Heart Failure and PAHs, OHPAHs, and Trace Elements Levels in Human Serum: Results from a Preliminary Pilot Study in Greek Population and the Possible Impact of Air Pollution
Abstract
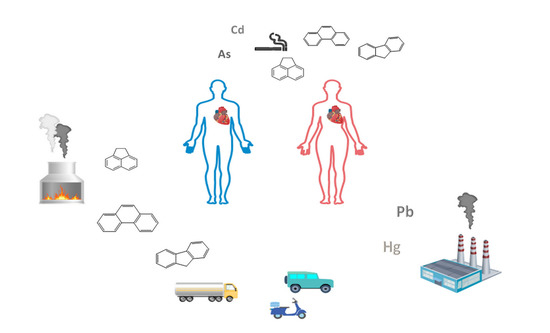
:1. Introduction
2. Results and Discussion
2.1. Cases and Controls
2.1.1. PAHs
2.1.2. OHPAHs
2.1.3. Trace Elements
2.2. Cases with Different Smoking Habits and Residence Areas
2.2.1. Sex
2.2.2. Smoking Habit
2.2.3. Area of Residence
2.3. Principal Component Analysis (PCA)
2.4. Strengths and Weaknesses
3. Materials and Methods
3.1. Study Population
3.2. Blood Sampling and Pretreatment
3.3. PAHs and OHPAHs Analysis and Quality Control
3.4. Trace Elements’ Analysis and Quality Control
3.5. Statistical Analysis
4. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Sample Availability
References
- Kelly, F.J.; Fussell, J.C. Air pollution and public health: Emerging hazards and improved understanding of risk. Environ. Geochem. Health 2015, 37, 631–649. [Google Scholar] [CrossRef] [Green Version]
- World Health Organization. Ambient (outdoor) Air Pollution. 2018. Available online: https://www.who.int/news-room/fact-sheets/detail/ambient-(outdoor)-air-quality-and-health (accessed on 1 December 2020).
- Cohen, A.J.; Brauer, M.; Burnett, R.; Anderson, H.R.; Frostad, J.; Estep, K.; Balakrishnan, K.; Brunekreef, B.; Dandona, L.; Dandona, R.; et al. Estimates and 25-year trends of the global burden of disease attributable to ambient air pollution: An analysis of data from the Global Burden of Diseases Study 2015. Lancet 2017, 389, 1907–1918. [Google Scholar] [CrossRef] [Green Version]
- Sakizadeh, M. Short-and long-term variations, spatial analysis along with cancer health risk assessment associated with 1, 3-butadiene. Atmos. Pollut. Res. 2020, 11, 755–765. [Google Scholar] [CrossRef]
- Shuai, J.; Kim, S.; Ryu, H.; Park, J.; Lee, C.K.; Kim, G. Health risk assessment of volatile organic compounds exposure near Daegu dyeing industrial complex in South Korea. BMC Public Health 2018, 18, 528. [Google Scholar] [CrossRef] [Green Version]
- Chen, T.; Gokhale, J.; Shofer, S.; Kuschner, W.G. Outdoor Air Pollution: Nitrogen Dioxide, Sulfur Dioxide, and Carbon Monoxide Health Effects. Am. J. Med. Sci. 2007, 333, 249–256. [Google Scholar] [CrossRef]
- Koukoulakis, K.G.; Chrysohou, E.; Kanellopoulos, P.G.; Karavoltsos, S.; Katsouras, G.; Dassenakis, M.; Nikolelis, D.; Bakeas, E. Trace elements bound to airborne PM10 in a heavily industrialized site nearby Athens: Seasonal patterns, emission sources, health implications. Atmos. Pollut. Res. 2019, 10, 1347–1356. [Google Scholar] [CrossRef]
- Mandalakis, M.; Tsapakis, M.; Tsoga, A.; Stephanou, E.G. Gas–particle concentrations and distribution of aliphatic hydrocarbons, PAHs, PCBs and PCDD/Fs in the atmosphere of Athens (Greece). Atmos. Environ. 2002, 36, 4023–4035. [Google Scholar] [CrossRef]
- International Agency for Research on Cancer. Air Pollution and Cancer; Straif, K., Cohen, A., Samet, J., Eds.; Publication No. 161; IARC Scientific: Lyon, France, 2013; Available online: https://publications.iarc.fr/Book-And-Report-Series/Iarc-Scientific-Publications/Air-Pollution-And-Cancer-2013 (accessed on 10 December 2020).
- Dockery, D.W.; Pope, C.A., III; Xu, X.; Spengler, J.D.; Ware, J.H.; Fay, M.E.; Ferris, B.G., Jr.; Speizer, F.E. An association between air pollutionand mortality in six U.S. cities. N. Engl. J. Med. 1993, 329, 1753–1759. [Google Scholar] [CrossRef] [Green Version]
- Srám, R.J.; Benes, I.; Binková, B.; Dejmek, J.; Horstman, D.; Kotĕsovec, F.; Otto, D.; Perreault, S.D.; Rubes, J.; Selevan, S.G.; et al. Teplice program--the impact of air pollution on human health. Environ. Health Perspect. 1996, 104, 699–714. [Google Scholar] [CrossRef] [Green Version]
- Lippmann, M.; Cohen, M.D.; Chen, L.-C. Health effects of World Trade Center (WTC) Dust: An unprecedented disaster with inadequate risk management. Crit. Rev. Toxicol. 2015, 45, 492–530. [Google Scholar] [CrossRef]
- Yin, P.; Brauer, M.; Cohen, A.J.; Wang, H.; Li, J.; Burnett, R.T.; Stanaway, J.D.; Causey, K.; Larson, S.; Godwin, W.; et al. The effect of air pollution on deaths, disease burden, and life expectancy across China and its provinces, 1990–2017: An analysis for the Global Burden of Disease Study 2017. Lancet Planet. Health 2020, 4, 386–398. [Google Scholar] [CrossRef]
- Achilleos, S.; Al-Ozairi, E.; Alahmad, B.; Garshick, E.; Neophytou, A.M.; Bouhamra, W.; Yassin, M.F.; Koutrakis, P. Acute effects of air pollution on mortality: A 17-year analysis in Kuwait. Environ. Int. 2019, 126, 476–483. [Google Scholar] [CrossRef] [PubMed]
- Lefler, J.S.; Higbee, J.D.; Burnett, R.T.; Ezzati, M.; Coleman, N.C.; Mann, D.D.; Marshall, J.D.; Bechle, M.; Wang, Y.; Robinson, A.L.; et al. Air pollution and mortality in a large, representative U.S. cohort: Multiple-pollutant analyses, and spatial and temporal decompositions. Environ. Health 2019, 18, 1–11. [Google Scholar] [CrossRef] [Green Version]
- Brønnum-Hansen, H.; Bender, A.M.; Andersen, Z.J.; Sørensen, J.; Bønløkke, J.H.; Boshuizen, H.; Becker, T.; Diderichsen, F.; Loft, S. Assessment of impact of traffic-related air pollution on morbidity and mortality in Copenhagen Municipality and the health gain of reduced exposure. Environ. Int. 2018, 121, 973–980. [Google Scholar] [CrossRef]
