Systemic Manifestations and Complications of Rheumatoid Arthritis
A topical collection in Journal of Clinical Medicine (ISSN 2077-0383). This collection belongs to the section "Immunology".
Viewed by 80922Editor
Interests: rheumatoid arthritis; systemic lupus erythematosus; autoimmunity; osteoporosis; biomarker; targeted treatment
Topical Collection Information
Dear Colleagues,
Rheumatoid arthritis (RA) is a systemic autoimmune disease predominantly involving small joints and causing joint deformity and functional loss. In addition, systemic manifestations, such as pulmonary, cardiovascular, and neurologic involvement, are commonly developed in RA patients with severe inflammation or long-standing disease duration. With adequate treatment to control inflammation, some of these complications of RA can be prevented. However, the treatment of RA also produces complications, such as cardiovascular, musculosketal, infectious, and neurologic problems. The knowledge of these complications as they develop in patients with RA is important in order to enable prevention and treatment. The Special Issue on “Systemic Manifestations and Complications of Rheumatoid Arthritis” is now open to your contributions. We look forward to your work on the diagnostic, preventive, and therapeutic aspect of various complications in patients with RA.
Prof. Dr. Chang-Hee Suh
Guest Editor
Manuscript Submission Information
Manuscripts should be submitted online at www.mdpi.com by registering and logging in to this website. Once you are registered, click here to go to the submission form. Manuscripts can be submitted until the deadline. All submissions that pass pre-check are peer-reviewed. Accepted papers will be published continuously in the journal (as soon as accepted) and will be listed together on the collection website. Research articles, review articles as well as short communications are invited. For planned papers, a title and short abstract (about 100 words) can be sent to the Editorial Office for announcement on this website.
Submitted manuscripts should not have been published previously, nor be under consideration for publication elsewhere (except conference proceedings papers). All manuscripts are thoroughly refereed through a single-blind peer-review process. A guide for authors and other relevant information for submission of manuscripts is available on the Instructions for Authors page. Journal of Clinical Medicine is an international peer-reviewed open access semimonthly journal published by MDPI.
Please visit the Instructions for Authors page before submitting a manuscript. The Article Processing Charge (APC) for publication in this open access journal is 2600 CHF (Swiss Francs). Submitted papers should be well formatted and use good English. Authors may use MDPI's English editing service prior to publication or during author revisions.
Keywords
- Rheumatoid arthritis
- Complications of treatment
- Osteoporosis and fracture
- Glucocorticoid-induced osteoporosis
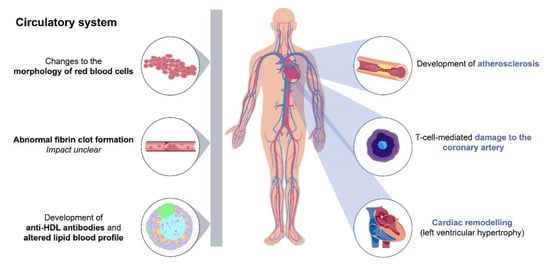
- Cardiovascular disease
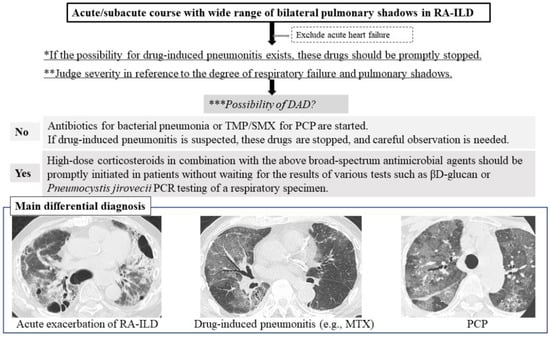
- Lung involvement
- Infection
- Neurologic complication