Exercise Stress Echocardiography in the Diagnostic Evaluation of Heart Failure with Preserved Ejection Fraction
Abstract
:1. Introduction
2. Pathophysiological Background Supporting the Importance of Exercise Stress Echocardiography for the Diagnosis of HFpEF
3. Exercise Echocardiography Methods
3.1. Clinical Indications
3.2. Exercise Stress Methods
3.3. Stress Protocols, Image Acquisition, and Targeted Parameters
3.4. Interpretation of Test Results and Diagnosis of HFpEF
4. Potential Value of Simultaneous Expired Gas Analysis
5. Conclusions and Future Directions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Borlaug, B.A. Evaluation and management of heart failure with preserved ejection fraction. Nat. Rev. Cardiol. 2020, 17, 559–573. [Google Scholar] [CrossRef] [PubMed]
- Dunlay, S.M.; Roger, V.L.; Redfield, M.M. Epidemiology of heart failure with preserved ejection fraction. Nat. Rev. Cardiol. 2017, 14, 591–602. [Google Scholar] [CrossRef] [PubMed]
- Obokata, M.; Reddy, Y.N.V.; Borlaug, B.A. Diastolic Dysfunction and Heart Failure with Preserved Ejection Fraction: Understanding Mechanisms by Using Noninvasive Methods. JACC Cardiovasc. Imaging 2020, 13, 245–257. [Google Scholar] [CrossRef] [PubMed]
- Obokata, M.; Kane, G.C.; Reddy, Y.N.V.; Olson, T.P.; Melenovsky, V.; Borlaug, B.A. Role of Diastolic Stress Testing in the Evaluation for Heart Failure with Preserved Ejection Fraction: A Simultaneous Invasive-Echocardiographic Study. Circulation 2017, 135, 825–838. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Borlaug, B.A.; Nishimura, R.A.; Sorajja, P.; Lam, C.S.P.; Redfield, M.M. Exercise hemodynamics enhance diagnosis of early heart failure with preserved ejection fraction. Circ. Heart Fail. 2010, 3, 588–595. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Obokata, M.; Borlaug, B.A. Stress Imaging in Heart Failure: Physiologic, Diagnostic, and Therapeutic Insights. Circ. Cardiovasc. Imaging. 2018, 11, e007785. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Lancellotti, P.; Pellikka, P.A.; Budts, W.; Chaudhry, F.A.; Donal, E.; Dulgheru, R.; Edvardsen, T.; Garbi, M.; Ha, J.W.; Kane, G.C.; et al. The Clinical Use of Stress Echocardiography in Non-Ischaemic Heart Disease: Recommendations from the European Association of Cardiovascular Imaging and the American Society of Echocardiography. J. Am. Soc. Echocardiogr. 2017, 30, 101–138. [Google Scholar] [CrossRef] [Green Version]
- Pieske, B.; Tschöpe, C.; De Boer, R.; Fraser, A.G.; Anker, S.D.; Donal, E.; Edelmann, F.; Fu, M.; Guazzi, M.; Lam, C.S.P.; et al. How to diagnose heart failure with preserved ejection fraction: The HFA-PEFF diagnostic algorithm: A consensus recommendation from the Heart Failure Association (HFA) of the European Society of Cardiology (ESC). Eur. Heart J. 2019, 40, 3297–3317. [Google Scholar] [CrossRef] [Green Version]
- Sozzi, F.B.; Maganti, K.; Malanchini, G.; Gherbesi, E.; Tondi, L.; Ciulla, M.M.; Canetta, C.; Lombardi, F. Diastolic stress test in heart failure with preserved ejection fraction. Eur. J. Prev. Cardiol. 2020, 27, 2089–2091. [Google Scholar] [CrossRef] [PubMed]
- Obokata, M.; Reddy, Y.N.V. The Role of Echocardiography in Heart Failure with Preserved Ejection Fraction: What Do We Want from Imaging? Heart Fail. Clin. 2019, 15, 241–256. [Google Scholar] [CrossRef]
- Harada, T.; Kagami, K.; Kato, T.; Obokata, M. Echocardiography in the diagnostic evaluation and phenotyping of heart failure with preserved ejection fraction. J. Cardiol. 2021, 11, 3. [Google Scholar] [CrossRef] [PubMed]
- Verbrugge, F.H.; Omote, K.; Reddy, Y.N.V.; Sorimachi, H.; Obokata, M.; Borlaug, B.A. Heart failure with preserved ejection fraction in patients with normal natriuretic peptide levels is associated with increased morbidity and mortality. Eur. Heart J. 2022. Available online: http://www.ncbi.nlm.nih.gov/pubmed/35139159 (accessed on 1 March 2022). [CrossRef]
