Synthesis and Protective Effect of New Ligustrazine-Benzoic Acid Derivatives against CoCl2-Induced Neurotoxicity in Differentiated PC12 Cells
Abstract
:1. Introduction
2. Results and Discussion
2.1. Chemistry


| Structure | Yield | Structure | Yield |
|---|---|---|---|
 | 61.1% |  | 85.1% |
| 1a | 1b | ||
 | 64.0% |  | 47.6% |
| 1c | 1d | ||
 | 61.7% |  | 81.9% |
| 2a | 2b | ||
 | 64.4% |  | 52.6% |
| 2c | 2d | ||
 | 61.7% |  | 89.7% |
| 3a | 3b | ||
 | 63.2% |  | 60.1% |
| 3c | 3d | ||
 | 62.5% |  | 87.4% |
| 4a | 4b | ||
 | 67.5% |  | 54.7% |
| 4c | 4d | ||
 | 58.4% |  | 87.1% |
| 5a | 5b | ||
 | 51.2% |  | 54.7% |
| 5c | 5d |
2.2. Biological Activities
2.2.1. Protective Effect on Injured Neuronal-like PC12 Cells
| Compound | Proliferation rate (%) | EC50 (µM) | ||||
|---|---|---|---|---|---|---|
| 60 µM | 30 µM | 15 µM | 7.5 µM | 3.75 µM | ||
| 1a | 61.63 | 58.87 | 27.69 | 18.97 | 4.58 | 27.359 |
| 2a | 16.27 | 25.49 | 27.48 | 33.71 | 15.65 | 40.715 |
| 3a | 81.60 | 77.58 | 64.50 | 32.08 | 30.07 | 11.467 |
| 4a | 126.60 | 117.10 | 89.76 | 52.98 | 31.12 | 4.249 |
| 5a | 47.14 | 36.44 | 36.01 | −7.22 | −5.94 | 45.029 |
| 1b | 5.50 | 32.37 | −1.76 | −8.25 | −16.00 | 90.345 |
| 2b | 16.91 | 27.96 | 6.99 | −22.43 | −22.76 | 95.484 |
| 3b | 27.30 | 46.91 | 33.84 | 11.21 | 6.44 | 38.493 |
| 4b | 6.29 | 10.84 | −2.28 | −10.40 | −10.73 | >100 |
| 5b | 27.14 | 0.47 | −0.08 | −3.71 | −5.67 | 85.723 |
| 1c | 21.88 | 21.67 | 19.32 | −1.87 | −17.07 | 73.801 |
| 2c | 55.78 | 90.74 | 96.07 | 72.74 | 58.09 | 5.828 |
| 3c | 57.72 | 18.75 | 9.20 | 22.27 | −1.86 | 43.909 |
| 4c | 9.18 | 12.54 | 14.28 | 12.04 | 7.31 | 66.230 |
| 5c | 15.68 | 27.93 | 27.45 | −7.01 | −11.72 | 68.265 |
| 1d | 50.28 | 41.08 | 22.15 | 13.55 | 2.86 | 37.398 |
| 2d | 29.07 | 44.19 | 37.79 | 36.63 | 1.163 | 33.245 |
| 3d | 46.79 | 40.13 | 41.79 | 36.13 | 33.47 | 22.210 |
| 4d | 15.27 | 62.41 | 51.74 | 30.06 | 1.16 | 29.683 |
| 5d | 11.50 | 37.43 | 23.97 | 14.19 | 11.90 | 46.678 |
| TMP | 14.71 | 12.11 | 11.76 | 10.60 | 9.44 | 64.459 |
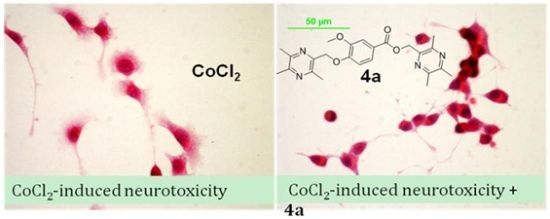
2.2.2. Effect of 4a on CoCl2-Induced Cell Injury
3. Experimental Section
3.1. Chemistry

3.1.1. General Procedure for the Preparation of Ligustrazine Derivatives 1a–5a (Scheme 1)
3.1.2. General Procedure for the Preparation of Ligustrazine Derivatives 1b–5b (Scheme 1)
3.1.3. General Procedure for the Preparation of Ligustrazine Derivatives 1c–5c (Scheme 2)
3.1.4. General Procedure for the Preparation of Ligustrazine Derivatives 1d–5d (Scheme 2)
3.2. Bio-Evaluation Methods
3.2.1. Protective Effect on Damaged Differentiated PC12 Cells [9,24,25,26]
3.2.2. Observation of Morphologic Changes [26,27]