- Miller, M.R.; Newby, D.E. Air pollution and cardiovascular disease: Car sick. Cardiovasc. Res. 2020, 116, 279–294. [Google Scholar] [CrossRef] [PubMed]
- Shah, A.S.V.; Langrish, J.P.; Nair, H.; Mcallister, D.A.; Hunter, A.L.; Donaldson, K.; Newby, D.E.; Mills, N.L. Global association of air pollution and heart failure: A systematic review and meta-analysis. Lancet 2013, 382, 1039–1048. [Google Scholar] [CrossRef] [Green Version]
- Feng, B.; Song, X.; Dan, M.; Yu, J.; Wang, Q.; Shu, M.; Xu, H.; Wang, T.; Chen, T.; Zhang, Y.; et al. High level of source-specific particulate matter air pollution associated with cardiac arrhythmias. Sci. Total Environ. 2019, 657, 1285–1293. [Google Scholar] [CrossRef]
- Provost, E.B.; Madhloum, N.; Panis, L.I.; Boever, P.D. Carotid Intima-Media Thickness, a Marker of Subclinical Atherosclerosis, and Particulate Air Pollution Exposure: The Meta-Analytical Evidence. PLoS ONE 2015, 73, 1–12. [Google Scholar] [CrossRef] [Green Version]
- Wold, L.E.; Ying, Z.; Hutchinson, K.R.; Velten, M.; Gorr, M.W.; Velten, C.; Youtz, D.Z.; Wang, A.; Lucchesi, P.A.; Sun, Q.; et al. Cardiovascular Remodeling in Response to Long-Term Exposure to Fine Particulate Matter Air Pollution. Circ. Heart Fail. 2012, 5, 452–461. [Google Scholar] [CrossRef] [Green Version]
- Tang, C.-S.; Chuang, K.-J.; Chang, T.-Y.; Chuang, H.-C.; Chen, L.-H.; Candice Lung, S.-C.; Chang, L.-T. Effects of Personal Exposures to Micro- and Nano-Particulate Matter, Black Carbon, Particle-Bound Polycyclic Aromatic Hydrocarbons, and Carbon Monoxide on Heart Rate Variability in a Panel of Healthy Older Subjects. Int. J. Environ. Res. Public Health 2019, 16, 4672. [Google Scholar] [CrossRef] [Green Version]
- Huang, C.; Tang, M.; Li Huichu, L.; Wen, J.; Wang, C.; Gao, Y.; Hu, J.; Lin, J.; Chen, R. Particulate matter air pollution and reduced heart rate variability: How the associations vary by particle size in Shanghai, China. Ecotoxocil. Environ. Saf. 2021, 208, 111726. [Google Scholar] [CrossRef]
- Cosselman, K.E.; Navas-Acien, A.; Kaufman, J.D. Environmental factors in cardiovascular disease. Nat. Rev. Cardiol. 2015, 12, 627–642. [Google Scholar] [CrossRef]
- European Heart Network. European Cardiovascular Disease Statistics. 2017. Available online: http://www.ehnheart.org/cvd-statistics/cvd-statistics-2017.html (accessed on 2 December 2020).
- Marris, C.R.; Kompella, S.N.; Miller, M.R.; Incardona, J.P.; Brette, F.; Hancox, J.C.; Sørhus, E.; Shiels, H.A. Polyaromatic hydrocarbons in pollution: A heart-breaking matter. J. Physiol. 2020, 598, 227–247. [Google Scholar] [CrossRef]
- Lee, M.-S.; Magari, S.; Christiani, D.C. Cardiac autonomic dysfunction from occupational exposure to polycyclic aromatic hydrocarbons. Occup. Environ. Med. 2011, 68, 474–478. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Holme, J.A.; Brinchmann, B.C.; Refsnes, M.; Låg, M.; Øvrevik, J. Potential role of polycyclic aromatic hydrocarbons as mediators of cardiovascular effects from combustion particles. Environ. Health 2019, 18, 1–18. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Huang, L.; Xi, Z.; Wang, C.; Zhang, Y.; Yang, Z. Phenanthrene exposure induces cardiac hypertrophy via reducing miR-133a expression by DNA methylation. Sci. Rep. 2016, 6, 20105. [Google Scholar] [CrossRef] [Green Version]
- Seinfeld, J.H.; Pandis, S.N. Atmospheric Chemistry and Physics: From Air Pollution to Climate Change, 2nd ed.; John Wiley & Sons: New York, NY, USA, 2006; pp. 670–671. [Google Scholar]
- Haritash, A.K.; Kaushik, C.P. Biodegradation aspects of polycyclic aromatic hydrocarbons (PAHs): A review. J. Hazard. Mater. 2009, 169, 1–15. [Google Scholar] [CrossRef] [PubMed]
- Rengarajan, T.; Rajendran, P.; Nandakumar, N.; Lokeshkumar, B.; Rajendran, P.; Nishigaki, I. Exposure to polycyclic aromatic hydrocarbons with special focus on cancer. Asian. Pac. J. Trop. Biomed. 2015, 5, 182–189. [Google Scholar] [CrossRef] [Green Version]
- Tellez-Plaza, M.; Guallar, E.; Navas-Acien, A. Environmental metals and cardiovascular disease. Br. Med. J. 2018, 362, 1–4. [Google Scholar] [CrossRef]
- Houston, M.C. The Role of Mercury in Cardiovascular Disease. J. Cardiovasc. Dis. Res. 2014, 2, 1–8. [Google Scholar] [CrossRef]
- Tellez-plaza, M.; Jones, M.R.; Dominguez-Lucas, A.; Guallar, E.; Navas-Acien, A. Cadmium Exposure and Clinical Cardiovascular Disease: A Systematic Review. Curr. Atheroscler. Rep. 2013, 15, 356. [Google Scholar] [CrossRef]
- Moon, K.; Guallar, E.; Navas-acien, A. Arsenic Exposure and Cardiovascular Disease: An Updated Systematic Review. Curr. Atheroscler. Rep. 2012, 14, 542–555. [Google Scholar] [CrossRef] [Green Version]
- Navas-acien, A.; Guallar, E.; Silbergeld, E.K.; Rothenberg, S.J. Lead Exposure and Cardiovascular Disease—A Systematic Review. Environ. Health Perspect. 2007, 115, 472–482. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Rayman, M.P. The importance of selenium to human health. Lancet 2000, 356, 233–241. [Google Scholar] [CrossRef] [Green Version]
- Scheiber, I.; Dringen, R.; Mercer, J.F.B. Copper: Effects of deficiency and overload. Ιn Interrelations between Essential Metal. Ions and Human Diseases, Metal. Ions in Life Sciences; Sigel, A., Sigel, H., Sigel, R.K.O., Eds.; Springer Science Business Media: Dordrecht, The Netherlands, 2013; Volume 13, pp. 359–387. [Google Scholar] [CrossRef]
