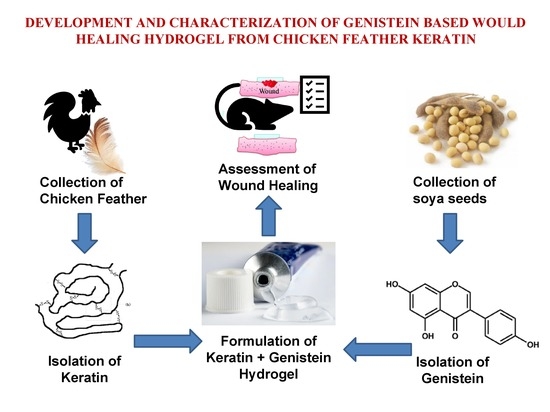
Innovative Wound Healing Hydrogel Containing Chicken Feather Keratin and Soy Isoflavone Genistein: In Vivo Studies
Abstract
:1. Introduction
2. Results and Discussion
2.1. Characterisation of Keratin
2.1.1. Protein Content
2.1.2. Amino Acid Profiling
2.1.3. Fourier-Transform Infrared (FT-IR) Spectroscopy
2.1.4. High-Performance Thin Layer Chromatography (HPTLC)
2.1.5. Scanning Electron Microscopy (SEM)
2.2. Characterisation of Genistein
High-Performance Thin Layer Chromatography (HPTLC)
2.3. Characterisation of Gel Formulations
2.3.1. General Characterisation
2.3.2. High-Performance Thin Layer Chromatography (HPTLC)
2.4. Stability Studies
2.5. Wound-Healing Activity
2.6. Histopathological Investigations
2.7. Biochemical Investigations
3. Conclusions
4. Material and Methods
4.1. Material
4.2. Extraction of Keratin from Chicken Feathers
4.3. Characterisation of Extracted Keratin
4.3.1. Protein Content
4.3.2. Amino Acid Analysis
4.3.3. Scanning Electron Microscopy (SEM)
4.3.4. Fourier-Transform Infrared (FT-IR) Spectroscopy
4.3.5. High-Performance Thin Layer Chromatography (HPTLC)
(a) For Keratin
(b) For Genistein
4.4. Characterisation of Genistein
4.5. Formulation Development (Gels)
4.5.1. Optimisation of Gel Base
4.5.2. Formulation Development of 2% Keratin Gel
4.5.3. Formulation Development of 1% Genistein Gel
4.5.4. Formulation Development of Keratin–Genistein Combination Gel
4.6. Characterisation of the Gel Formulation
4.6.1. Physical Evaluation
Gel Strength
pH
Viscosity
Spreadability
4.6.2. Keratin and Genistein Contents
4.6.3. HPTLC
4.6.4. Short-Term Stability Study
4.7. Animals
4.8. Wound Healing Study
4.9. Biochemical Analysis
4.9.1. Estimation of Cytokines by ELISA
4.9.2. qRT-PCR Analysis
4.10. Histopathological Investigations
4.11. Digital Image Analysis
4.12. Statistical Analysis
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Abbreviations
| TLC | Thin-Layer Chromatography |
| HPTLC | High-Performance Thin-Layer Chromatography |
| FTIR | Fourier-Transform Infrared Spectroscopy |
| SEM | Scanning Electron Microscopy |
| ELISA | Enzyme-Linked Immunoassay |
| qRT-PCR | Real-Time Quantitative Reverse Transcription PCR |
| IAEC | Institutional Animal Ethical Committee |
| CCSEA | Committee for Control and Supervision of Experiments on Animals |
| T-BHP | t-butylhydroperoxide |
| COX-2 | Cyclooxygenase-2 |
| IPQC | In-Process Quality Control |
References
- Guest, J.F.; Vowden, K.; Vowden, P. The health economic burden that acute and chronic wounds impose on an average clinical commissioning group/health board in the UK. J. Wound Care 2017, 26, 292–303. [Google Scholar] [CrossRef] [Green Version]
- Cheng, Q.; Gibb, M.; Graves, N.; Finlayson, K.; Pacella, R.E. Cost-effectiveness analysis of guideline-based optimal care for venous leg ulcers in Australia. BMC Health Serv. Res. 2018, 18, 421. [Google Scholar] [CrossRef]