4. Conclusions
Supplementary Materials
Acknowledgments
Conflicts of Interest
References
- Meng, Y.; Guo, Y.; Ling, Y.; Zhao, Y.; Zhang, Q.; Zhou, X.; Ding, F.; Yang, Y. Synthesis and protective effects of aralkyl alcoholic 2-acetamido-2-deoxy-b-D-pyranosides on hypoglycemia and serum limitation induced apoptosis in PC12 cell. Bioorg. Med. Chem. 2011, 19, 5577–5584. [Google Scholar] [CrossRef]
- Young, A.R.; Ali, C.; Duretête, A.; Vivien, D. Neuroprotection and stroke: Time for a compromise. J. Neurochem. 2007, 103, 1302–1309. [Google Scholar] [CrossRef]
- Sun, Y.; Jiang, J.; Zhang, Z.; Yu, P.; Wang, L.; Xu, C.; Liu, W.; Wang, Y. Antioxidative and thrombolytic TMP nitrone for treatment of ischemic stroke. Bioorg. Med. Chem. 2008, 16, 8868–8874. [Google Scholar] [CrossRef]
- Kidwell, C.S.; Liebeskind, D.S.; Starkman, S.; Saver, J.L. Trends in acute ischemic stroke trials through the 20th century. Stroke 2001, 32, 1349–1359. [Google Scholar] [CrossRef]
- Cheng, X.R.; Zhang, L.; Hu, J.J.; Sun, L.; Du, G.H. Neuroprotectiveeffectsof tetramethylpyrazine on hydrogen peroxide induced apoptosis in PC12 cells. Cell Biol. Int. 2007, 31, 438–443. [Google Scholar] [CrossRef]
- Liu, S.Y.; Sylvester, D.M. Antithrombotic/antiplatelet activity of tetramethylpyrazine. Thromb. Res. 1990, 58, 129–140. [Google Scholar] [CrossRef]
- Liu, C.F.; Lin, C.H.; Chen, C.F.; Huang, T.C.; Lin, S.C. Antioxidative effects of tetramethylpyrazine on acute ethanol-induced lipid peroxidation. Am. J. Chin. Med. 2005, 33, 981–988. [Google Scholar] [CrossRef]
- Li, S.; Chen, H.; Wang, X.; Wu, J.; Jiang, J.; Wang, Y. Pharmacokinetic study of a novel stroke therapeutic, 2-[[(1,1-dimethylethyl)oxidoimino]methyl]-3,5,6-trimethylpyrazine, by a simple HPLC-UV method in rats. Eur. J. Drug Metab. Pharmacokinet. 2011, 36, 95–101. [Google Scholar] [CrossRef]
- Chen, H.; Li, G.; Zhan, P.; Liu, X. Ligustrazine derivatives. Part 5: Design, synthesis and biological evaluation of novel ligustrazinyloxy-cinnamic acid derivatives as potent cardiovascular agents. Eur. J. Med. Chem. 2011, 46, 5609–5615. [Google Scholar] [CrossRef]
- Liu, X.; Zhang, R.; Xu, W.; Li, C.; Zhao, Q.; Wang, X. Synthesis of the novel liqustrazine derivatives and their protective effect on injured vascular endothelial cell damaged by hydrogen peroxide. Bioorg. Med. Chem. Lett. 2003, 13, 2123–2126. [Google Scholar] [CrossRef]
- Li, J.M.; Zhao, Y.H.; Ma, F.S.; Wang, Z.Y.; He, Y.; Zhang, D.S.; Ren, H.B. Synthesis of ligustrazine-aromatic acid derivatives and their inhibitory effect on platelet aggregation. Chin. J. Org. Chem. 2008, 28, 1578–1583. [Google Scholar]