- Yamada, K. Cobalt: Its role in health and disease. In Interrelations between Essential Metal Ions and Human Diseases, Metal Ions in Life Sciences; Sigel, A., Sigel, H., Sigel, R., Eds.; Springer Science Business Media: Dordrecht, The Netherlands, 2013; Volume 13, pp. 295–320. [Google Scholar] [CrossRef]
- Chasapis, C.T.; Spiliopoulou, C.A.; Loutsidou, A.C.; Stefanidou, M.E. Zinc and human health: An update. Arch. Toxicol. 2012, 86, 521–534. [Google Scholar] [CrossRef]
- Venter, A.D.; van Zyl, P.G.; Beukes, J.P.; Josipovic, M.; Hendriks, J.; Vakkari, V.; Laakso, L. Atmospheric trace metals measured at a regional background site (Welgegund) in South Africa. Atmos. Chem. Phys. 2017, 17, 4251–4263. [Google Scholar] [CrossRef] [Green Version]
- Thurston, G.D.; Ito, K.; Lall, R. A source apportionment of U.S. fine particulate matter air pollution. Atmos. Environ. 2011, 45, 3924–3936. [Google Scholar] [CrossRef] [Green Version]
- Horemans, B.; Cardell, C.; Bencs, L.; Kontozova-Deutsch, V.; DeWael, K.; Van Grieken, R. Evaluation of airborne particles at the Alhambra monument in Granada, Spain. Microchem. J. 2011, 99, 429–438. [Google Scholar] [CrossRef]
- Gladtke, D.; Volkhausen, W.; Bach, B. Estimating the contribution of industrial facilities to annual PM10 concentrations at industrially influenced sites. Atmos. Environ. 2009, 43, 4655–4665. [Google Scholar] [CrossRef]
- Hu, C.; Hou, J.; Zhou, Y.; Sun, H.; Yin, W.; Zhang, Y.; Wang, X.; Wang, G.; Chen, W.; Yuan, J. Association of polycyclic aromatic hydrocarbons exposure with atherosclerotic cardiovascular disease risk: A role of mean platelet volume or club cell secretory protein. Environ. Pollut. 2018, 233, 45–53. [Google Scholar] [CrossRef]
- Alshaarawy, O.; Elbaz, H.A.; Andrew, M.E. The association of urinary polycyclic aromatic hydrocarbon biomarkers and cardiovascular disease in the US population. Environ. Int. 2016, 89–90, 174–178. [Google Scholar] [CrossRef] [Green Version]
- Clark, J.D.; Serdar, B.; Lee, D.J.; Arheart, K.; Wilkinson, J.D.; Fleming, L.E. Exposure to polycyclic aromatic hydrocarbons and serum inflammatory markers of cardiovascular disease. Environ. Res. 2012, 117, 132–137. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Sun, L.; Ye, Z.; Ling, Y.; Cai, S.; Xu, J.; Fan, C.; Zhong, Y.; Shen, Q.; Li, Y. Relationship between polycyclic aromatic hydrocarbons and rheumatoid arthritis in US general population, NHANES 2003–2012. Sci. Total Environ. 2020, 704, 135294. [Google Scholar] [CrossRef]
- Khosravipour, M.; Khosravipour, H. The association between urinary metabolites of polycyclic aromatic hydrocarbons and diabetes: A systematic review and meta-analysis study. Chemosphere 2020, 247, 125680. [Google Scholar] [CrossRef] [PubMed]
- Santos, P.M.; del Nogal Sánchez, M.; Pavón, J.L.P.; Cordero, B.M. Determination of polycyclic aromatic hydrocarbons in human biological samples: A critical review. Trends Analyt. Chem. 2019, 113, 194–209. [Google Scholar] [CrossRef]
- Pleil, J.D.; Stiegel, M.A.; Sobus, J.R.; Tabucchi, S.; Ghio, A.J.; Madden, M.C. Cumulative exposure assessment for trace-level polycyclic aromatic hydrocarbons (PAHs) using human blood and plasma analysis. J. Chromatogr. B 2010, 878, 1753–1760. [Google Scholar] [CrossRef]
- Song, X.F.; Chen, Z.Y.; Zang, Z.J.; Zhang, Y.N.; Zeng, F.; Peng, Y.P.; Yang, C. Investigation of polycyclic aromatic hydrocarbon level in blood and semen quality for residents in Pearl River Delta Region in China. Environ. Int. 2013, 60, 97–105. [Google Scholar] [CrossRef] [PubMed]
- Koukoulakis, K.G.; Kanellopoulos, P.G.; Chrysochou, E.; Koukoulas, V.; Minaidis, M.; Maropoulos, G.; Nikoleli, G.P.; Bakeas, E. Leukemia and PAHs levels in human blood serum: Preliminary results from an adult cohort in Greece. Atmos. Pollut. Res. 2020, 11, 1552–1565. [Google Scholar] [CrossRef]
- Boada, L.D.; Henríquez-Hernández, L.A.; Navarro, P.; Zumbado, M.; Almeida-González, M.; Camacho, M.; Álvarez-León, E.E.; Valencia-Santana, J.A.; Luzardo, O.P. Exposure to polycyclic aromatic hydrocarbons (PAHs) and bladder cancer: Evaluation from a gene-environment perspective in a hospital-based case-control study in the Canary Islands (Spain). Int. J. Occup. Med. Environ. Health 2015, 21, 23–30. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Singh, V.K.; Patel, D.K.; Ram, S.; Mathur, N.; Siddiqui, M.K.J.; Behari, J.R. Blood levels of polycyclic aromatic hydrocarbons in children of Lucknow, India. Arch. Environ. Contam. Toxicol. 2008, 54, 348–354. [Google Scholar] [CrossRef]
- Tsang, H.L.; Wu, S.; Leung, C.K.M.; Tao, S.; Wong, M.H. Body burden of POPs of Hong Kong residents, based on human milk, maternal and cord serum. Environ. Int. 2011, 37, 142–151. [Google Scholar] [CrossRef]
- Zhang, X.; Li, X.; Jing, Y.; Fang, X.; Zhang, X.; Lei, B.; Yu, Y. Transplacental transfer of polycyclic aromatic hydrocarbons in paired samples of maternal serum, umbilical cord serum, and placenta in Shangai, China. Eniviron. Pollut. 2017, 222, 267–275. [Google Scholar] [CrossRef]
- Chen, Q.; Zheng, T.; Bassig, B.A.; Cheng, Y.; Leaderer, B.; Lin, S.; Holford, T.; Qiu, J.; Zhang, Y.; Shi, K.; et al. Prenatal exposure to polycyclic aromatic hydrocarbons and birth weight in China. Open J. Air Pollut. 2014, 3, 100–110. [Google Scholar] [CrossRef] [Green Version]