- Olsson, M.; Järbrink, K.; Divakar, U.; Bajpai, R.; Upton, Z.; Schmidtchen, A.; Car, J. The humanistic and economic burden of chronic wounds: A systematic review. Wound Repair Regen. 2019, 27, 114–125. [Google Scholar] [CrossRef] [Green Version]
- Gray, T.A.; Rhodes, S.; Atkinson, R.; Rothwell, K.; Wilson, P.; Dumville, J.C.; Cullum, N. Opportunities for better value wound care: A multiservice, cross-sectional survey of complex wounds and their care in a UK community population. BMJ Open 2018, 8, e019440. [Google Scholar] [CrossRef] [Green Version]
- Casado-Díaz, A.; La Torre, M.; Priego-Capote, F.; Verdú-Soriano, J.; Lázaro-Martínez, J.L.; Rodríguez-Mañas, L.; Pérez, M.B.; Tunez, I. EHO-85: A Multifunctional Amorphous Hydrogel for Wound Healing Containing Olea europaea Leaf Extract: Effects on Wound Microenvironment and Preclinical Evaluation. J. Clin. Med. 2022, 11, 1229. [Google Scholar] [CrossRef] [PubMed]
- Pastar, I.; Stojadinovic, O.; Yin, N.C.; Ramirez, H.; Nusbaum, A.G.; Sawaya, A.; Patel, S.B.; Khalid, L.; Isseroff, R.R.; Tomic-Canic, M. Epithelialization in Wound Healing: A Comprehensive Review. Adv. Wound Care 2014, 3, 445–464. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Boateng, J.S.; Matthews, K.H.; Stevens, H.N.; Eccleston, G.M. Wound Healing Dressings and Drug Delivery Systems: A Review. J. Pharm. Sci. 2008, 97, 2892–2923. [Google Scholar] [CrossRef] [PubMed]
- Chattopadhyay, N.; Zastre, J.; Wong, H.-L.; Wu, X.Y.; Bendayan, R. Solid Lipid Nanoparticles Enhance the Delivery of the HIV Protease Inhibitor, Atazanavir, by a Human Brain Endothelial Cell Line. Pharm. Res. 2008, 25, 2262–2271. [Google Scholar] [CrossRef]
- Rouse, J.G.; Van Dyke, M.E. A Review of Keratin-Based Biomaterials for Biomedical Applications. Materials 2010, 3, 999–1014. [Google Scholar] [CrossRef] [Green Version]
- Khosa, M.A.; Ullah, A.J.J.F.P. A sustainable role of keratin biopolymer in green chemistry: A review. J. Food Process. Beverages 2013, 1, 8. [Google Scholar]
- Hill, P.; Brantley, H.; Van Dyke, M. Some properties of keratin biomaterials: Kerateines. Biomaterials 2010, 31, 585–593. [Google Scholar] [CrossRef]
- Kumaran, P.; Gupta, A.; Sharma, S. Synthesis of wound-healing keratin hydrogels using chicken feathers proteins and its properties. Int. J. Pharm. Pharm. Sci. 2017, 9, 171–178. [Google Scholar] [CrossRef] [Green Version]
- Ar, B.; Choudhury, K. Study on the Effect of Genistein, a Soy Isoflavone in Insulin Tolerance in Albino Rat (Rattus albicans). Sch. Acad. J. Biosci. 2018, 6, 366–371. [Google Scholar]
- Emmerson, E.; Campbell, L.; Ashcroft, G.S.; Hardman, M.J. The phytoestrogen genistein promotes wound healing by multiple independent mechanisms. Mol. Cell. Endocrinol. 2010, 321, 184–193. [Google Scholar] [CrossRef]