- Zhang, H.N.; An, C.N.; Xu, M.; Guo, D.A.; Li, M.; Pu, X.P. Protocatechuic acid inhibits rat pheochromocytoma cell damage induced by a dopaminergic neurotoxin. Biol. Pharm. Bull. 2009, 32, 1866–1869. [Google Scholar] [CrossRef]
- Zhang, H.N.; An, C.N.; Zhang, H.N.; Pu, X.P. Protocatechuic acid inhibits neurotoxicity induced by MPTP in vivo. Neurosci. Lett. 2010, 474, 99–103. [Google Scholar] [CrossRef]
- Jeong, C.H.; Jeong, H.R.; Kim, D.O.; Choi, S.G.; Shim, K.H.; Heo, H.J. Phenolics of propolis and in vitro protective effects against oxidative stress induced cytotoxicity. J. Agric. Life Sci. 2012, 46, 87–95. [Google Scholar]
- Gepdiremen, A.; Hacimüftüoglu, A.; Düzenli, S.; Oztaş, S.; Süleyman, H. Effects of salicylic acid in glutamateand kainic acid-induced neurotoxicity in cerebellar granular cell. Pharmacol. Res. 2000, 42, 547–551. [Google Scholar] [CrossRef]
- De La Cruz, J.P.; Guerrero, A.; González-Correa, J.A.; Arrebola, M.M.; de la Cuesta, S.F. Antioxidant effect of acetylsalicylic and salicylic acid in rat brain slices subjected to hypoxia. J. Neurosci. Res. 2004, 75, 280–290. [Google Scholar] [CrossRef]
- Yang, X.; Wang, Y.; Luo, J.; Liu, S.; Yang, Z. Protective effects of YC-1 against glutamate induced PC12 cell apoptosis. Cell. Mol. Neurobiol. 2011, 31, 303–311. [Google Scholar] [CrossRef]
- Wang, H.; Zhou, X.; Huang, J.; Mu, N.; Guo, Z.; Wen, Q.; Wang, R.; Chen, S.; Feng, Z.P.; Zheng, W. The role of Akt/FoxO3a in the protective effect of venlafaxine against corticosterone-induced cell death in PC12 cells. Psychopharmacology 2013, 228, 129–141. [Google Scholar] [CrossRef]
- Hu, J.; Zhao, T.Z.; Chu, W.H.; Luo, C.X.; Tang, W.H.; Yi, L.; Feng, H. Protective effects of 20-hydroxyecdysone on CoCl(2)-induced cell injury in PC12 cells. J. Cell. Biochem. 2010, 111, 1512–1521. [Google Scholar] [CrossRef]
- Crispo, J.A.; Ansell, D.R.; Piche, M.; Eibl, J.K.; Khaper, N.; Ross, G.M.; Tai, T.C. Protective effects of polyphenolic compounds on oxidative stress-induced cytotoxicity in PC12 cells. Can. J. Physiol. Pharmacol. 2010, 88, 429–438. [Google Scholar] [CrossRef]
- Wang, P.L.; She, G.M.; Yang, Y.N.; Li, Q.; Zhang, H.G.; Liu, J.; Cao, Y.Q.; Xu, X.; Lei, H.M. Synthesis and biological evaluation of new ligustrazine derivatives as anti-tumor agents. Molecules 2012, 17, 4972–4985. [Google Scholar]
- Wang, P.L.; Xu, X.; Li, G.L.; Chu, F.H.; Lin, J.X.; Xu, K.; Zhou, S.; Gong, Y.; Zhang, Y.Z.; Li, Q.; et al. Synthesis and anti-tumor evaluation of new ligustrazine derivatives. Northwest Pharm. J. 2013, in press. [Google Scholar]