- Heitland, P.; Koster, H.D. Human biomonitoring of 73 elements in blood, serum, erythrocytes and urine. J. Trace. Elem. Med. Biol. 2021, 64, 126706. [Google Scholar] [CrossRef]
- Ivanenko, N.B.; Ganeev, A.A.; Solovyev, N.D.; Moskvin, L.N. Determination of Trace Elements in Biological fluids. J. Anal. Chem. 2011, 66, 784–799. [Google Scholar] [CrossRef]
- Asgary, S.; Movahedian, A.; Keshvari, M.; Taleghani, M.; Sahebkar, A.; Sarrafzadegan, N. Serum levels of lead, mercury and cadmium in relation to coronary artery disease in the elderly: A cross-sectional study. Chemosphere 2017, 180, 540–544. [Google Scholar] [CrossRef]
- Ari, E.; Kaya, Y.; Demir, H.; Asicioglu, E.; Keskin, S. The correlation of serum trace elements and heavy metals with carotid artery atherosclerosis in maintenance hemodialysis patients. Biol. Trace. Elem. Res. 2011, 144, 351–359. [Google Scholar] [CrossRef]
- Koh, H.Y.; Kim, T.H.; Sheen, Y.H.; Lee, S.W.; An, J.; Kim, M.A.; Han, M.Y.; Yon, D.K. Serum heavy metal levels are associated with asthma, allergic rhinitis, atopic dermatitis, allergic multimorbidity, and airflow obstruction. J. Allergy Clin. Immunol. Pract. 2019, 7, 2912–2915.e2. [Google Scholar] [CrossRef]
- Ohanian, M.; Telouk, P.; Kornblau, S.; Albarede, F.; Ruvolo, P.; Tidwell, R.S.S.; Plesa, A.; Kanagal-Shamanna, R.; Matera, E.L.; Cortes, J.; et al. A heavy metal baseline score predicts outcome in acute myeloid leukemia. Am. J. Hematol. 2020, 95, 422–434. [Google Scholar] [CrossRef]
- Khuder, A.; Issa, H.; Bakir, M.A.; Habil, K.; Mohammad, A.; Solaiman, A. Major, minor, and trace elements in whole blood of patients with different leukemia patterns. Nukleonika 2012, 57, 389–399. [Google Scholar]
- Inamdar, A.A.; Inamdar, A.C. Heart Failure: Diagnosis, Management and Utilization. J. Clin. Med. 2016, 5, 62. [Google Scholar] [CrossRef]
- Palazzuoli, A.; Nuti, R. Heart failure: Pathophysiology and clinical picture. In Fluid Overload: Diagnosis and Management, Contributions to Nephrology; Ronco, C., Costanzo, M.R., Bellomo, R., Maisel, A.S., Eds.; Karger: Basel, Switzerland, 2010; Volume 164, pp. 1–10. [Google Scholar] [CrossRef]
- Wang, B.; Jin, L.; Ren, A.; Yuan, Y.; Liu, J.; Li, Z.; Zhang, L.; Yi, D.; Wang, L.L.; Zhang, Y.; et al. Levels of polycyclic aromatic hydrocarbons in maternal serum and risk of neural tube defects in offspring. Environ. Sci. Technol. 2015, 49, 588–596. [Google Scholar] [CrossRef] [PubMed]
- Qin, Y.Y.; Leung, C.K.M.; Lin, C.K.; Leung, A.O.W.; Wang, H.S.; Giesy, J.P.; Wong, M.H. Halogenated POPs and PAHs in blood plasma of Hong Kong residents. Environ. Sci. Technol. 2011, 45, 1630–1637. [Google Scholar] [CrossRef]
- Loutfy, N.M.; Malhat, F.; Ahmed, M.T. Polycyclic aromatic hydrocarbons residues in blood serum and human milk, an Egyptian pilot study. Hum. Ecol. Risk. Assess. 2017, 23, 1573–1584. [Google Scholar] [CrossRef]
- Yang, Q.; Zhao, Y.; Qiu, X.; Zhang, C.; Li, R.; Qiao, J. Association of serum levels of typical organic pollutants with polycystic ovary syndrome (PCOS): A case-control study. Hum. Reprod. 2015, 30, 1964–1973. [Google Scholar] [CrossRef] [PubMed]
- Cao, L.; Wang, D.; Zhu, C.; Wang, B.; Cen, X.; Chen, A.; Zhou, H.; Ye, Z.; Tan, Q.; Nie, X.; et al. Polycyclic aromatic hydrocarbon exposure and atherosclerotic cardiovascular disease risk in urban adults: The mediating role of oxidatively damaged DNA. Environ. Pollut. 2020, 265, 114860. [Google Scholar] [CrossRef] [PubMed]
- Hajir, S.; Al Aaraj, L.; Zgheib, N.; Badr, K.; Ismaeel, H.; Abchee, A.; Tamim, H.; Saliba, N.A. The association of urinary metabolites of polycyclic aromatic hydrocarbons with obstructive coronary artery disease: A red alert for action. Environ. Pollut. 2020, 115967. [Google Scholar] [CrossRef]
- Yin, W.; Hou, J.; Xu, T.; Cheng, J.; Li, P.; Wang, L.; Zhang, Y.; Wang, X.; Hu, C.; Huang, C.; et al. Obesity mediated the association of exposure to polycyclic aromatic hydrocarbon with risk of cardiovascular events. Sci. Total Environ. 2018, 616–617, 841–854. [Google Scholar] [CrossRef] [PubMed]
- Gao, P.; da Silva, E.; Hou, L.; Denslow, N.D.; Xiang, P.; Ma, L.Q. Human exposure to polycyclic aromatic hydrocarbons: Metabolomics perspective. Environ. Int. 2018, 119, 466–477. [Google Scholar] [CrossRef]
- Sevim, Ç.; Doğan, E.; Comakli, S. Cardiovascular disease and toxic metals. Curr. Opin. Toxicol. 2020, 19, 88–92. [Google Scholar] [CrossRef]
- Yang, A.M.; Lo, K.; Zheng, T.Z.; Yang, J.L.; Bai, Y.N.; Feng, Y.Q.; Cheng, N.; Liu, S.M. Environmental heavy metals and cardiovascular diseases: Status and future direction. Chronic. Dis. Transl. Med. 2020, 6, 251–259. [Google Scholar] [CrossRef] [PubMed]
- Mu, X.; Wang, Z.; Liu, L.; Guo, X.; Gu, C.; Xu, H.; Zhao, L.; Jiang, W.; Cao, H.; Mao, X.; et al. Multiple exposure pathways of first-year university students to heavy metals in China: Serum sampling and atmospheric modeling. Sci. Total Environ. 2020, 746, 141405. [Google Scholar] [CrossRef] [PubMed]
- Pappas, R.S.; Fresquez, M.R.; Martone, N.; Watson, C.H. Toxic metal concentrations in mainstream smoke from cigarettes available in the USA. J. Anal. Toxicol. 2014, 38, 204–211. [Google Scholar] [CrossRef] [Green Version]
- Agency for Toxic Substances and Disease Registry. Medical Management Guidelines for Arsenic (As) and Inorganic Arsenic Compounds. 2014. Available online: https://www.atsdr.cdc.gov/MMG/MMG.asp?id=1424&tid=3 (accessed on 1 December 2020).