- Duchnik, E.; Kruk, J.; Baranowska-Bosiacka, I.; Pilutin, A.; Maleszka, R.; Marchlewicz, M. Effects of the soy isoflavones, genistein and daidzein, on male rats’ skin. Adv. Dermatol. Allergol. 2019, 36, 760–766. [Google Scholar] [CrossRef] [PubMed]
- Marini, H.R.; Polito, F.; Altavilla, D.; Irrera, N.; Minutoli, L.; Calò, M.; Adamo, E.B.; Vaccaro, M.; Squadrito, F.; Bitto, A. Genistein aglycone improves skin repair in an incisional model of wound healing: A comparison with raloxifene and oestradiol in ovariectomized rats. Br. J. Pharmacol. 2010, 160, 1185–1194. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Emmerson, E.; Hardman, M.J. The role of estrogen deficiency in skin ageing and wound healing. Biogerontology 2012, 13, 3–20. [Google Scholar] [CrossRef] [PubMed]
- Rohrmann, S.; Shvetsov, Y.B.; Morimoto, Y.; Wilkens, L.R.; Monroe, K.R.; Le Marchand, L.; Franke, A.A.; Kolonel, L.N.; Maskarinec, G. Self-reported dietary flavonoid intake and serum markers of inflammation: The multiethnic cohort. Cancer Causes Control 2018, 29, 601–607. [Google Scholar] [CrossRef] [Green Version]
- Irrera, N.; Pizzino, G.; D’anna, R.; Vaccaro, M.; Arcoraci, V.; Squadrito, F.; Altavilla, D.; Bitto, A. Dietary Management of Skin Health: The Role of Genistein. Nutrients 2017, 9, 622. [Google Scholar] [CrossRef] [Green Version]
- Hwang, K.; Chung, R.S.; Schmitt, J.M.; Buck, D.; Winn, S.R.; Hollinger, J.O. The Effect of Topical Genistein on Soft Tissue Wound Healing in Rats. J. Histotechnol. 2001, 24, 95–99. [Google Scholar] [CrossRef]
- Cooke, P.S.; Selvaraj, V.; Yellayi, S. Genistein, estrogen receptors, and the acquired immune response. J. Nutr. 2006, 136, 704–708. [Google Scholar] [CrossRef] [Green Version]
- Sinkiewicz, I.; Śliwińska, A.; Staroszczyk, H.; Kołodziejska, I. Alternative Methods of Preparation of Soluble Keratin from Chicken Feathers. Waste Biomass Valorization 2017, 8, 1043–1048. [Google Scholar] [CrossRef]
- Sadowska-Krowicka, H.; Mannick, E.E.; Oliver, P.D.; Sandoval, M.; Zhang, X.-J.; Eloby-Childess, S.; Clark, D.A.; Miller, M.J.S. Genistein and Gut Inflammation: Role of Nitric Oxide. Proc. Soc. Exp. Boil. Med. 1998, 217, 351–357. [Google Scholar] [CrossRef] [PubMed]
- Kharwade, R.; Ali, N.; Gangane, P.; Pawar, K.; More, S.; Iqbal, M. DOE-Assisted Formulation, Optimization, and Characterization of Tioconazole-Loaded Transferosomal Hydrogel for the Effective Treatment of Atopic Dermatitis: In Vitro and In Vivo Evaluation. Gels 2023, 9, 303. [Google Scholar] [CrossRef] [PubMed]
- Seibel, J.; Molzberger, A.F.; Hertrampf, T.; Laudenbach-Leschowski, U.; Diel, P. Oral treatment with genistein reduces the expression of molecular and biochemical markers of inflammation in a rat model of chronic TNBS-induced colitis. Eur. J. Nutr. 2009, 48, 213–220. [Google Scholar] [CrossRef] [PubMed]