- Obokata, M.; Nagata, Y.; Kado, Y.; Kurabayashi, M.; Otsuji, Y.; Takeuchi, M. Ventricular-Arterial Coupling and Exercise-Induced Pulmonary Hypertension During Low-Level Exercise in Heart Failure with Preserved or Reduced Ejection Fraction. J. Card. Fail. 2017, 23, 216–220. [Google Scholar] [CrossRef] [PubMed]
- Obokata, M.; Reddy, Y.N.V.; Pislaru, S.V.; Melenovsky, V.; Borlaug, B.A. Evidence Supporting the Existence of a Distinct Obese Phenotype of Heart Failure with Preserved Ejection Fraction. Circulation 2017, 136, 6–19. [Google Scholar] [CrossRef] [PubMed]
- Gorter, T.; Obokata, M.; Reddy, Y.; Borlaug, B. Exercise Unmasks Distinct Pathophysiologic Features of Pulmonary Vascular Disease in Heart Failure with Preserved Ejection Fraction. Eur. Heart J. 2018, 39, 2825–2835. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Obokata, M.; Olson, T.P.; Reddy, Y.N.V.; Melenovsky, V.; Kane, G.C.; Borlaug, B.A. Haemodynamics, dyspnoea, and pulmonary reserve in heart failure with preserved ejection fraction. Eur. Heart J. 2018, 39, 2810–2821. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Obokata, M.; Reddy, Y.N.V.; Melenovsky, V.; Kane, G.C.; Olson, T.P.; Jarolim, P.; Borlaug, B.A. Myocardial Injury and Cardiac Reserve in Patients with Heart Failure and Preserved Ejection Fraction. J. Am. Coll. Cardiol. 2018, 72, 29–40. [Google Scholar] [CrossRef] [PubMed]
- Obokata, M.; Borlaug, B.A. The strengths and limitations of E/e’ in heart failure with preserved ejection fraction. Eur. J. Heart Fail. 2018, 20, 1312–1314. [Google Scholar] [CrossRef] [PubMed]
- Amanai, S.; Harada, T.; Kagami, K.; Yoshida, K.; Kato, T.; Wada, N.; Obokata, M. The H2FPEF and HFA-PEFF algorithms for predicting exercise intolerance and abnormal hemodynamics in heart failure with preserved ejection fraction. Sci. Rep. 2022, 12, 13. [Google Scholar] [CrossRef] [PubMed]
- Nagueh, S.F.; Smiseth, O.A.; Appleton, C.P.; Byrd, B.F.; Dokainish, H.; Edvardsen, T.; Flachskampf, F.A.; Gillebert, T.C.; Klein, A.L.; Lancellotti, P.; et al. Recommendations for the Evaluation of Left Ventricular Diastolic Function by Echocardiography: An Update from the American Society of Echocardiography and the European Association of Cardiovascular Imaging. J. Am. Soc. Echocardiogr. 2016, 29, 277–314. [Google Scholar] [CrossRef] [Green Version]
- Sharifov, O.F.; Schiros, C.G.; Aban, I.; Denney, T.S.; Gupta, H. Diagnostic accuracy of tissue Doppler index E/e’ for evaluating left ventricular filling pressure and diastolic dysfunction/heart failure with preserved ejection fraction: A systematic review and meta-analysis. J. Am. Heart Assoc. 2016, 5, e002530. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Reddy, Y.N.V.; Carter, R.E.; Obokata, M.; Redfield, M.M.; Borlaug, B.A. A Simple, Evidence-Based Approach to Help Guide Diagnosis of Heart Failure with Preserved Ejection Fraction. Circulation 2018, 138, 861–870. [Google Scholar] [CrossRef] [PubMed]
- Rendón-Giraldo, J.A.; Lema, C.; Saldarriaga-Giraldo, C.I. Association between Diastolic Stress Test and H2FPEF Score. Arch. Cardiol México. 2021. Available online: http://www.archivoscardiologia.com/frame_esp.php?id=388 (accessed on 1 March 2022). [CrossRef] [PubMed]
- Tao, Y.; Wang, W.; Zhu, J.; You, T.; Li, Y.; Zhou, X. H2FPEF score predicts 1-year rehospitalisation of patients with heart failure with preserved ejection fraction. Postgrad Med. J. 2021, 97, 164–167. [Google Scholar] [CrossRef] [PubMed]
- Sueta, D.; Yamamoto, E.; Nishihara, T.; Tokitsu, T.; Fujisue, K.; Oike, F.; Takae, M.; Usuku, H.; Takashio, S.; Arima, Y.; et al. H2FPEF Score as a Prognostic Value in HFpEF Patients. Am. J. Hypertens. 2019, 32, 1082–1090. [Google Scholar] [CrossRef] [PubMed]
