.J., Jr.; Swistel, D.G. The impact of deep sternal wound infection on long-term survival after coronary artery bypass grafting. Chest 2005, 127, 464–471. [Google Scholar] [CrossRef]
- Toumpoulis, I.K.; Theakos, N.; Dunning, J. Does bilateral internal thoracic artery harvest increase the risk of mediastinitis? Interact. Cardiovasc. Thorac. Surg. 2007, 6, 787–791. [Google Scholar] [CrossRef] [Green Version]
- Magruder, J.T.; Young, A.; Grimm, J.C.; Conte, J.V.; Shah, A.S.; Mandal, K.; Sciortino, C.M.; Zehr, K.J.; Cameron, D.E.; Price, J. Bilateral internal thoracic artery grafting: Does graft configuration affect outcome? J. Thorac. Cardiovasc. Surg. 2016, 152, 120–127. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Toumpoulis, I.K.; Pappa, C.K.; Kanistras, D.A.; Anagnostopoulos, C.E.; Toumpoulis, S.K. Superiority of bilateral internal thoracic artery grafting in long-term survival after coronary artery bypass through the lenses of a bedside risk score. Hell. J. Cardiol. 2022, 64, 15–23. [Google Scholar] [CrossRef] [PubMed]




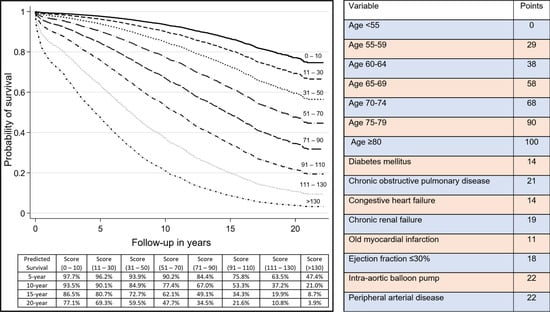
| Variable | Q1 Score 0–38 n = 810 | Q2 Score 39–65 n = 615 | Q3 Score 66–90 n = 734 | Q4 Score > 91 n = 687 | p Value | Points |
|---|---|---|---|---|---|---|
| Female sex, n (%) | 144 (17.8) | 141 (22.9) | 216 (29.4) | 244 (35.5) | <0.001 | - |
| Age, years | <0.001 | - | ||||
| <55, n (%) | 511 (63.1) | 50 (8.1) | 9 (1.2) | 3 (0.4) | - | 0 |
| 55–59, n (%) | 144 (17.8) | 220 (35.8) | 42 (5.7) | 15 (2.2) | - | 29 |
| 60–64, n (%) | 155 (19.1) | 184 (29.9) | 86 (11.7) | 44 (6.4) | - | 38 |
| 65–69, n (%) | 0 | 161 (26.2) | 250 (34.1) | 109 (15.9) | - | 58 |
| 70–74, n (%) | 0 | 0 | 275 (37.5) | 175 (25.5) | - | 68 |
| 75–79, n (%) | 0 | 0 | 72 (9.8) | 189 (27.5) | - | 90 |
| ≥80, n (%) | 0 | 0 | 0 | 152 (22.1) | - | 100 |
| Diabetes mellitus, n (%) | 106 (13.1) | 226 (36.7) | 248 (33.8) | 352 (51.2) | <0.001 | 14 |
| Chronic obstructive pulmonary disease, n (%) | 31 (3.8) | 42 (6.8) | 67 (9.1) | 171 (24.9) | <0.001 | 21 |
| Congestive heart failure, n (%) | 11 (1.4) | 31 (5.0) | 67 (9.1) | 250 (36.4) | <0.001 | 14 |
| Chronic renal failure | 3 (0.4) | 6 (1.0) | 14 (1.9) | 60 (8.7) | <0.001 | 19 |
| Old myocardial infarction, n (%) | 144 (17.8) | 218 (35.4) | 260 (35.4) | 371 (54.0) | <0.001 | 11 |
| Left ventricular ejection fraction ≤30%, n (%) | 39 (4.8) | 79 (12.8) | 121 (16.5) | 279 (40.6) | <0.001 | 18 |
| Intra-aortic balloon pump, n (%) | 6 (0.7) | 15 (2.4) | 16 (2.2) | 41 (6.0) | <0.001 | 22 |
| Peripheral arterial disease, n (% | 11 (1.4) | 37 (6.0) | 48 (6.5) | 193 (28.1) | <0.001 | 22 |