- Kharwade, R.S.; Mahajan, N.M. Formulation and Evaluation of Nanostructured Lipid Carriers Based Anti-Inflammatory Gel for Topical Drug Delivery System. Asian J. Pharm. Clin. Res. 2019, 12, 286–291. [Google Scholar] [CrossRef]
- Tie, L.; An, Y.; Han, J.; Xiao, Y.; Xiaokaiti, Y.; Fan, S.; Liu, S.; Chen, A.F.; Li, X. Genistein accelerates refractory wound healing by suppressing superoxide and FoxO1/iNOS pathway in type 1 diabetes. J. Nutr. Biochem. 2013, 24, 88–96. [Google Scholar] [CrossRef]
- Stipcevic, T.; Piljac, A.; Piljac, G. Enhanced healing of full-thickness burn wounds using di-rhamnolipid. Burns 2006, 32, 24–34. [Google Scholar] [CrossRef] [Green Version]
- Woods, A. Syndecans: Transmembrane modulators of adhesion and matrix assembly. J. Clin. Investig. 2001, 107, 935–941. [Google Scholar] [CrossRef] [Green Version]
- Greene, D.K.; Tumova, S.; Couchman, J.R.; Woods, A. Syndecan-4 Associates with α-Actinin. J. Biol. Chem. 2003, 278, 7617–7623. [Google Scholar] [CrossRef] [Green Version]
- Diegelmann, R.F.; Cohen, I.K.; Kaplan, A.M. The Role of Macrophages in Wound Repair: A review. Plast. Reconstr. Surg. 1981, 68, 107–113. [Google Scholar] [CrossRef]
- Gupta, A.; Perumal, R.; Yunus, R.B.M.; Kamarudin, N.B. Extraction of keratin protein from chicken feather. J. Chem. Chem. Eng. 2011, 6, 732. [Google Scholar]
- Šafarič, R.; Zemljič, L.F.; Novak, M.; Dugonik, B.; Bratina, B.; Gubeljak, N.; Bolka, S.; Strnad, S. Preparation and Characterisation of Waste Poultry Feathers Composite Fibreboards. Materials 2020, 13, 4964. [Google Scholar] [CrossRef]
- Wang, H.; Pampati, N.; McCormick, W.M.; Bhattacharyya, L. Protein Nitrogen Determination by Kjeldahl Digestion and Ion Chromatography. J. Pharm. Sci. 2016, 105, 1851–1857. [Google Scholar] [CrossRef] [PubMed]
- Fekkes, D.; van Dalen, A.; Edelman, M.; Voskuilen, A. Validation of the determination of amino acids in plasma by high-performance liquid chromatography using automated pre-column derivatization with o-phthaldialdehyde. J. Chromatogr. B Biomed. Sci. Appl. 1995, 669, 177–186. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Blackburn, S.; Lowther, A.G. The action of organic acids on some fibrous proteins: The oxidation of wool keratin. Biochem. J. 1951, 49, 554–559. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Elhawary, Y.; Badria, F. Mode of Action of Centella Asiatica in Wound Healing Using Immunohistochemical Studies. Egypt. Dent. J. 2011, 57, 1. [Google Scholar]
- Ullah, N.; Amin, A.; Farid, A.; Selim, S.; Rashid, S.A.; Aziz, M.I.; Kamran, S.H.; Khan, M.A.; Khan, N.R.; Mashal, S.; et al. Development and Evaluation of Essential Oil-Based Nanoemulgel Formulation for the Treatment of Oral Bacterial Infections. Gels 2023, 9, 252. [Google Scholar] [CrossRef]