- Yousef, S.; Eapen, V.; Zoubeidi, T.; Kosanovic, M.; Mabrouk, A.A.; Adem, A. Learning disorder and blood concentration of heavy metals in the United Arab Emirates. Asian. J. Psychiatr. 2013, 6, 394–400. [Google Scholar] [CrossRef] [PubMed]
- Xiang, S.; Jin, Q.; Xu, F.; Yao, Y.; Liang, W.; Zuo, X.; Ye, T.; Ying, C. High serum arsenic and cardiovascular risk factors in patients undergoing continuous ambulatory peritoneal dialysis. J. Trace. Elem. Med. Biol. 2019, 52, 1–5. [Google Scholar] [CrossRef]
- World Health Organization. Environmental Health Criteria 135: Cadmium: Environmental Aspects. 1992. Available online: http://www.inchem.org/documents/ehc/ehc/ehc135.htm (accessed on 11 December 2020).
- Choi, S.; Kwon, J.; Kwon, P.; Lee, C.; Jang, S.I. Association between blood heavy metal levels and predicted 10-year risk for a first atherosclerosis cardiovascular disease in the general korean population. Int. J. Environ. Res. Public Health 2020, 17, 2134. [Google Scholar] [CrossRef] [Green Version]
- Genchi, G.; Sinicropi, M.S.; Carocci, A.; Lauria, G.; Catalano, A. Mercury exposure and heart diseases. Int. J. Environ. Res. Public Health 2017, 14, 74. [Google Scholar] [CrossRef] [Green Version]
- Hightower, J.M.; Moore, D. Mercury levels in high-end consumers of fish. Environ. Health Perspect. 2003, 111, 604–608. [Google Scholar] [CrossRef] [Green Version]
- Adimado, A.A.; Baah, D.A. Mercury in Human Blood, Urine, Hair, Nail, and Fish from the Ankobra and Tano River Basins in Southwestern Ghana. Bull. Environ. Contam. Toxicol. 2002, 68, 339–346. [Google Scholar] [CrossRef]
- Houston, M.C. Role of mercury toxicity in hypertension, cardiovascular disease, and stroke. J. Clin. Hypertens. 2011, 13, 621–627. [Google Scholar] [CrossRef]
- Liu, S.; Tsui, M.T.; Lee, E.; Fowler, J.; Jia, Z. Uptake, efflux, and toxicity of inorganic and methyl mercury in the endothelial cells (EA.hy926). Sci. Rep. 2020, 10, 9023. [Google Scholar] [CrossRef] [PubMed]
- Agency for Toxic Substances and Disease Registry. Case Studies in Environmental Medicine (CSEM), Lead Toxicity. 2017. Available online: https://www.atsdr.cdc.gov/csem/lead/docs/csem-lead_toxicity_508.pdf (accessed on 2 December 2020).
- Sharma, B.; Singh, S.; Siddiqi, N.J. Biomedical Implications of Heavy Metals Induced Imbalances in Redox Systems. Biomed. Res. Int. 2014, 2014, 640754. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Vaziri, N.D. Mechanisms of lead-induced hypertension and cardiovascular disease. Am. J. Physiol. Heart Circ. Physiol. 2008, 295, 454–465. [Google Scholar] [CrossRef] [Green Version]
- Patrick, L. Lead toxicity part II: The role of free radical damage and the use of antioxidants in the pathology and treatment of lead toxicity. Altern. Med. Rev. 2006, 11, 114–127. [Google Scholar] [PubMed]
- Navas-acien, A.; Selvin, E.; Sharrett, A.R.; Calderon-Aranda, E.; Silbergeld, E.; Guallar, E. Lead, Cadmium, Smoking, and Increased Risk of Peripheral Arterial Disease. Circulation 2004, 109, 3196–3201. [Google Scholar] [CrossRef] [Green Version]
- Karadas, S.; Sayin, R.; Aslan, M.; Gonullu, H.; Kati, C.; Dursun, R.; Duran, L.; Gonullu, E.; Demir, H. Serum levels of trace elements and heavy metals in patients with acute hemorrhagic stroke. J. Membr. Biol. 2014, 247, 175–180. [Google Scholar] [CrossRef]
- Ford, E.S. Serum copper concentration and coronary heart disease among US adults. Am. J. Epidemiol. 2000, 151, 1182–1188. [Google Scholar] [CrossRef]
- Leone, N.; Courbon, D.; Ducimetiere, P.; Zureik, M. Zinc, copper, and magnesium and risks for all-cause, cancer, and cardiovascular mortality. Epidemiology 2006, 17, 308–314. [Google Scholar] [CrossRef] [PubMed]
- Lind, P.M.; Olsén, L.; Lind, L. Circulating levels of metals are related to carotid atherosclerosis in elderly. Sci. Total Environ. 2012, 416, 80–88. [Google Scholar] [CrossRef]
- Alissa, E.M.; Bahjri, S.M.; Ahmed, W.H.; Al-Ama, N.; Ferns, G.A.A. Chromium status and glucose tolerance in Saudi men with and without coronary artery disease. Biol. Trace. Elem. Res. 2009, 131, 215–228. [Google Scholar] [CrossRef]
- Afridi, H.; Kazi, T.G.; Kazi, N.; Sirajuddin, U.; Kandhro, G.A.; Baig, J.A.; Shah, A.Q.; Jamali, M.K.; Arain, M.B.; Wadhwa, S.K.; et al. Chromium and manganese levels in biological samples of Pakistani myocardial infarction patients at different stages as related to controls. Biol. Trace. Elem. Res. 2011, 142, 259–273. [Google Scholar] [CrossRef]
- Gutierrez-Bedmar, M.; Martinez-Gonzalez, M.A.; Munoz-Bravo, C.; Ruiz-Canela, M.; Mariscal, A.; Salas-Salvado, J.; Estruch, R.; Corella, D.; Aros, F.; Fito Colomer, M.; et al. Chromium exposure and risk of cardiovascular disease in high cardiovascular risk subjects: Nested case-control study in the prevention with mediterranean diet (PREDIMED) study. Circ. J. 2017, 81, 1183–1190. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Keir, J.L.A.; Cakmak, S.; Blais, J.M.; White, P.A. The influence of demographic and lifestyle factors on urinary levels of PAH metabolites—empirical analyses of Cycle 2 (2009–2011) CHMS data. J. Expo. Sci. Environ. Epidemiol. 2020, 31, 386–397. [Google Scholar] [CrossRef] [Green Version]
- Sakellari, A.; Karavoltsos, S.; Kalogeropoulos, N.; Theodorou, D.; Dedoussis, G.; Chrysohoou, C.; Dassenakis, M.; Scoullos, M. Predictors of cadmium and lead concentrations in the blood of residents from the metropolitan area of Athens (Greece). Sci. Total Environ. 2016, 568, 263–270. [Google Scholar] [CrossRef]