- Sun, Y.; Wang, N.; Li, X.; Zhang, Y.; Yang, J.; Tse, G.; Liu, Y. Predictive value of H2 FPEF score in patients with heart failure with preserved ejection fraction. ESC Heart Fail. 2021, 8, 1244–1252. [Google Scholar] [CrossRef] [PubMed]
- Hwang, I.-C.; Cho, G.-Y.; Choi, H.-M.; Yoon, Y.E.; Park, J.J.; Park, J.-B.; Park, J.-H.; Lee, S.-P.; Kim, H.-K.; Kim, Y.-J. H2FPEF Score Reflects the Left Atrial Strain and Predicts Prognosis in Patients with Heart Failure with Preserved Ejection Fraction. J. Card. Fail. 2021, 27, 198–207. [Google Scholar] [CrossRef] [PubMed]
- Borlaug, B.A.; Olson, T.P.; Lam, C.S.P.; Flood, K.S.; Lerman, A.; Johnson, B.D.; Redfield, M.M. Global cardiovascular reserve dysfunction in heart failure with preserved ejection fraction. J. Am. Coll. Cardiol. 2010, 56, 845–854. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Van Iterson, E.H.; Johnson, B.D.; Borlaug, B.A.; Olson, T.P. Physiological dead space and arterial carbon dioxide contributions to exercise ventilatory inefficiency in patients with reduced or preserved ejection fraction heart failure. Eur. J. Heart Fail. 2017, 19, 1675–1685. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Haykowsky, M.J.; Brubaker, P.H.; John, J.M.; Stewart, K.P.; Morgan, T.M.; Kitzman, D.W. Determinants of exercise intolerance in elderly heart failure patients with preserved ejection fraction. J. Am. Coll. Cardiol. 2011, 58, 265–274. [Google Scholar] [CrossRef] [Green Version]
- Sorimachi, H.; Burkhoff, D.; Verbrugge, F.H.; Omote, K.; Obokata, M.; Reddy, Y.N.; Takahashi, N.; Sunagawa, K.; Borlaug, B.A. Obesity, venous capacitance, and venous compliance in heart failure with preserved ejection fraction. Eur. J. Heart Fail. 2021, 23, 1648–1658. [Google Scholar] [CrossRef] [PubMed]
- Kawaguchi, M.; Hay, I.; Fetics, B.; Kass, D.A. Combined ventricular systolic and arterial stiffening in patients with heart failure and preserved ejection fraction: Implications for systolic and diastolic reserve limitations. Circulation 2003, 107, 714–720. [Google Scholar] [CrossRef] [PubMed]
- Penicka, M.; Bartunek, J.; Trakalova, H.; Hrabakova, H.; Maruskova, M.; Karasek, J.; Kočka, V. Heart Failure with Preserved Ejection Fraction in Outpatients with Unexplained Dyspnea. A Pressure-Volume Loop Analysis. J. Am. Coll. Cardiol. 2010, 55, 1701–1710. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Obokata, M.; Negishi, K.; Marwick, T.H.; Kurosawa, K.; Ishida, H.; Ito, K.; Ogawa, T.; Ando, Y.; Kurabayashi, M. Comparison of different interdialytic intervals among hemodialysis patients on their echocardiogram-based cardiovascular parameters. Am. Heart J. 2015, 169, 523–530.e2. [Google Scholar] [CrossRef] [PubMed]
- Obokata, M.; Negishi, K.; Kurosawa, K.; Arima, H.; Tateno, R.; Ui, G.; Tange, S.; Arai, M.; Kurabayashi, M. Incremental diagnostic value of la strain with leg lifts in heart failure with preserved ejection fraction. JACC Cardiovasc. Imaging 2013, 6, 749–758. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kusunose, K.; Yamada, H.; Saijo, Y.; Nishio, S.; Hirata, Y.; Ise, T.; Yamaguchi, K.; Fukuda, D.; Yagi, S.; Soeki, T.; et al. Preload Stress Echocardiography for the Assessment of Heart Failure with Preserved Ejection Fraction. JACC Cardiovasc. Imaging 2022, 15, 375–378. [Google Scholar] [CrossRef] [PubMed]
- Borlaug, B.A.; Jaber, W.A.; Ommen, S.R.; Lam, C.S.P.; Redfield, M.M.; Nishimura, R.A. Diastolic relaxation and compliance reserve during dynamic exercise in heart failure with preserved ejection fraction. Heart 2011, 97, 964–969. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Erdei, T.; Smiseth, O.A.; Marino, P.; Fraser, A.G. A systematic review of diastolic stress tests in heart failure with preserved ejection fraction, with proposals from the EU-FP7 MEDIA study group. Eur. J. Heart Fail. 2014, 16, 1345–1361. [Google Scholar] [CrossRef] [PubMed]