- Jia, Z.; Babu, P.V.A.; Si, H.; Nallasamy, P.; Zhu, H.; Zhen, W.; Misra, H.P.; Li, Y.; Liu, D. Genistein inhibits TNF-α-induced endothelial inflammation through the protein kinase pathway A and improves vascular inflammation in C57BL/6 mice. Int. J. Cardiol. 2013, 168, 2637–2645. [Google Scholar] [CrossRef] [Green Version]
- Fule, R.; Kaleem, M.; Asar, T.O.; Rashid, A.; Shaik, R.A.; Eid, B.G.; Nasrullah, M.Z.; Ahmad, A.; Kazmi, I. Formulation, Optimization and Evaluation of Cytarabine-Loaded Iron Oxide Nanoparticles: From In Vitro to In Vivo Evaluation of Anticancer Activity. Nanomaterials 2023, 13, 175. [Google Scholar] [CrossRef]
- Omer, A.B.; Dalhat, M.H.; Khan, M.K.; Afzal, O.; Altamimi, A.S.A.; Alzarea, S.I.; Almalki, W.H.; Kazmi, I. Butin Mitigates Memory Impairment in Streptozotocin-Induced Diabetic Rats by Inhibiting Oxidative Stress and Inflammatory Responses. Metabolites 2022, 12, 1050. [Google Scholar] [CrossRef]
- Bahramsoltani, R.; Farzaei, M.H.; Rahimi, R. Medicinal plants and their natural components as future drugs for the treatment of burn wounds: An integrative review. Arch. Dermatol. Res. 2014, 306, 601–617. [Google Scholar] [CrossRef] [PubMed]
- Midwood, K.S.; Williams, L.V.; Schwarzbauer, J.E. Tissue repair and the dynamics of the extracellular matrix. Int. J. Biochem. Cell Biol. 2004, 36, 1031–1037. [Google Scholar] [CrossRef]
- Singh, A.K.; Bhadauria, A.S.; Kumar, U.; Raj, V.; Rai, A.; Kumar, P.; Keshari, A.K.; Kumar, D.; Maity, B.; Nath, S.; et al. Novel Indole-fused benzo-oxazepines (IFBOs) inhibit invasion of hepatocellular carcinoma by targeting IL-6 mediated JAK2/STAT3 oncogenic signals. Sci. Rep. 2018, 8, 5932. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Park, E.; Lee, S.M.; Jung, I.-K.; Lim, Y.; Kim, J.-H. Effects of genistein on early-stage cutaneous wound healing. Biochem. Biophys. Res. Commun. 2011, 410, 514–519. [Google Scholar] [CrossRef]
- Alghamdi, R.M.; Hassan, M.A.; Kaleem, M.; Kayali, A.; Halwani, M.A.; Zamzami, M.A.; Choudhry, H.; Alhosin, M. Targeting Itch/p73 pathway by thymoquinone as a novel therapeutic strategy for cancers with p53 mutation. Eur. J. Cell Sci. 2020, 2, 20–26. [Google Scholar] [CrossRef]
- Al Khalaf, A.K.; Abdulrahman, A.O.; Kaleem, M.; Nur, S.M.; Asseri, A.H.; Choudhry, H.; Khan, M.I. Comparative Analysis of the Impact of Urolithins on the Composition of the Gut Microbiota in Normal-Diet Fed Rats. Nutrients 2021, 13, 3885. [Google Scholar] [CrossRef] [PubMed]
- Kaleem, M.; Haque, S.E. Evaluation of Cardioprotective Role of Vinpocetine in Isoproterenolinduced Myocardial Infarction in Rats. J. Pharm. Res. 2015, 9, 408–414. Available online: https://www.researchgate.net/publication/342480421_Evaluation_of_Cardioprotective_role_of_Vinpocetine_in_Isoproterenol-induced_Myocardial_Infarction_in_Rats (accessed on 29 November 2021).









