Tei Index Is a Useful Adjunctive Tool in the Diagnostic Workup of Patients with Acute Myocarditis
Abstract
:1. Introduction
2. Materials and Methods
2.1. Patients
2.2. Statistical Analysis
3. Results
3.1. Baseline Characteristics
3.2. Findings of Transthoracic Echocardiography (TTE)
3.3. ROC-Analysis and Cut-Offs
3.4. Binary Logistic Regression Analysis before Propensity Score Weighting
3.5. Propensity Weighted Logistic Regression Analysis
4. Discussion
5. Conclusions
6. Limitations
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Stepinska, J.; Lettino, M.; Ahrens, I.; Bueno, H.; Garcia-Castrillo, L.; Khoury, A.; Lancellotti, P.; Mueller, C.; Muenzel, T.; Oleksiak, A.; et al. Diagnosis and Risk Stratification of Chest Pain Patients in the Emergency Department: Focus on Acute Coronary Syndromes. A Position Paper of the Acute Cardiovascular Care Association. Eur. Heart J. Acute Cardiovasc. Care 2020, 9, 76–89. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Sagar, S.; Liu, P.P.; Cooper, L.T. Myocarditis. Lancet 2012, 379, 738–747. [Google Scholar] [CrossRef] [Green Version]
- Imazio, M.; Cooper, L.T. Management of Myopericarditis. Expert Rev. Cardiovasc. Ther. 2013, 11, 193–201. [Google Scholar] [CrossRef]
- Adler, Y.; Charron, P.; Imazio, M.; Badano, L.; Barón-Esquivias, G.; Bogaert, J.; Brucato, A.; Gueret, P.; Klingel, K.; Lionis, C.; et al. 2015 ESC Guidelines for the Diagnosis and Management of Pericardial Diseases. Eur. Heart J. 2015, 36, 2921–2964. [Google Scholar] [CrossRef] [PubMed]
- Ibanez, B.; James, S.; Agewall, S.; Antunes, M.J.; Bucciarelli-Ducci, C.; Bueno, H.; Caforio, A.L.P.; Crea, F.; Goudevenos, J.A.; Halvorsen, S.; et al. 2017 ESC Guidelines for the Management of Acute Myocardial Infarction in Patients Presenting with ST-Segment Elevation. Eur. Heart J. 2018, 39, 119–177. [Google Scholar] [CrossRef] [Green Version]
- Caforio, A.L.P.; Pankuweit, S.; Arbustini, E.; Basso, C.; Gimeno-Blanes, J.; Felix, S.B.; Fu, M.; Heliö, T.; Heymans, S.; Jahns, R.; et al. Current State of Knowledge on Aetiology, Diagnosis, Management, and Therapy of Myocarditis: A Position Statement of the European Society of Cardiology Working Group on Myocardial and Pericardial Diseases. Eur. Heart J. 2013, 34, 2636–2648, 2648a–2648d. [Google Scholar] [CrossRef] [PubMed]
- Bami, K.; Haddad, T.; Dick, A.; Dennie, C.; Dwivedi, G. Noninvasive Imaging in Acute Myocarditis. Curr. Opin. Cardiol. 2016, 31, 217–223. [Google Scholar] [CrossRef]
- Blauwet, L.A.; Cooper, L.T. Myocarditis. Prog. Cardiovasc. Dis. 2010, 52, 274–288. [Google Scholar] [CrossRef] [Green Version]
- Felker, G.M.; Boehmer, J.P.; Hruban, R.H.; Hutchins, G.M.; Kasper, E.K.; Baughman, K.L.; Hare, J.M. Echocardiographic Findings in Fulminant and Acute Myocarditis. J. Am. Coll. Cardiol. 2000, 36, 227–232. [Google Scholar] [CrossRef] [Green Version]
- Meindl, C.; Paulus, M.; Poschenrieder, F.; Zeman, F.; Maier, L.S.; Debl, K. Patients with Acute Myocarditis and Preserved Systolic Left Ventricular Function: Comparison of Global and Regional Longitudinal Strain Imaging by Echocardiography with Quantification of Late Gadolinium Enhancement by CMR. Clin. Res. Cardiol. 2021, 110, 1792–1800. [Google Scholar] [CrossRef]
- Matshela, M.R. The Role of Echocardiography in Acute Viral Myocarditis. Cardiovasc. J. Afr. 2019, 30, 239–244. [Google Scholar] [CrossRef] [PubMed]
- Cooper, L.T. Myocarditis. N. Engl. J. Med. 2009, 360, 1526–1538. [Google Scholar] [CrossRef] [Green Version]