- Lee, J.W.; Lee, C.K.; Moon, C.S.; Choi, I.J.; Lee, K.J.; Yi, S.M.; Jang, B.K.; Yoon, B.J.; Kim, D.S.; Peak, D.; et al. Korea National Survey for Environmental Pollutants in the Human Body 2008: Heavy metals in the blood or urine of the Korean population. Int. J. Hyg. Environ. Health 2012, 215, 449–457. [Google Scholar] [CrossRef]
- Nunes, J.A.; Batista, B.L.; Rodrigues, J.L.; Caldas, N.M.; Neto, J.A.G.; Barbosa, F. A simple method based on ICP-MS for estimation of background levels of arsenic, cadmium, copper, manganese, nickel, lead, and selenium in blood of the Brazilian population. J. Toxicol. Environ. Health Part. A 2010, 73, 878–887. [Google Scholar] [CrossRef] [PubMed]
- Nisse, C.; Tagne-Fotso, R.; Howsam, M.; Richeval, C.; Labat, L.; Leroyer, A. Blood and urinary levels of metals and metalloids in the general adult population of Northern France: The IMEPOGE study, 2008–2010. Int. J. Hyg. Environ. Health 2017, 220, 341–363. [Google Scholar] [CrossRef] [PubMed]
- Vahter, M.; Berglund, M.; Akesson, A.; Liden, C. Metals and women’s health. Environ. Res. 2002, 88, 145–155. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Mathers, C.D.; Loncar, D. Projections of global mortality and burden of disease from 2002 to 2030. PLoS Med. 2006, 3, 2011–2030. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Wong, N.D. Epidemiological studies of CHD and the evolution of preventive cardiology. Nat. Rev. Cardiol. 2014, 11, 276–289. [Google Scholar] [CrossRef]
- Pirie, K.; Peto, R.; Reeves, G.K.; Green, J.; Beral, V. The 21st century hazards of smoking and benefits of stopping: A prospective study of one million women in the UK. Lancet 2013, 381, 133–141. [Google Scholar] [CrossRef] [Green Version]
- Gopal, D.M.; Kalogeropoulos, A.P.; Georgiopoulou, V.V.; Smith, A.L.; Bauer, D.C.; Newman, A.B.; Kim, L.; Bibbins-Domingo, K.; Tindle, H.; Harris, T.B.; et al. Cigarette smoking exposure and heart failure risk in older adults: The Health, Aging, and Body Composition Study. Am. Heart J. 2012, 164, 236–242. [Google Scholar] [CrossRef] [Green Version]
- Wang, Y.; Wong, L.; Meng, L.; Pittman, E.N.; Trinidad, D.A.; Hubbard, K.L.; Etheredge, A.; Del Valle-Pinero, A.Y.; Zamoiski, R.; van Bemmel, D.M.; et al. Urinary concentrations of monohydroxylated polycyclic aromatic hydrocarbons in adults from the U.S. Population Assessment of Tobacco and Health (PATH) Study Wave 1 (2013–2014). Environ. Int. 2019, 123, 201–208. [Google Scholar] [CrossRef] [PubMed]
- Jain, R.B. Trends and concentrations of selected polycyclic aromatic hydrocarbons in general US population: Data from NHANES 2003–2008. Cogent. Environ. Sci. 2015, 110, 1–16. [Google Scholar] [CrossRef]
- Pappas, R.S. Toxic elements in tobacco and in cigarette smoke: Inflammation and sensitization. Metallomics 2011, 3, 1181–1198. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Bonberg, N.; Pesch, B.; Ulrich, N.; Moebus, S.; Eisele, L.; Marr, A.; Arendt, M.; Jöckel, K.H.; Brüning, T.; Weiss, T. The distribution of blood concentrations of lead (Pb), cadmium (Cd), chromium (Cr) and manganese (Mn) in residents of the German Ruhr area and its potential association with occupational exposure in metal industry and/or other risk factors. Int. J. Hyg. Environ. Health 2017, 220, 998–1005. [Google Scholar] [CrossRef] [PubMed]
- Kasdagli, M.I.; Katsouyanni, K.; de Hoogh, K.; Lagiou, P.; Samoli, E. Associations of air pollution and greenness with mortality in Greece: An ecological study. Environ. Res. 2020, 110348. [Google Scholar] [CrossRef]
- Fourtziou, L.; Liakakou, E.; Stavroulas, I.; Theodosi, C.; Zarmpas, P.; Psiloglou, B.; Sciare, J.; Maggos, T.; Bairachtari, K.; Bougiatioti, A.; et al. Multi-tracer approach to characterize domestic wood burning in Athens (Greece) during wintertime. Atmos. Environ. 2017, 148, 89–101. [Google Scholar] [CrossRef]
- Gratsea, M.; Liakakou, E.; Mihalopoulos, N.; Adamopoulos, A.; Tsilibari, E.; Gerasopoulos, E. The combined effect of reduced fossil fuel consumption and increasing biomass combustion on Athens’ air quality, as inferred from long term CO measurements. Sci. Total Environ. 2017, 592, 115–123. [Google Scholar] [CrossRef] [PubMed]
- Paraskevopoulou, D.; Liakakou, E.; Gerasopoulos, E.; Mihalopoulos, N. Sources of atmospheric aerosol from long-term measurements (5years) of chemical composition in Athens, Greece. Sci. Total Environ. 2015, 527–528, 165–178. [Google Scholar] [CrossRef]
- Saffari, A.; Daher, N.; Samara, C.; Voutsa, D.; Kouras, A.; Manoli, E.; Karagiozidou, O.; Vlachokostas, C.; Moussiopoulos, N.; Shafer, M.M.; et al. Increased biomass burning due to the economic crisis in Greece and its adverse impact on wintertime air quality in Thessaloniki. Environ. Sci. Technol. 2013, 47, 13313–13320. [Google Scholar] [CrossRef]
- Michas, G.; Karvelas, G.; Trikas, A. Cardiovascular disease in Greece; the latest evidence on risk factors. Hellenic J. Cardiol. 2019, 60, 271–275. [Google Scholar] [CrossRef] [PubMed]
- Vasilakos, C.; Levi, N.; Maggos, T.; Hatzianestis, J.; Michopoulos, J.; Helmis, C. Gas-particle concentration and characterization of sources of PAHs in the atmosphere of a suburban area in Athens, Greece. J. Hazard. Mater. 2007, 140, 45–51. [Google Scholar] [CrossRef]
- Pateraki, S.; Asimakopoulos, D.N.; Maggos, T.; Assimakopoulos, V.D.; Bougiatioti, A.; Bairachtari, K.; Vasilakos, C.; Mihalopoulos, N. Chemical characterization, sources and potential health risk of PM2.5 and PM1 pollution across the Greater Athens Area. Chemosphere 2020, 241, 125026. [Google Scholar] [CrossRef] [PubMed]