| Test Parameter | Test Unit (g/100 g) | Reference Range (g/100 g) |
|---|---|---|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
| Peak | Start Position (Rf) | Start Height (AU) | Max Position (Rf) | Max Height (AU) | Max % | End Position (Rf) | End Height (AU) | Area (AU) | Area % |
|---|---|---|---|---|---|---|---|---|---|
| Keratin extract and keratin gel formulation | |||||||||
| 3 | 0.62 | 6.5 | 0.63 | 12.8 | 2.52 | 0.64 | 0.4 | 90.3 | 0.57 |
| 7 | 0.62 | 7.7 | 0.63 | 18.9 | 3.54 | 0.65 | 6.4 | 159.5 | 0.95 |
| Genistein extract and genistein gel formulation | |||||||||
| 6 | 0.56 | 42.9 | 0.56 | 49.2 | 8.81 | 0.60 | 38.7 | 802.0 | 11.03 |
| 5 | 0.48 | 26.8 | 0.50 | 41.4 | 13.37 | 0.51 | 25.6 | 448.2 | 13.34 |
| Keratin, genistein extract and keratin, genistein combination gel (Mobile Phase: butanol: acetic acid: water) | |||||||||
| 10 | 0.56 | 3.5 | 0.58 | 14.3 | 2.33 | 0.60 | 9.8 | 175.0 | 1.46 |
| 9 | 0.49 | 5.9 | 0.51 | 13.0 | 2.35 | 0.55 | 1.2 | 135.9 | 1.78 |
| Keratin, genistein extract and keratin, genistein combination gel (Mobile Phase: chloroform: methanol) | |||||||||
| 4 | 0.73 | 21.3 | 0.74 | 27.7 | 6.09 | 0.75 | 19.5 | 279.2 | 3.68 |
| 8 | 0.68 | 15.2 | 0.70 | 25.4 | 7.02 | 0.72 | 14.2 | 271.8 | 4.87 |
| Gel Type | Gel Strength (Sec) | Drug Content Mean ± SD | pH Mean ± SD | Viscosity (Cps) Mean ± SD | Spreadability (gm·cm/s) Mean ± SD | |||
|---|---|---|---|---|---|---|---|---|
| Pre-Stability | Post-Stability | Pre-Stability | Post-Stability | Pre-Stability | Post-Stability | |||
| Keratin gel | 4 | 96.07 ± 0.7214 | 7.6 ± 0.15 | 6.8 ± 0.15 | 470,913 ± 1978.7 | 433,342 ± 9495.1 | 9.78 ± 1.0 | 8.4 ± 0.85 |
| Genistein gel | 3 | 91.89 ± 0.2134 | 6.8 ± 0.1 | 6.4 ± 0.20 | 738,063 ± 2411.4 | 706,920 ± 1126.8 | 14 ± 1.4 | 13.65 ± 0.63 |
| Keratin–Genistein gel | 4 | 93.21 ± 0.764 (Keratin) 92.79 ± 0.7543 (Genistein) | 7.2 ± 0.2 | 6.5 ± 0.26 | 714,547.53 ± 3040.3 | 700,446 ± 6777.86 | 12.56 ± 0.92 | 10.83 ± 1.2 |
| Formulation | pH Mean ± SD | Viscosity (cPs) Mean ± SD | Spreadability (gm·cm/s) Mean ± SD | |||
|---|---|---|---|---|---|---|
| 0 Days | 90 Days | 0 Days | 90 Days | 0 Days | 90 Days | |
| Keratin gel | 7.6 ± 0.15 | 6.8 ± 0.15 | 470,913 ± 19,787.5 | 433,342 ± 9495.15 | 9.78 ± 1.0 | 8.4 ± 0.85 |
| Genistein gel | 6.8 ± 0.1 | 6.4 ± 0.20 | 738,063 ± 24,114.7 | 706,920 ± 11,268.6 | 14 ± 1.4 | 13.65 ± 0.63 |
| Keratin-Genistein gel | 7.2 ± 0.2 | 6.5 ± 0.26 | 714,547.53 ± 30,403.9 | 700,446 ± 6777.86 | 12.56 ± 0.92 | 10.83 ± 1.2 |
| Groups | Day 7 (% Wound Healing) Mean ± SD | Day 14 (% Wound Healing) Mean ± SD |
|---|---|---|
| Keratin gel | 54.29 ± 4.170 | 87.57 ± 5.00 |
| Genistein gel | 48.51 ± 7.88 | 87.40 ± 3.57 |