- Tei, C.; Ling, L.H.; Hodge, D.O.; Bailey, K.R.; Oh, J.K.; Rodeheffer, R.J.; Tajik, A.J.; Seward, J.B. New Index of Combined Systolic and Diastolic Myocardial Performance: A Simple and Reproducible Measure of Cardiac Function—A Study in Normals and Dilated Cardiomyopathy. J. Cardiol. 1995, 26, 357–366. [Google Scholar]
- Harjai, K.J.; Scott, L.; Vivekananthan, K.; Nunez, E.; Edupuganti, R. The Tei Index: A New Prognostic Index for Patients with Symptomatic Heart Failure. J. Am. Soc. Echocardiogr. 2002, 15, 864–868. [Google Scholar] [CrossRef] [PubMed]
- Dujardin, K.S.; Tei, C.; Yeo, T.C.; Hodge, D.O.; Rossi, A.; Seward, J.B. Prognostic Value of a Doppler Index Combining Systolic and Diastolic Performance in Idiopathic-Dilated Cardiomyopathy. Am. J. Cardiol. 1998, 82, 1071–1076. [Google Scholar] [CrossRef]
- Bruch, C.; Schmermund, A.; Marin, D.; Katz, M.; Bartel, T.; Schaar, J.; Erbel, R. Tei-Index in Patients with Mild-to-Moderate Congestive Heart Failure. Eur. Heart J. 2000, 21, 1888–1895. [Google Scholar] [CrossRef] [PubMed]
- Ono, M.; Tanabe, K.; Asanuma, T.; Yoshitomi, H.; Shimizu, H.; Ohta, Y.; Shimada, T. Doppler Echocardiography-Derived Index of Myocardial Performance (TEI Index): Comparison with Brain Natriuretic Peptide Levels in Various Heart Disease. Jpn. Circ. J. 2001, 65, 637–642. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Keser, N.; Yildiz, S.; Kurtoǧlu, N.; Dindar, I. Modified TEI Index: A Promising Parameter in Essential Hypertension? Echocardiography 2005, 22, 296–304. [Google Scholar] [CrossRef]
- Mansour, H.; Nassar, A.; Abdel Rehim, W.; Roushdy, A.; Abobakr, M.; Zaki, H.; Aboubakr El Missiri, A. Can Tei Index Predict High Syntax Score in Patients with Chronic Coronary Syndrome and Normal Left Ventricular Systolic Function? J. Cardiovasc. Echogr. 2021, 31, 11–16. [Google Scholar] [CrossRef]
- Collet, J.-P.; Thiele, H.; Barbato, E.; Barthélémy, O.; Bauersachs, J.; Bhatt, D.L.; Dendale, P.; Dorobantu, M.; Edvardsen, T.; Folliguet, T.; et al. 2020 ESC Guidelines for the Management of Acute Coronary Syndromes in Patients Presenting without Persistent ST-Segment Elevation. Eur. Heart J. 2021, 42, 1289–1367. [Google Scholar] [CrossRef]
- Martínez-Camblor, P.; Pardo-Fernández, J.C. The Youden Index in the Generalized Receiver Operating Characteristic Curve Context. Int. J. Biostat. 2019, 15, 20180060. [Google Scholar] [CrossRef] [PubMed]
- Mccaffrey, D.F.; Griffin, B.A.; Almirall, D.; Slaughter, M.E.; Ramchand, R.; Burgette, L.F. A Tutorial on Propensity Score Estimation for Multiple Treatments Using Generalized Boosted Models. Stat. Med. 2013, 32, 3388–3414. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ogunmola, O.J.; Akintomide, A.O.; Olamoyegun, A.M. Relationship between Clinically Assessed Heart Failure Severity and the Tei Index in Nigerian Patients. BMC Res. Notes 2013, 6, 488. [Google Scholar] [CrossRef] [Green Version]
- Seyis, S. The Value of the Tei Index in Predicting Implantable Cardioverter Defibrillator Shocks. Med. Bull. Sisli Etfal Hosp. 2018, 52, 36. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Uzunhasan, I.; Bader, K.; Okçun, B.; Hatemi, A.C.; Mutlu, H. Correlation of the Tei Index with Left Ventricular Dilatation and Mortality in Patients with Acute Myocardial Infarction. Int. Heart J. 2006, 47, 331–342. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Bennett, S.; Wong, C.W.; Griffiths, T.; Stout, M.; Khan, J.N.; Duckett, S.; Heatlie, G.; Kwok, C.S. The Prognostic Value of Tei Index in Acute Myocardial Infarction: A Systematic Review. Echo. Res. Pract. 2020, 7, 49–58. [Google Scholar] [CrossRef]