- Reddy, Y.N.V.; Olson, T.P.; Obokata, M.; Melenovsky, V.; Borlaug, B.A. Hemodynamic Correlates and Diagnostic Role of Cardiopulmonary Exercise Testing in Heart Failure with Preserved Ejection Fraction. JACC Heart Fail. 2018, 6, 665–675. [Google Scholar] [CrossRef] [PubMed]
- Houstis, N.E.; Eisman, A.S.; Pappagianopoulos, P.P.; Wooster, L.; Bailey, C.S.; Wagner, P.D.; Lewis, G.D. Exercise Intolerance in Heart Failure with Preserved Ejection Fraction. Circulation 2018, 137, 148–161. [Google Scholar] [CrossRef]
- Rao, V.N.; Kelsey, M.D.; Blazing, M.A.; Pagidipati, N.J.; Fortin, T.A.; Fudim, M. Unexplained Dyspnea on Exertion: The Difference the Right Test Can Make. Circ Heart Fail. 2022, 15, e008982. [Google Scholar] [CrossRef] [PubMed]
- Kramer, B.; Massie, B.; Topic, N. Hemodynamic differences between supine and upright exercise in patients with congestive heart failure. Circulation 1982, 66, 820–825. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Bhella, P.S.; Pacini, E.L.; Prasad, A.; Hastings, J.L.; Adams-Huet, B.; Thomas, J.D.; Grayburn, P.A.; Levine, B.D. Echocardiographic indices do not reliably track changes in left-sided filling pressure in healthy subjects or patients with heart failure with preserved ejection fraction. Circ Cardiovasc. Imaging 2011, 4, 482–489. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Maeder, M.T.; Thompson, B.R.; Brunner-La Rocca, H.P.; Kaye, D.M. Hemodynamic basis of exercise limitation in patients with heart failure and normal ejection fraction. J. Am. Coll. Cardiol. 2010, 56, 855–863. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Santos, M.; Rivero, J.; McCullough, S.D.; West, E.; Opotowsky, A.R.; Waxman, A.B.; Systrom, D.M.; Shah, A.M. E/e′ ratio in patients with unexplained dyspnea lack of accuracy in estimating left ventricular filling pressure. Circ Heart Fail. 2015, 8, 749–756. [Google Scholar] [CrossRef] [Green Version]
- Hasenfuß, G.; Hayward, C.; Burkhoff, D.; Silvestry, F.E.; McKenzie, S.; Gustafsson, F.; Malek, F.; Van der Heyden, J.; Lang, I.; Petrie, M.C.; et al. A transcatheter intracardiac shunt device for heart failure with preserved ejection fraction (REDUCE LAP-HF): A multicentre, open-label, single-arm, phase 1 trial. Lancet 2016, 387, 1298–1304. [Google Scholar] [CrossRef] [Green Version]
- Hammoudi, N.; Laveau, F.; Helft, G.; Cozic, N.; Barthelemy, O.; Ceccaldi, A.; Petroni, T.; Berman, E.; Komajda, M.; Michel, P.-L.; et al. Low level exercise echocardiography helps diagnose early stage heart failure with preserved ejection fraction: A study of echocardiography versus catheterization. Clin. Res. Cardiol. 2017, 106, 192–201. [Google Scholar] [CrossRef]
- Bentivegna, E.; Luciani, M.; Martelletti, P. New Model for Non-Invasive Echocardiographic Assessment of Pulmonary-Capillary Wedge Pressure in Patients with Aortic and Mitral Regurgitation. SN Compr. Clin. Med. 2020, 2, 914–918. [Google Scholar] [CrossRef]
- Borlaug, B.A.; Obokata, M. Is it time to recognize a new phenotype? Heart failure with preserved ejection fraction with pulmonary vascular disease. Eur. Heart J. 2017, 38, 2874–2878. [Google Scholar] [CrossRef]
- Guazzi, M. Stress echocardiography combined with cardiopulmonary exercise testing: Opening a new window into diagnosis of heart failure with preserved ejection fraction. Eur. J. Prev. Cardiol. 2016, 23, 67–70. [Google Scholar] [CrossRef]
- Belyavskiy, E.; Morris, D.A.; Url-Michitsch, M.; Verheyen, N.; Meinitzer, A.; Radhakrishnan, A.-K.; Kropf, M.; Frydas, A.; Ovchinnikov, A.G.; Schmidt, A.; et al. Diastolic stress test echocardiography in patients with suspected heart failure with preserved ejection fraction: A pilot study. ESC Heart Fail. 2019, 6, 146–153. [Google Scholar] [CrossRef] [PubMed]
