Advances in the Pathogenesis of Neurodegenerative Diseases
A topical collection in Medical Sciences (ISSN 2076-3271). This collection belongs to the section "Neurosciences".
Viewed by 50630Editor
Interests: multiple sclerosis; neurodegenerative diseases; serum biomarkers; neuroimaging
Special Issues, Collections and Topics in MDPI journals
Topical Collection Information
Dear Colleagues,
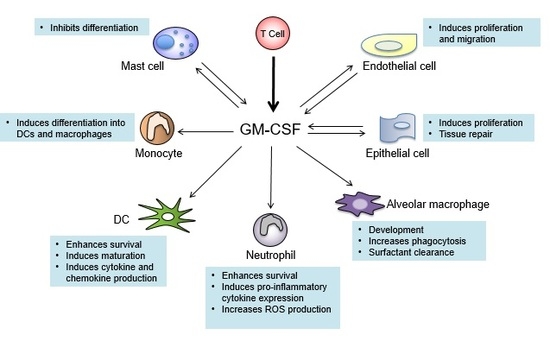
The term “Neurodegenerative Diseases” (NDDs) identifies a heterogeneous group of disorders characterized by progressive degeneration of the structure and function of the central or peripheral nervous systems. The evidence of common features, represented, e.g., by intracellular accumulation and aggregation of misfolded proteins, abnormal cellular transport and mitochondrial deficits, suggest converging pathogenic pathways that lead to neurodegeneration. Quite recently, inflammation has been confirmed as another essential contributing factor, in which reactive astroglia and/or microglia seem to play key roles.
Despite the current knowledge, at present, the whole picture of neurodegeneration is still missing. Furthermore, besides well-known degenerative disorders like Alzheimer's, Parkinson's, Huntington's diseases and Amyotrophic Lateral Sclerosis, a crucial neurodegenerative component has been recognized, e.g., in inflammatory demyelinating diseases like Multiple Sclerosis, thus representing a significant piece of the puzzle in their characterization, which may narrow a more successful therapeutic window. Another important consideration concerns the wide heterogeneity of clinical or instrumental (e.g., neuroradiological) phenotypes in most of NDDs that may explain the sometimes-different response to treatment of each patient.
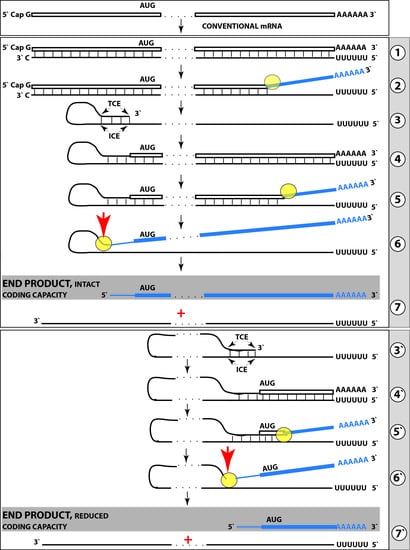
A fundamental support for the possible solution of these different issues is represented by the use of innovative extensive approaches in the molecular analysis like massive high-throughput sequencing (DNA, RNA) and proteomics that allowed to show the involvement of multiple cellular pathways in a given pathogenic process. As examples, transcriptomics studies showed that misregulated microRNAs (miRNAs, endogenous small RNAs binding the target sites of protein-coding genes, which lead to their degradation or the repression of translation) seem to justify several neurodegenerative processes, suggesting that alterations in miRNA regulatory pathways may contribute significantly to NDDs pathogenesis. Considering the growing interest in the potential of miRNAs, it is also plausible that these findings may lead to develop miRNAs therapeutics also for NDDs.
To our view, understanding the interplay of these (and others) key factors (i.e., extracellular vesicles and their cargos) may be of invaluable help in the effort of shedding lights on these still progressive and irreversible processes.
On these grounds, the big challenge of this Special Issue is to further explore the novel molecular hypotheses that underline the degenerative features of NDDs, in order: 1) to better define their pathogenic processes; 2) to picture peculiar molecular profiles of clinical/instrumental phenotypes; 3) to possibly identify early circulating biomarkers of clinical prognosis and treatment efficacy. The final goal of this approach will be to possibly offer suggestions for controlling the diseases and their progression, thus avoiding the irreversible and dramatic events of more advanced conditions. This will lead to more attention regarding the patient's quality of life, by promoting treatment plans based on the individual molecular signature (i.e.: the most effective dose with least side effects), a fundamental step towards the implementation of so-called Personalized Medicine.
Dr. Maria Liguori
Guest Editor
Manuscript Submission Information
Manuscripts should be submitted online at www.mdpi.com by registering and logging in to this website. Once you are registered, click here to go to the submission form. Manuscripts can be submitted until the deadline. All submissions that pass pre-check are peer-reviewed. Accepted papers will be published continuously in the journal (as soon as accepted) and will be listed together on the collection website. Research articles, review articles as well as short communications are invited. For planned papers, a title and short abstract (about 100 words) can be sent to the Editorial Office for announcement on this website.
Submitted manuscripts should not have been published previously, nor be under consideration for publication elsewhere (except conference proceedings papers). All manuscripts are thoroughly refereed through a single-blind peer-review process. A guide for authors and other relevant information for submission of manuscripts is available on the Instructions for Authors page. Medical Sciences is an international peer-reviewed open access quarterly journal published by MDPI.
Please visit the Instructions for Authors page before submitting a manuscript. The Article Processing Charge (APC) for publication in this open access journal is 1400 CHF (Swiss Francs). Submitted papers should be well formatted and use good English. Authors may use MDPI's English editing service prior to publication or during author revisions.
Keywords
Neurodegenerative diseases
- Neurobiology
- Extracellular vesicles
- Massive high-throughput sequencing (DNA, RNA)
- Non-coding RNAs, gene targets
- Molecular pathways
- Circulating biomarkers of diseases
- Phenotype Biomarkers
- Biomarkers of treatment efficacy