| Body mass index, kg/m2 | <0.001 | - | ||||
| <18.5, n (%) | 5 (0.6) | 7 (1.1) | 5 (0.7) | 13 (1.9) | - | - |
| 18.5–24.99, n (%) | 169 (20.9) | 161 (26.2) | 215 (29.3) | 215 (31.3) | - | - |
| 25.0–39.99, n (%) | 618 (76.3) | 427 (69.4) | 496 (67.6) | 447 (65.1) | - | - |
| ≥40, n (%) | 18 (2.2) | 20 (3.3) | 18 (2.4) | 12 (1.7) | - | - |
| EuroSCORE II, median (IQR) | 1.48 (1.04–2.35) | 1.92 (1.33–2.88) | 2.49 (1.61–3.87) | 5.40 (3.44–9.06) | <0.001 | - |
| Score, median (IQR) | 18 (0–29) | 54 (47–58) | 79 (69–83) | 112 (101–125) | <0.001 | - |
| Number of coronary arteries diseased, median (IQR) | 3 (2–3) | 3 (3–3) | 3 (3–3) | 3 (3–3) | <0.001 | - |
| Distal anastomoses, median (IQR) | 4 (3–4) | 4 (3–4) | 4 (3–4) | 4 (3–4) | 0.035 | - |
| In-hospital mortality, n (%) | 5 (0.6) | 7 (1.1) | 9 (1.2) | 33 (4.8) | <0.001 | |
| Long-term mortality, n (%) | 130 (16.0) | 187 (30.4) | 383 (52.2) | 476 (69.3) | <0.001 | - |
| Follow-up in years, median (IQR) | 14.8 (9.4–18.5) | 12.5 (7.9–16.9) | 10.4 (6.6–14.4) | 7.0 (3.0–11.2) | <0.001 | - |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Toumpoulis, I.K.; Kanistras, D.A.; Pappa, C.K.; Zagoriti, Z.; Anagnostopoulos, C.E.; Toumpoulis, S.K. Prediction of Long-Term Survival after Coronary Artery Bypass with Bilateral Internal Thoracic Artery Grafting: External Validation of A Contemporary Nomogram. J. Cardiovasc. Dev. Dis. 2022, 9, 375. https://doi.org/10.3390/jcdd9110375
Toumpoulis IK, Kanistras DA, Pappa CK, Zagoriti Z, Anagnostopoulos CE, Toumpoulis SK. Prediction of Long-Term Survival after Coronary Artery Bypass with Bilateral Internal Thoracic Artery Grafting: External Validation of A Contemporary Nomogram. Journal of Cardiovascular Development and Disease. 2022; 9(11):375. https://doi.org/10.3390/jcdd9110375
Chicago/Turabian StyleToumpoulis, Ioannis K., Dimitrios A. Kanistras, Christina K. Pappa, Zoi Zagoriti, Constantine E. Anagnostopoulos, and Stavros K. Toumpoulis. 2022. "Prediction of Long-Term Survival after Coronary Artery Bypass with Bilateral Internal Thoracic Artery Grafting: External Validation of A Contemporary Nomogram" Journal of Cardiovascular Development and Disease 9, no. 11: 375. https://doi.org/10.3390/jcdd9110375
APA StyleToumpoulis, I. K., Kanistras, D. A., Pappa, C. K., Zagoriti, Z., Anagnostopoulos, C. E., & Toumpoulis, S. K. (2022). Prediction of Long-Term Survival after Coronary Artery Bypass with Bilateral Internal Thoracic Artery Grafting: External Validation of A Contemporary Nomogram. Journal of Cardiovascular Development and Disease, 9(11), 375. https://doi.org/10.3390/jcdd9110375