- Shim, C.Y.; Kim, S.-A.; Choi, D.; Yang, W.-I.; Kim, J.-M.; Moon, S.-H.; Lee, H.-J.; Park, S.; Choi, E.-Y.; Chung, N.; et al. Clinical outcomes of exercise-induced pulmonary hypertension in subjects with preserved left ventricular ejection fraction: Implication of an increase in left ventricular filling pressure during exercise. Heart 2011, 97, 1417–1424. [Google Scholar] [CrossRef] [PubMed]
- Donal, E.; Lund, L.H.; Oger, E.; Reynaud, A.; Schnell, F.; Persson, H.; Drouet, E.; Linde, C.; Daubert, C. Value of exercise echocardiography in heart failurewith preserved ejection fraction: A substudy from the KaRen study. Eur. Heart J. Cardiovasc. Imaging 2016, 17, 106–113. [Google Scholar] [PubMed] [Green Version]
- Van Riel, A.C.M.J.; Opotowsky, A.R.; Santos, M.; Rivero, J.M.; Dhimitri, A.; Mulder, B.J.M.; Bouma, B.J.; Landzberg, M.J.; Waxman, A.B.; Systrom, D.M.; et al. Accuracy of Echocardiography to Estimate Pulmonary Artery Pressures with Exercise. Circ. Cardiovasc. Imaging 2017, 10, e005711. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Obokata, M.; Kane, G.C.; Sorimachi, H.; Reddy, Y.N.V.; Olson, T.P.; Egbe, A.C.; Melenovsky, V.; Borlaug, B.A. Noninvasive evaluation of pulmonary artery pressure during exercise: The importance of right atrial hypertension. Eur. Respir J. Eur. Respir. Soc. 2020, 55, 1901617. [Google Scholar] [CrossRef] [PubMed]
- Sperry, B.W.; Campbell, J.; Yanavitski, M.; Kapadia, S.; Tang, W.H.W.; Hanna, M. Peripheral Venous Pressure Measurements in Patients with Acute Decompensated Heart Failure (PVP-HF). Circ. Heart Fail. 2017, 10, e004130. [Google Scholar] [CrossRef]
- Vlismas, P.P.; Wiesenfeld, E.; Oh, K.T.; Murthy, S.; Vukelic, S.; Saeed, O.; Patel, S.; Shin, J.J.; Jorde, U.P.; Sims, D.B. Relation of Peripheral Venous Pressure to Central Venous Pressure in Patients with Heart Failure, Heart Transplant, and Left Ventricular Assist Device. Am. J. Cardiol. 2021, 138, 80–84. [Google Scholar] [CrossRef]
- Yang, J.H.; Harada, T.; Choi, K.H.; Kato, T.; Kim, D.; Takama, N.; Park, T.K.; Kurabayashi, M.; Chang, S.A.; Obokata, M. Peripheral Venous Pressure-Assisted Exercise Stress Echocardiography in the Evaluation of Pulmonary Hypertension During Exercise in Patients with Suspected Heart Failure with Preserved Ejection Fraction. Circ. Heart Fail. 2022. Available online: http://www.ncbi.nlm.nih.gov/pubmed/35189688 (accessed on 1 March 2022). [CrossRef]
- Huang, D.; Dong, M.S.; Ms, S.; Zhang, M. The application of lung ultrasound in acute decompensated heart failure in heart failure with preserved and reduced ejection fraction. Echocardiography 2017, 34, 1462–1469. [Google Scholar]
- Picano, E.; Scali, M.C.; Ciampi, Q.; Lichtenstein, D. Lung Ultrasound for the Cardiologist. JACC Cardiovasc. Imaging 2018, 11, 1692–1705. [Google Scholar] [CrossRef]
- Platz, E.; Jhund, P.S.; Girerd, N.; Pivetta, E.; McMurray, J.J.; Peacock, W.F.; Masip, J.; Martin-Sanchez, F.J.; Miró, O.; Price, S.; et al. Expert consensus document: Reporting checklist for quantification of pulmonary congestion by lung ultrasound in heart failure. Eur. J. Heart Fail. 2019, 21, 844–851. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Scali, M.C.; Zagatina, A.; Simova, I.; Zhuravskaya, N.; Ciampi, Q.; Paterni, M.; Marzilli, M.; Carpeggiani, C.; Picano, E.; Citro, R.; et al. B-lines with Lung Ultrasound: The Optimal Scan Technique at Rest and During Stress. Ultrasound Med. Biol. 2017, 43, 2558–2566. [Google Scholar] [CrossRef] [PubMed]
- Reddy, Y.N.V.; Obokata, M.; Wiley, B.; Koepp, K.E.; Jorgenson, C.C.; Egbe, A.; Melenovsky, V.; Carter, R.E.; Borlaug, B.A. The haemodynamic basis of lung congestion during exercise in heart failure with preserved ejection fraction. Eur. Heart J. 2019, 40, 3721–3730. [Google Scholar] [CrossRef] [PubMed]