- Xu, K.; Wang, P.L.; Xu, X.; Chu, F.H.; Lin, J.X.; Zhang, Y.Z.; Lei, H.M. An overview on structural modifications of ligustrazine and biological evaluation of its synthetic derivatives. Res. Chem. Intermed. 2013. [Google Scholar] [CrossRef]
- Cheng, X.C.; Liu, X.Y.; Xu, W.F.; Guo, X.L.; Ou, Y. Design, synthesis, and biological activities of novel Ligustrazine derivatives. Bioorg. Med. Chem. 2007, 15, 3315–3320. [Google Scholar] [CrossRef]
- Li, Z.; Yu, F.; Cui, L.; Zhan, P.; Wang, S.; Shen, Y.; Liu, X. Ligustrazine derivatives. Part 6: Design, synthesis and evaluation of novel ligustrazinyl acylguanidine derivatives as potential cardiovascular agents. Med. Chem. 2012, 8, 928–933. [Google Scholar] [CrossRef]
- Shi, X.W.; Liu, L.; Gao, J.M.; Zhang, A.L. Cyathane diterpenes from Chinese mushroom Sarcodon scabrosus and their neurite outgrowth-promoting activity. Eur. J. Med. Chem. 2011, 46, 3112–3117. [Google Scholar] [CrossRef]
- Zhang, L.; Chang, M.; Li, H.; Hou, S.; Zhang, Y.; Hu, Y.; Han, W.; Hu, L. Proteomic changes of PC12 cells treated with proteasomal inhibitor PSI. Brain Res. 2007, 1153, 196–203. [Google Scholar] [CrossRef]
- Sample Availability: Samples of the compounds 1a–5a, 1b–5b, 1c–5c, 1d–5d are available from the authors.
© 2013 by the authors; licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution license (http://creativecommons.org/licenses/by/3.0/).
Share and Cite
Wang, P.; Zhang, H.; Chu, F.; Xu, X.; Lin, J.; Chen, C.; Li, G.; Cheng, Y.; Wang, L.; Li, Q.; et al. Synthesis and Protective Effect of New Ligustrazine-Benzoic Acid Derivatives against CoCl2-Induced Neurotoxicity in Differentiated PC12 Cells. Molecules 2013, 18, 13027-13042. https://doi.org/10.3390/molecules181013027
Wang P, Zhang H, Chu F, Xu X, Lin J, Chen C, Li G, Cheng Y, Wang L, Li Q, et al. Synthesis and Protective Effect of New Ligustrazine-Benzoic Acid Derivatives against CoCl2-Induced Neurotoxicity in Differentiated PC12 Cells. Molecules. 2013; 18(10):13027-13042. https://doi.org/10.3390/molecules181013027
Chicago/Turabian StyleWang, Penglong, Honggui Zhang, Fuhao Chu, Xin Xu, Jinxuan Lin, Chunxiao Chen, Guoliang Li, Yatao Cheng, Lin Wang, Qiang Li, and et al. 2013. "Synthesis and Protective Effect of New Ligustrazine-Benzoic Acid Derivatives against CoCl2-Induced Neurotoxicity in Differentiated PC12 Cells" Molecules 18, no. 10: 13027-13042. https://doi.org/10.3390/molecules181013027
APA StyleWang, P., Zhang, H., Chu, F., Xu, X., Lin, J., Chen, C., Li, G., Cheng, Y., Wang, L., Li, Q., Zhang, Y., & Lei, H. (2013). Synthesis and Protective Effect of New Ligustrazine-Benzoic Acid Derivatives against CoCl2-Induced Neurotoxicity in Differentiated PC12 Cells. Molecules, 18(10), 13027-13042. https://doi.org/10.3390/molecules181013027