Radiation Oncology
A topical collection in Lymphatics (ISSN 2813-3307).
Viewed by 7662Editors
Interests: radiation oncology; hematology
Special Issues, Collections and Topics in MDPI journals
Interests: Hodgkin's lymphoma; non-Hodgkin's lymphoma; radiation oncology
Interests: follicular lymphoma; marginal zone lymphoma; diffuse large B-cell lymphoma; immunotherapy; cellular therapy
Special Issues, Collections and Topics in MDPI journals
Interests: radiation oncology
Interests: radiation therapy; lymphoma
Special Issues, Collections and Topics in MDPI journals
Interests: acute lymphoblastic leukemia; acute myeloid leukemia; measurable residual disease
Special Issues, Collections and Topics in MDPI journals
Topical Collection Information
Dear Colleagues,
The aim of this Collection of the journal Lymphatics is to enable rapid publications of scientific contributions and discoveries in the field of radiation oncology in reference to hematological malignancies.
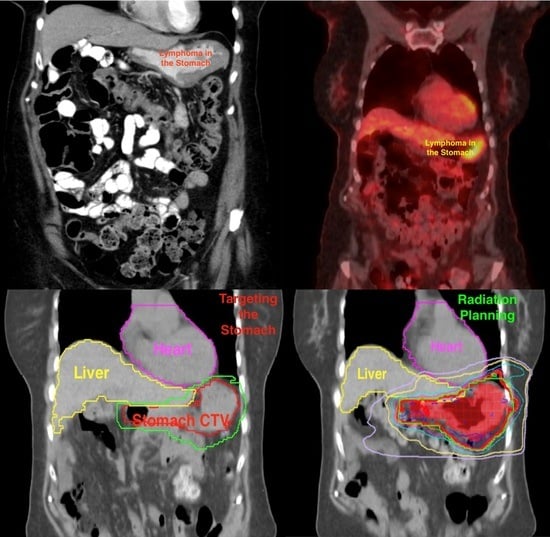
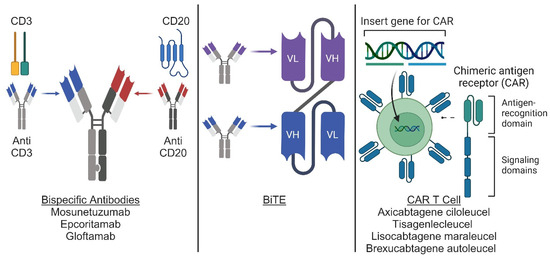
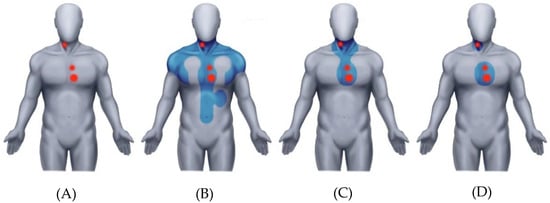
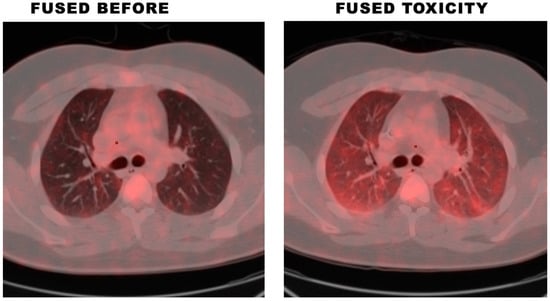
Over the past five decades, the role and application of radiation therapy have dramatically changed, leading to 1) a reduction in the radiation fields and doses to mitigate the long-term toxicities seen when using outdated radiation; 2) the introduction of new indications for radiation treatment, 3) and most importantly, the employment of the radiation ability to produce immunogenic cell death, facilitating its introduction into the environment of immunotherapy and cellular therapy.
Topics include, but are not limited to:
- Radiation techniques
- Motion control management
- Applications of radiation fields and dose
- Mitigating radiation toxicity
- Radiation as consolidation post systemic therapy
- Combined modality with radiation and chemotherapy
- Combined radiation and immunotherapy
- Radiation as a conditioning prior to stem cell transplant
- Radiation as bridging in the cellular therapy environment
- Novel indications for radiation use
- Mechanisms of radiation induced immunogenicity
- Radiation in the palliative setting
We also welcome reviews on these subjects, particularly those that challenge existing concepts.
Prof. Dr. Bouthaina S. Dabaja
Prof. Dr. Andrea K. Ng
Dr. Paolo Strati
Dr. Michael T. Spiotto
Prof. Dr. Hans Theodor Eich
Dr. Nicholas J. Short
Prof. Dr. N. George Mikhaeel
Collection Editors
Manuscript Submission Information
Manuscripts should be submitted online at www.mdpi.com by registering and logging in to this website. Once you are registered, click here to go to the submission form. Manuscripts can be submitted until the deadline. All submissions that pass pre-check are peer-reviewed. Accepted papers will be published continuously in the journal (as soon as accepted) and will be listed together on the collection website. Research articles, review articles as well as short communications are invited. For planned papers, a title and short abstract (about 100 words) can be sent to the Editorial Office for announcement on this website.
Submitted manuscripts should not have been published previously, nor be under consideration for publication elsewhere (except conference proceedings papers). All manuscripts are thoroughly refereed through a single-blind peer-review process. A guide for authors and other relevant information for submission of manuscripts is available on the Instructions for Authors page. Lymphatics is an international peer-reviewed open access quarterly journal published by MDPI.
Please visit the Instructions for Authors page before submitting a manuscript. The Article Processing Charge (APC) for publication in this open access journal is 1000 CHF (Swiss Francs). Submitted papers should be well formatted and use good English. Authors may use MDPI's English editing service prior to publication or during author revisions.