- Yadav, D.K.; Choudhary, S.; Gupta, P.K.; Beniwal, M.K.; Agarwal, S.; Shukla, U.; Dubey, N.K.; Sankar, J.; Kumar, P. The Tei Index and Asymptomatic Myocarditis in Children with Severe Dengue. Pediatr. Cardiol. 2013, 34, 1307–1313. [Google Scholar] [CrossRef]


| Control (n = 50) | ACS (n = 29) | Myocarditis (n = 40) | |||||
|---|---|---|---|---|---|---|---|
| Median | IQR | Median | IQR | Median | IQR | p-Value | |
| Age (years) | 70 | 62–76 | 52 | 49–55 | 35 | 25–43 | <0.0001 |
| Serum creatinine (mg/dL) | 0.88 | 0.77–0.99 | 0.97 | 0.85–1.01 | 0.89 | 0.74–1.00 | 0.110 |
| C-reactive protein (mg/dL) | 0.20 | 0.10–0.43 | 0.20 | 0.10–1.00 | 2.35 | 0.68–6.18 | <0.0001 |
| High sensitivity troponin (hsTnT) (ng/L) | 14 | 11–21 | 244 | 80–681 | 375 | 135–862 | <0.0001 |
| Pro brain natriuretic peptide (pBNP) (ng/L) | 1034 | 254–2881 | 110 | 83–240 | 432 | 232–1090 | 0.006 |
| % | n | % | n | % | n | p-Value | |
| Male sex | 52.0 | 26 | 75.9 | 22 | 72.5 | 29 | 0.049 |
| Diabetes mellitus | 18.0 | 9 | 27.6 | 8 | 2.5 | 1 | 0.010 |
| Hyperlipidemia | 62.0 | 31 | 82.8 | 24 | 7.5 | 3 | <0.0001 |
| Obesity (BMI >30 kg/m²) | 29.8 | 14 | 37.9 | 11 | 12.5 | 5 | 0.047 |
| Arterial hypertension | 80.0 | 40 | 65.6 | 19 | 10.0 | 4 | <0.0001 |
| History of smoking | 50.0 | 22 | 55.2 | 16 | 17.5 | 7 | 0.001 |
| Control (n = 50) | ACS (n = 29) | Myocarditis (n = 40) | |||||
|---|---|---|---|---|---|---|---|
| Median | IQR | Median | IQR | Median | IQR | p-Value | |
| Ejection fraction (%) | 55 | 50–60 | 48 | 40–55 | 55 | 48–60 | 0.013 |
| IVSDd (mm) | 11 | 10–13 | 12 | 10–13 | 11 | 9–13 | 0.302 |
| LVEDd (mm) | 50 | 43–55 | 47 | 42–50 | 48 | 44–51 | 0.119 |
| E/e‘ | 11.3 | 8.3–14.1 | 10.0 | 8.1–11.9 | 8.6 | 7.0–10.0 | 0.041 |
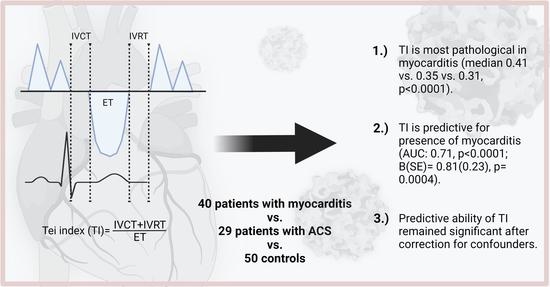
| TI | 0.31 | 0.23–0.36 | 0.35 | 0.30–0.44 | 0.41 | 0.35–0.48 | <0.0001 |
| B | SE | p-Value | |
|---|---|---|---|
| TI, z-score | 0.81 | 0.23 | 0.0004 |
| EF, z-score | 0.14 | 0.21 | 0.498 |
| E/e‘, z-score | −0.22 | 0.27 | 0.416 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Mirna, M.; Schmutzler, L.; Vogl, F.; Topf, A.; Hoppe, U.C.; Lichtenauer, M. Tei Index Is a Useful Adjunctive Tool in the Diagnostic Workup of Patients with Acute Myocarditis. J. Cardiovasc. Dev. Dis. 2022, 9, 283. https://doi.org/10.3390/jcdd9080283
Mirna M, Schmutzler L, Vogl F, Topf A, Hoppe UC, Lichtenauer M. Tei Index Is a Useful Adjunctive Tool in the Diagnostic Workup of Patients with Acute Myocarditis. Journal of Cardiovascular Development and Disease. 2022; 9(8):283. https://doi.org/10.3390/jcdd9080283
Chicago/Turabian StyleMirna, Moritz, Lukas Schmutzler, Fabian Vogl, Albert Topf, Uta C. Hoppe, and Michael Lichtenauer. 2022. "Tei Index Is a Useful Adjunctive Tool in the Diagnostic Workup of Patients with Acute Myocarditis" Journal of Cardiovascular Development and Disease 9, no. 8: 283. https://doi.org/10.3390/jcdd9080283
APA StyleMirna, M., Schmutzler, L., Vogl, F., Topf, A., Hoppe, U. C., & Lichtenauer, M. (2022). Tei Index Is a Useful Adjunctive Tool in the Diagnostic Workup of Patients with Acute Myocarditis. Journal of Cardiovascular Development and Disease, 9(8), 283. https://doi.org/10.3390/jcdd9080283