- Platz, E.; Merz, A.; Silverman, M.; Lewis, E.; Groarke, J.D.; Waxman, A.; Systrom, D. Association between lung ultrasound findings and invasive exercise haemodynamics in patients with undifferentiated dyspnoea. ESC Heart Fail. 2019, 6, 202–220. [Google Scholar] [CrossRef] [PubMed]
- Coiro, S.; Simonovic, D.; Deljanin-Ilic, M.; Duarte, K.; Carluccio, E.; Cattadori, G.; Girerd, N.; Ambrosio, G. Prognostic Value of Dynamic Changes in Pulmonary Congestion During Exercise Stress Echocardiography in Heart Failure with Preserved Ejection Fraction. Circ. Heart Fail. 2020, 13, e006769. [Google Scholar] [CrossRef] [PubMed]
- Pugliese, N.R.; De Biase, N.; Gargani, L.; Mazzola, M.; Conte, L.; Fabiani, I.; Natali, A.; Dini, F.L.; Frumento, P.; Rosada, J.; et al. Predicting the transition to and progression of heart failure with preserved ejection fraction: A weighted risk score using bio-humoural, cardiopulmonary, and echocardiographic stress testing. Eur. J. Prev. Cardiol. 2021, 28, 1650–1661. [Google Scholar] [CrossRef] [PubMed]
- D’Andrea, A.; Ilardi, F.; D’Ascenzi, F.; Bandera, F.; Benfari, G.; Esposito, R.; Malagoli, A.; Mandoli, G.E.; Santoro, C.; Russo, V.; et al. Impaired myocardial work efficiency in heart failure with preserved ejection fraction. Eur. Heart J. Cardiovasc. Imaging 2021, 22, 1312–1320. [Google Scholar] [CrossRef]
- Kagami, K.; Harada, T.; Yamaguchi, K.; Kouno, S.; Ikoma, T.; Yoshida, K.; Kato, T.; Tomono, J.; Wada, N.; Adachi, T.; et al. Association between lung ultrasound B-lines and exercise-induced pulmonary hypertension in patients with connective tissue disease. Echocardiography 2021, 38, 1297–1306. [Google Scholar] [CrossRef] [PubMed]
- Guazzi, M.; Bandera, F.; Ozemek, C.; Systrom, D.; Arena, R. Cardiopulmonary Exercise Testing: What Is its Value? J. Am. Coll. Cardiol. 2017, 70, 1618–1636. [Google Scholar] [CrossRef]
- Guazzi, M.; Myers, J.; Arena, R. Cardiopulmonary exercise testing in the clinical and prognostic assessment of diastolic heart failure. J. Am. Coll. Cardiol. 2005, 46, 1883–1890. [Google Scholar] [CrossRef] [Green Version]
- Nadruz, W.; West, E.; Sengeløv, M.; Santos, M.; Groarke, J.D.; Forman, D.E.; Claggett, B.; Skali, H.; Shah, A.M. Prognostic Value of Cardiopulmonary Exercise Testing in Heart Failure with Reduced, Midrange, and Preserved Ejection Fraction. J. Am. Heart Assoc. 2017, 6, e006000. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Shafiq, A.; Brawner, C.A.; Aldred, H.A.; Lewis, B.; Williams, C.T.; Tita, C.; Schairer, J.R.; Ehrman, J.K.; Velez, M.; Selektor, Y.; et al. Prognostic value of cardiopulmonary exercise testing in heart failure with preserved ejection fraction. The Henry Ford HospITal CardioPulmonary EXercise Testing (FIT-CPX) project. Am. Heart J. 2016, 174, 167–172. [Google Scholar] [CrossRef] [Green Version]
- Sugimoto, T.; Bandera, F.; Generati, G.; Alfonzetti, E.; Bussadori, C.; Guazzi, M. Left Atrial Function Dynamics During Exercise in Heart Failure: Pathophysiological Implications on the Right Heart and Exercise Ventilation Inefficiency. JACC Cardiovasc. Imaging 2017, 10, 1253–1264. [Google Scholar] [CrossRef] [PubMed]
- Dhakal, B.P.; Malhotra, R.; Murphy, R.M.; Pappagianopoulos, P.P.; Baggish, A.L.; Weiner, R.B.; Houstis, N.E.; Eisman, A.S.; Hough, S.S.; Lewis, G.D. Mechanisms of exercise intolerance in heart failure with preserved ejection fraction: The role of abnormal peripheral oxygen extraction. Circ. Heart Fail. 2015, 8, 286–294. [Google Scholar] [CrossRef] [Green Version]