| Keratin and genistein combination gel | 51.18 ± 2.043 | 94.65 ± 4.64 |
| Standard gel | 54.99 ± 13.63 | 96.66 ± 5.77 |
| Control | 48.15 ± 9.32 | 85.98 ± 3.53 |
| Parameters | NC | WC | PC | Keratin | Genistein | Keratin and Genistein |
|---|---|---|---|---|---|---|
| COX-2 (pg/mL) | 188.78 ± 8.09 | 449.24 ± 12.95 | 210.84 ± 10.51 *** | 240.97 ± 8.46 *** | 223.79 ± 11.49 *** | 196.25 ± 9.61 *** |
| IL-2 (pg/mL) | 492.27 ± 12.03 | 1103.32 ± 19.37 | 594.38 ± 12.45 *** | 620.31 ± 16.85 *** | 601.76 ± 18.17 *** | 519.37 ± 11.51 *** |
| IL-6 (pg/mL) | 148.91 ± 4.61 | 327.94 ± 8.16 | 179.24 ± 5.34 *** | 204.37 ± 9.17 *** | 191.38 ± 7.42 *** | 163.84 ± 7.19 *** |
| IL-10 (pg/mL) | 630.94 ± 20.37 | 1294.01 ± 25.79 | 764.85 ± 23.14 *** | 804.59 ± 22.67 *** | 789.41 ± 11.64 *** | 681.93 ± 9.43 *** |
| IL1-β (pg/mL) | 552.37 ± 18.19 | 1109.86 ± 24.17 | 624.87 ± 12.37 *** | 655.49 ± 11.27 *** | 634.59 ± 9.73 *** | 611.48 ± 10.70 *** |
| 2% KERATIN GEL | 1% GENISTEIN GEL | KERATIN–GENISTEIN GEL | |||
|---|---|---|---|---|---|
| Ingredients | Quantity | Ingredients | Quantity | Ingredients | Quantity |
| Carbopol 934 | 1% w/v | Carbopol 934 | 1% w/v | Carbopol 934 | 1% w/v |
| Keratin | 1 g | Genistein | 0.5 g | Keratin | 1 g |
| Cremophor RH 40 | 3 mL | Methyl paraben | 0.01 g | Genistein | 0.5 g |
| Methyl Paraben | 0.01 g | Propyl paraben | 0.01 g | Cremophor RH 40 | 3 mL |
| Propyl Paraben | 0.01 g | Triethanolamine | q.s. | Methyl paraben | 0.01 g |
| Triethanolamine | q.s. | Propyl paraben | 0.01 g | ||
| Triethanolamine | q.s. | ||||
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Mahajan, N.M.; Wanaskar, K.; Ali, N.; Mahapatra, D.K.; Iqbal, M.; Bhat, A.R.; Kaleem, M. Innovative Wound Healing Hydrogel Containing Chicken Feather Keratin and Soy Isoflavone Genistein: In Vivo Studies. Gels 2023, 9, 462. https://doi.org/10.3390/gels9060462
Mahajan NM, Wanaskar K, Ali N, Mahapatra DK, Iqbal M, Bhat AR, Kaleem M. Innovative Wound Healing Hydrogel Containing Chicken Feather Keratin and Soy Isoflavone Genistein: In Vivo Studies. Gels. 2023; 9(6):462. https://doi.org/10.3390/gels9060462
Chicago/Turabian StyleMahajan, Nilesh M., Kalyani Wanaskar, Nemat Ali, Debarshi Kar Mahapatra, Muzaffar Iqbal, Abid R. Bhat, and Mohammed Kaleem. 2023. "Innovative Wound Healing Hydrogel Containing Chicken Feather Keratin and Soy Isoflavone Genistein: In Vivo Studies" Gels 9, no. 6: 462. https://doi.org/10.3390/gels9060462
APA StyleMahajan, N. M., Wanaskar, K., Ali, N., Mahapatra, D. K., Iqbal, M., Bhat, A. R., & Kaleem, M. (2023). Innovative Wound Healing Hydrogel Containing Chicken Feather Keratin and Soy Isoflavone Genistein: In Vivo Studies. Gels, 9(6), 462. https://doi.org/10.3390/gels9060462