- Srogi, K. Monitoring of environmental exposure to polycyclic aromatic hydrocarbons: A review. Environ. Chem Lett. 2007, 5, 169–195. [Google Scholar] [CrossRef] [Green Version]
- Gerde, P.; Muggenburg, B.A.; Lundborg, M.; Dahl, A.R. The rapid alveolar absorption of diesel soot-adsorbed benzo[a]pyrene: Bioavailability, metabolism and dosimetry of an inhaled particle-borne carcinogen. Carcinogenesis 2001, 22, 741–749. [Google Scholar] [CrossRef]
- Laamech, J.; Bernard, A.; Dumont, X.; Benazzouz, B.; Lyoussi, B. Blood lead, cadmium and mercury among children from urban, industrial and rural areas of Fez Boulemane Region (Morocco): Relevant factors and early renal effects. Int. J. Occup. Med. Environ. Health 2014, 27, 641–659. [Google Scholar] [CrossRef]
- Kim, L.; Jeon, H.J.; Kim, Y.C.; Yang, S.H.; Choi, H.; Kim, T.O.; Lee, S.E. Monitoring polycyclic aromatic hydrocarbon concentrations and distributions in rice paddy soils from Gyeonggi-do, Ulsan, and Pohang. Appl. Biol. Chem. 2019, 62, 18. [Google Scholar] [CrossRef] [Green Version]
- Wang, Z.; Liu, Z.; Xu, K.; Mayer, L.M.; Zhang, Z.; Kolker, A.S.; Wu, W. Concentrations and sources of polycyclic aromatic hydrocarbons in surface coastal sediments of the northern Gulf of Mexico. Geochem. Trans. 2014, 15, 1–12. [Google Scholar] [CrossRef] [Green Version]
- Neta, G.; Goldman, L.R.; Barr, D.; Sjodin, A.; Apelberg, B.J.; Witter, F.R.; Halden, R.U. Distribution and determinants of pesticide mixtures in cord serum using principal component analysis. Environ. Sci. Technol. 2010, 44, 5641–5648. [Google Scholar] [CrossRef] [PubMed]
- Andrysík, Z.; Vondráček, J.; Marvanová, S.; Ciganek, M.; Neča, J.; Pěnčíková, K.; Mahadevan, B.; Topinka, J.; Baird, W.M.; Kozubík, A.; et al. Activation of the aryl hydrocarbon receptor is the major toxic mode of action of an organic extract of a reference urban dust particulate matter mixture: The role of polycyclic aromatic hydrocarbons. Mutat. Res. 2011, 714, 53–62. [Google Scholar] [CrossRef]
- Barron, M.G.; Heintz, R.; Rice, S.D. Relative potency of PAHs and heterocycles as aryl hydrocarbon receptor agonists in fish. Mar. Environ. Res. 2004, 58, 95–100. [Google Scholar] [CrossRef]
- Solenkova, N.V.; Newman, J.D.; Berger, J.S.; Thurston, G.; Hochman, J.S.; Lamas, G.A. Metal pollutants and cardiovascular disease: Mechanisms and consequences of exposure. Am. Heart J. 2014, 168, 812–822. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Duruibe, J.O.; Ogwuegbu, M.O.; Egwurugwu, J.N. Heavy metal pollution and human biotoxic effects. Int. J. Phys. Sci. 2007, 2, 112–118. [Google Scholar] [CrossRef]
- Huang, T.; Li, J.; Zhang, W. Application of principal component analysis and logistic regression model in lupus nephritis patients with clinical hypothyroidism. BMC Med. Res. Methodol. 2020, 20, 99. [Google Scholar] [CrossRef] [PubMed]
- DiStefano, C.; Zhu, M.; Mîndrilã, D. Understanding and Using Factor Scores: Considerations for the Applied Researcher. Pract. Assess. Res. Eval. 2009, 14. [Google Scholar] [CrossRef]
- Chowdhury, R.; Ramond, A.; O’Keeffe, L.M.; Shahzad, S.; Kunutsor, S.K.; Muka, T.; Gregson, J.; Willeit, P.; Warnakula, S.; Khan, H.; et al. Environmental toxic metal contaminants and risk of cardiovascular disease: Systematic review and meta-analysis. BMJ 2018, 362, k3310. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Batáriová, A.; Spěváčková, V.; Beneš, B.; Čejchanová, M.; Šmíd, J.; Černá, M. Blood and urine levels of Pb, Cd and Hg in the general population of the Czech Republic and proposed reference values. Int. J. Hyg. Environ. Health 2006, 209, 359–366. [Google Scholar] [CrossRef] [PubMed]
- Jin, L.; Liu, J.; Ye, B.; Ren, A. Concentrations of selected heavy metals in maternal blood and associated factors in rural areas in Shanxi Province, China. Environ. Int. 2014, 66, 157–164. [Google Scholar] [CrossRef]
- United States Environmental Protection Agency. Definition and Procedures for the Determination of the Method Detection Limit. App. B, Part 136:343–345. 40 CFR Ch (7–1–12 edition). 2016. Available online: https://www.epa.gov/sites/production/files/2016-12/documents/mdl-procedure_rev2_12-13-2016.pdf (accessed on 10 December 2020).
- Kanellopoulos, P.G.; Verouti, E.; Chrysochou, E.; Koukoulakis, K.; Bakeas, E. Primary and secondary organic aerosol in an urban/industrial site: Sources, health implications and the role of plastic enriched waste burning. J. Environ. Sci. 2021, 99, 222–238. [Google Scholar] [CrossRef]
- Manoli, E.; Kouras, A.; Karagkiozidou, O.; Argyropoulos, G.; Voutsa, D.; Samara, C. Polycyclic aromatic hydrocarbons (PAHs) at traffic and urban background sites of northern Greece: Source apportionment of ambient PAH levels and PAH-induced lung cancer risk. Environ. Sci. Pollut. Res. 2016, 23, 3556–3568. [Google Scholar] [CrossRef] [PubMed]
- Santos, E.; Souza, M.R.R.; Vilela Junior, A.R.; Soares, L.S.; Frena, M.; Alexandre, M.R. Polycyclic aromatic hydrocarbons (PAH) in superficial water from a tropical estuarine system: Distribution, seasonal variations, sources and ecological risk assessment. Mar. Pollut. Bull. 2018, 127, 352–358. [Google Scholar] [CrossRef]
- Hussain, K.; Hoque, R.R. Seasonal attributes of urban soil PAHs of the Brahmaputra Valley. Chemosphere 2015, 119, 794–802. [Google Scholar] [CrossRef] [PubMed]