- Abudiab, M.M.; Redfield, M.M.; Melenovsky, V.; Olson, T.P.; Kass, D.A.; Johnson, B.D.; Borlaug, B.A. Cardiac output response to exercise in relation to metabolic demand in heart failure with preserved ejection fraction. Eur. J. Heart Fail. 2013, 15, 776–785. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kitzman, D.W.; Brubaker, P.H.; Morgan, T.M.; Stewart, K.P.; Little, W.C. Exercise training in older patients with Heart failure and preserved ejection fraction: A randomized, controlled, single-blind trial. Circ. Heart Fail. 2010, 3, 659–667. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kitzman, D.W.; Brubaker, P.; Morgan, T.; Haykowsky, M.; Hundley, G.; Kraus, W.E.; Eggebeen, J.; Nicklas, B.J. Effect of caloric restriction or aerobic exercise training on peak oxygen consumption and quality of life in obese older patients with heart failure with preserved ejection fraction: A randomized clinical trial. JAMA J. Am. Med. Assoc. 2016, 315, 36–46. [Google Scholar] [CrossRef]
- Francis, D.P.; Shamim, W.; Davies, L.C.; Piepoli, M.F.; Ponikowski, P.; Anker, S.D.; Coats, A.S. Cardiopulmonary exercise testing for prognosis in chronic heart failure: Continuous and independent prognostic value from VE/VCO(2)slope and peak VO(2). Eur. Heart J. 2000, 21, 154–161. [Google Scholar] [CrossRef] [PubMed]
- Arena, R.; Myers, J.; Aslam, S.S.; Varughese, E.B.; Peberdy, M.A. Peak VO2 and VE/VCO2 slope in patients with heart failure: A prognostic comparison. Am. Heart J. 2004, 147, 354–360. [Google Scholar] [CrossRef]
- Guazzi, M.; Myers, J.; Peberdy, M.A.; Bensimhon, D.; Chase, P.; Arena, R. Exercise oscillatory breathing in diastolic heart failure: Prevalence and prognostic insights. Eur. Heart J. 2008, 29, 2751–2759. [Google Scholar] [CrossRef] [PubMed]
- Elbehairy, A.F.; Ciavaglia, C.E.; Webb, K.A.; Guenette, J.A.; Jensen, D.; Mourad, S.M.; Neder, J.A.; O’Donnell, D.E. Pulmonary Gas Exchange Abnormalities in Mild Chronic Obstructive Pulmonary Disease. Implications for Dyspnea and Exercise Intolerance. Am. J. Respir. Crit. Care Med. 2015, 191, 1384–1394. [Google Scholar] [CrossRef] [PubMed]
- Shah, S.; Kitzman, D.W.; Borlaug, B.; Van Heerebeek, L.; Zile, M.; Kass, D.A.; Paulus, W.J. Phenotype-specific treatment of heart failure with preserved ejection fraction. Circulation 2016, 134, 73–90. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kosmala, W.; Przewlocka-Kosmala, M.; Rojek, A.; Mysiak, A.; Dabrowski, A.; Marwick, T.H. Association of Abnormal Left Ventricular Functional Reserve with Outcome in Heart Failure with Preserved Ejection Fraction. JACC Cardiovasc. Imaging 2017, 11, 1737–1746. [Google Scholar] [CrossRef] [PubMed]
- Sugimoto, T.; Barletta, M.; Bandera, F.; Generati, G.; Alfonzetti, E.; Rovida, M.; Ruscone, T.G.; Rossi, A.; Cicoira, M.; Guazzi, M. Central role of left atrial dynamics in limiting exercise cardiac output increase and oxygen uptake in heart failure: Insights by cardiopulmonary imaging. Eur. J. Heart Fail. 2020, 22, 1186–1198. [Google Scholar] [CrossRef] [PubMed]
- Marino, P.N.; Zanaboni, J.; Degiovanni, A.; Sartori, C.; Patti, G.; Fraser, A.G. Left atrial conduit flow rate at baseline and during exercise: An index of impaired relaxation in HFpEF patients. ESC Heart Fail. 2021, 8, 4334–4342. [Google Scholar] [CrossRef] [PubMed]






| Key Questions | Gaps in Evidence and Future Studies Needed |
|---|---|
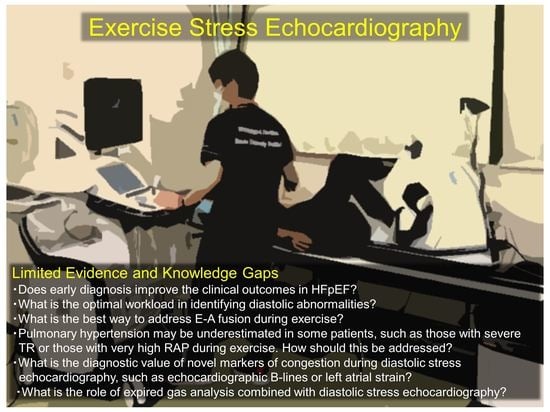
| Diastolic stress echocardiography allows the diagnosis of HFpEF among patients with dyspnea; however, it is unclear whether early diagnosis itself will improve the clinical outcomes. | Echocardiographic markers of congestion during exercise are associated with clinical outcomes in HFpEF, supporting the prognostic value of diastolic stress echocardiography [53,65,83,84]; however, further prospective studies are needed to determine if intervention after an early diagnosis will improve the outcomes. |
| No universally adopted protocols exist, and whether a multistep or ramp protocol is better remains unknown. | Patients with HFpEF are older, and a ramp protocol or a multistep protocol with low initial and incremental workload (e.g., 10 watts) may be preferred [38]. Further studies are required to develop optimal protocols. |
| What is the optimal workload in identifying diastolic abnormalities? It is unclear whether maximal workload is necessary. | Submaximal exercise is likely to be more feasible and equivalent to daily activities; however, few studies have examined its diagnostic value [4]. Further studies are warranted to establish the clinical value of echocardiographic indices measured during submaximal exercise. |
| The E/e′ ratio plays a central role in diastolic stress echocardiography; however, what is the best way to address E–A fusion during exercise? What is the optimal cutoff of E/e′ during exercise in patients with AF? E/e’ ratio cannot be applied to patients with specific diseases, such as mitral valve diseases, mitral valve repair, or prosthetic mitral valves, or in the presence of regional wall motion abnormalities [52]. | The E/e′ ratio during submaximal exercise or the early recovery period can be used to diagnose HFpEF; however, evidence supporting this practice is insufficient. Data on the exercise E/e′ ratio in patients with AF remain limited. Further studies are required to examine the diagnostic value of the exercise E/e′ ratio, using simultaneous invasive right heart catheterization. |
| Identification of pulmonary hypertension during exercise is useful for diagnosing HFpEF. Pulmonary hypertension may be underestimated in some patients, such as those with severe TR or those with very high RAP during exercise. How should this be addressed? | It is unclear how the underestimation of the TR gradient in patients with severe TR should be addressed. Further studies are required. Measurements of peripheral venous pressure may be a useful alternative to RAP measurements during exercise [56,58]. |
| What is the diagnostic value of other candidate markers of congestion during diastolic stress echocardiography, such as echocardiographic B-lines or left atrial strain [85]? | The presence of multiple B-lines may be useful in detecting pulmonary congestion that develops during exercise [63]; however, it is unclear how the data should be interpreted (e.g., the optimal cutoff value for B-lines is unknown). Further studies are warranted to establish the optimal role of the assessment of B-lines in diastolic stress echocardiography. |
| What is the role of expired gas analysis combined with diastolic stress echocardiography? | Simultaneous assessment of exercise capacity (peak oxygen consumption) is the major advantage of diastolic stress echocardiography [39]. Further studies are needed to determine the clinical value of combining diastolic stress echocardiography and expired gas analysis in the diagnosis of HFpEF. |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Harada, T.; Kagami, K.; Kato, T.; Ishii, H.; Obokata, M. Exercise Stress Echocardiography in the Diagnostic Evaluation of Heart Failure with Preserved Ejection Fraction. J. Cardiovasc. Dev. Dis. 2022, 9, 87. https://doi.org/10.3390/jcdd9030087
Harada T, Kagami K, Kato T, Ishii H, Obokata M. Exercise Stress Echocardiography in the Diagnostic Evaluation of Heart Failure with Preserved Ejection Fraction. Journal of Cardiovascular Development and Disease. 2022; 9(3):87. https://doi.org/10.3390/jcdd9030087
Chicago/Turabian StyleHarada, Tomonari, Kazuki Kagami, Toshimitsu Kato, Hideki Ishii, and Masaru Obokata. 2022. "Exercise Stress Echocardiography in the Diagnostic Evaluation of Heart Failure with Preserved Ejection Fraction" Journal of Cardiovascular Development and Disease 9, no. 3: 87. https://doi.org/10.3390/jcdd9030087
APA StyleHarada, T., Kagami, K., Kato, T., Ishii, H., & Obokata, M. (2022). Exercise Stress Echocardiography in the Diagnostic Evaluation of Heart Failure with Preserved Ejection Fraction. Journal of Cardiovascular Development and Disease, 9(3), 87. https://doi.org/10.3390/jcdd9030087