- Alhamdow, A.; Lindh, C.; Albin, M.; Gustavsson, P.; Tinnerberg, H.; Broberg, K. Early markers of cardiovascular disease are associated with occupational exposure to polycyclic aromatic hydrocarbons. Sci. Rep. 2017, 7, 1–11. [Google Scholar] [CrossRef]
- Ravindra, K.; Sokhi, R.; Van Grieken, R. Atmospheric polycyclic aromatic hydrocarbons: Source attribution, emission factors and regulation. Atmos. Environ. 2008, 42, 2895–2921. [Google Scholar] [CrossRef] [Green Version]
- Jollife, I.T.; Cadima, J. Principal component analysis: A review and recent developments. Phil. Trans. R. Soc. A 2016, 374, 20150202. [Google Scholar] [CrossRef] [PubMed]
- Pathak, A.K.; Sharma, M.; Katiyar, S.K.; Katiyar, S.; Nagar, P.K. Logistic regression analysis of environmental and other variables and incidences of tuberculosis in respiratory patients. Sci. Rep. 2020, 10, 21843. [Google Scholar] [CrossRef]













| Cases | Controls | |||||
|---|---|---|---|---|---|---|
| Variance % | 18.2 | 10.5 | 8.3 | 15.0 | 12.0 | 8.8 |
| 1 | 2 | 3 | 1 | 2 | 3 | |
| PHE | 0.873 | −0.100 | 0.137 | 0.074 | 0.631 | −0.481 |
| FLT | 0.866 | 0.016 | 0.159 | 0.215 | 0.187 | −0.238 |
| ACE | 0.804 | 0.211 | 0.059 | 0.089 | 0.295 | −0.394 |
| NAP | 0.764 | −0.063 | 0.171 | 0.505 | −0.302 | −0.112 |
| 1OHPYR | 0.741 | 0.362 | −0.334 | −0.126 | 0.704 | 0.247 |
| FL | 0.735 | 0.090 | 0.237 | 0.022 | 0.118 | −0.020 |
| PYR | 0.694 | 0.177 | 0.289 | −0.240 | 0.639 | 0.164 |
| 2OHPHE | 0.692 | −0.111 | −0.129 | 0.553 | 0.365 | −0.213 |
| ANT | 0.676 | 0.101 | 0.209 | 0.490 | 0.219 | 0.022 |
| 3OHPHE | 0.634 | −0.067 | −0.252 | 0.016 | 0.268 | 0.589 |
| Cd | 0.139 | 0.704 | 0.122 | −0.113 | 0.196 | −0.365 |
| Pb | 0.138 | 0.631 | 0.118 | 0.613 | 0.089 | 0.203 |
| Co | 0.011 | 0.624 | 0.091 | −0.325 | −0.440 | −0.016 |
| Hg | 0.015 | 0.601 | 0.118 | 0.110 | −0.041 | −0.002 |
| CHR | 0.061 | −0.051 | 0.728 | 0.604 | 0.012 | −0.042 |
| BaA | 0.313 | −0.009 | 0.614 | 0.452 | 0.007 | 0.173 |
| DBA | −0.118 | −0.172 | 0.610 | −0.012 | 0.746 | 0.146 |
| BFA | 0.189 | 0.073 | 0.606 | 0.482 | 0.514 | 0.083 |
| ACY | 0.290 | 0.027 | 0.033 | 0.536 | −0.192 | 0.214 |
| BaP | −0.034 | 0.360 | −0.006 | 0.901 | −0.024 | 0.057 |
| IPY | −0.038 | 0.155 | 0.324 | 0.803 | 0.231 | −0.176 |
| 1OHNAP | 0.023 | 0.507 | −0.038 | 0.005 | 0.261 | 0.644 |
| 2OHNAP | 0.200 | 0.420 | −0.142 | −0.006 | −0.094 | 0.477 |
| 1OHPHE | −0.098 | 0.473 | −0.255 | 0.314 | 0.291 | 0.225 |
| 9OHPHE | 0.368 | 0.264 | −0.221 | −0.003 | −0.258 | 0.057 |
| As | 0.014 | 0.364 | 0.303 | 0.229 | 0.239 | 0.099 |
| Ba | 0.419 | 0.215 | −0.174 | 0.386 | 0.028 | −0.244 |
| Cr | 0.063 | 0.432 | −0.188 | 0.166 | 0.252 | 0.776 |
| Cu | 0.031 | 0.303 | −0.150 | 0.464 | −0.487 | 0.256 |
| Ni | −0.026 | 0.522 | 0.244 | 0.338 | −0.040 | −0.233 |
| Rb | −0.197 | 0.048 | −0.217 | −0.005 | 0.457 | −0.030 |
| B | S.E. | Wald | Sig. | Exp(B) | 95% C.I. for EXP(B) | ||
| Lower | Upper | ||||||
| Regression Scores Factor 1 | 3.375 | 1.518 | 4.945 | 0.026 | 29.214 | 1.492 | 571.879 |
| Regression Scores Factor 2 | 10.534 | 3.868 | 7.418 | 0.006 | 37,561.068 | 19.167 | 73,6079,32.642 |
| Regression Scores Factor 3 | 4.592 | 1650 | 7.747 | 0.005 | 98.668 | 3.890 | 2502.895 |
| Cases (n = 96) | Controls (n = 35) | |||||
|---|---|---|---|---|---|---|
| N | (%) | p Value | N | (%) | p Value | |
| Sex | ||||||
| Men | 52 | 54.2 | 0.475 | 18 | 51.4 | 0.999 |
| Women | 44 | 45.8 | 17 | 48.6 | ||
| Residence Area | ||||||
| Industrial | 31 | 32.3 | 0.380 | 15 | 42.9 | 0.499 |
| Urban | 38 | 39.6 | 20 | 57.1 | ||
| Rural | 27 | 28.1 | - | - | ||
| Age (Years) | ||||||
| 40–49 | 12 | 12.5 | 0.004 | 15 | 42.8 | 0.449 |
| 50–59 | 26 | 27.1 | 11 | 31.4 | ||
| 60–69 | 27 | 28.1 | 9 | 25.7 | ||
| 70–79 | 23 | 24.0 | - | - | ||
| 80–89 | 8 | 8.3 | - | - | ||
| Smoking Habit | ||||||
| Ever | 36 | 37.5 | 0.519 | 11 | 31.4 | 0.892 |
| Ex | 27 | 28.1 | 11 | 31.4 | ||
| Never | 33 | 34.3 | 13 | 37.1 | ||
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Chrysochou, E.; Kanellopoulos, P.G.; Koukoulakis, K.G.; Sakellari, A.; Karavoltsos, S.; Minaidis, M.; Bakeas, E. Heart Failure and PAHs, OHPAHs, and Trace Elements Levels in Human Serum: Results from a Preliminary Pilot Study in Greek Population and the Possible Impact of Air Pollution. Molecules 2021, 26, 3207. https://doi.org/10.3390/molecules26113207
Chrysochou E, Kanellopoulos PG, Koukoulakis KG, Sakellari A, Karavoltsos S, Minaidis M, Bakeas E. Heart Failure and PAHs, OHPAHs, and Trace Elements Levels in Human Serum: Results from a Preliminary Pilot Study in Greek Population and the Possible Impact of Air Pollution. Molecules. 2021; 26(11):3207. https://doi.org/10.3390/molecules26113207
Chicago/Turabian StyleChrysochou, Eirini, Panagiotis Georgios Kanellopoulos, Konstantinos G. Koukoulakis, Aikaterini Sakellari, Sotirios Karavoltsos, Minas Minaidis, and Evangelos Bakeas. 2021. "Heart Failure and PAHs, OHPAHs, and Trace Elements Levels in Human Serum: Results from a Preliminary Pilot Study in Greek Population and the Possible Impact of Air Pollution" Molecules 26, no. 11: 3207. https://doi.org/10.3390/molecules26113207
APA StyleChrysochou, E., Kanellopoulos, P. G., Koukoulakis, K. G., Sakellari, A., Karavoltsos, S., Minaidis, M., & Bakeas, E. (2021). Heart Failure and PAHs, OHPAHs, and Trace Elements Levels in Human Serum: Results from a Preliminary Pilot Study in Greek Population and the Possible Impact of Air Pollution. Molecules, 26(11), 3207. https://doi.org/10.3390/molecules26113207